If a portion of the umbilical cord comes out of the cervix or vulva ahead of the fetus, this is called a prolapsed umbilical cord.
This can be a big problem for the fetus in a number of ways:
- If the umbilical vein is obstructed, but the arteries are still patent, then the fetus will continue to pump blood out to the placenta but get nothing in return. This will lead fairly rapidly to hypoxia (no fresh oxygen coming in), and hypovolemia (shock, from reduction on available blood volume).
- if the cord is totally compressed, hypoxia will develop relatively quickly, and be aggravated by the bradycardia that accompanies the obstruction of umbilical arteries.
None of this is good.

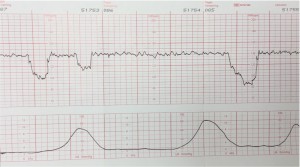
Prolapsed umbilical cords are often preceded by variable decelerations of the fetal heart rate, demonstrated on the electronic fetal monitor. Whenever these appear (and have not previously been seen), it is a good idea to examine the pelvis for evidence of a prolapsed cord. Whenever membranes rupture, check to make sure there is no sign of a prolapsed cord.
Once the cord is prolapsed, immediate delivery is the best solution.
Put the mother in the knee-chest position and use your hand in her vagina to elevate the fetal head back up into the uterus. This action may relieve enough pressure on the umbilical cord that oxygen can still get through to the baby. I wouldn’t be too reassured by feeling a normal pulse in the umbilical cord between your fingers. The umbilical vein could still be obstructed even with normal arterial pulsations.
Consider giving Terbutaline 0.25 mg SQ to stop her contractions, relieving pressure on the cord.
Transport the mother in the knee-chest position and you with your hand elevating the fetal presenting part to the cesarean section room. If, on arrival, the baby is immediately deliverable vaginally (with forceps, vacuum extractor, etc.), then that is a safe approach. If the fetus is not immediately deliverable, then proceed with cesarean section.
If the cord has stopped pulsating, then the likelihood is that the fetus has died. Cesarean section at this point will not change the long-term outcome, and vaginal delivery should usually be continued.
