A pudendal block provides excellent anesthesia to an area about the size of a dinner plate, centered on the vagina.
This block will allow for numbing the vaginal opening to allow for a less painful delivery, some introital relaxation, and satisfactory anesthesia for repair of lacerations or episiotomies.
The perineum is innervated by the pudendal nerves that originate from S3-S4, and pass close to the ischial spine as it traverses the pelvic sidewall.
The ischial spines are bony landmarks palpable to the examining finger, and located deep, lateral and a little posterior to the vagina. The spine can be felt as a distinct boney “bump” quite separate from the rest of the pelvic sidewall.
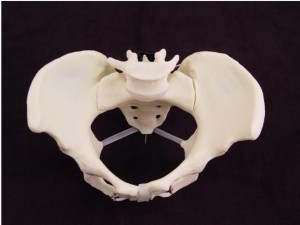
Running from the ischial spine to the sacrum is the sacrospinous ligament, a tough band of tissue that can be felt with the examining fingers. This ligament is important because the pudendal nerve runs just underneath it and next to the ischial spine.
How to give a pudendal block
The essential equipment includes and “Iowa Trumpet,” a long, hollow, blunt tube for placing at the injection site, and a matching needle, slightly longer. Pre-packaged kits typically will include both the Iowa Trumpet and the needle. Most kits will also have a plastic spacer on the needle that limits its depth of penetration to 5 mm beyond the Iowa Trumpet. This 5 mm depth of penetration is just right for a paracervical block, but is too shallow for a pudendal block. Remove the spacer to allow for a full 10 mm depth of penetration.
Open the kit and put on sterile gloves. The injection is done by feel, not by visualization. Use your right hand to examine the patient, determine the cervical dilatation, location of the fetal presenting part, and the ischial spine on the patient’s right side. Keeping two fingers of the right hand in the vagina, slide the Iowa Trumpet (without the needle) down the length of your vaginal fingers and direct it onto the sacrospinous ligament, about 1 cm from the ischial spine.

Once the trumpet is in place, slide the long needle through the Iowa Trumpet until it is fully seated within the trumpet. At this point, the tip of the needle will be extending 10 mm beyond the Iowa Trumpet and will have perforated through the sacrospinous ligament.

Aspirate to make sure you haven’t perforated a blood vessel, then slowly inject 10 cc of 1% lidocaine.
Move to the opposite side. Switch vaginal examining hands so that the left hand is in the vagina when injecting on the left side of the patient. Repeat the procedure, injecting another 10 cc.
It will take 10-20 minutes to achieve maximum anesthesia effect after the injections are complete. One-sided blocks are common and can be treated with an additional 5 cc of lidocaine to the poorly-anesthetized side.