This sexually-transmitted disease is caused by “Chlamydia trachomatis”.
It very commonly locates in the cervical canal although it can spread to the fallopian tubes where it can cause PID.
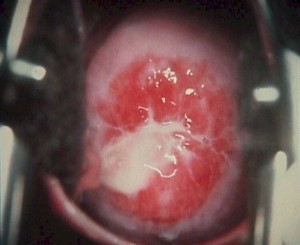
Most women harboring chlamydia will have no symptoms, but others complain of purulent vaginal discharge, deep dyspareunia, and pelvic pain. There may be no significant pelvic findings, but a friable cervix, mucopurulent cervical discharge, pain on motion of the cervix, and tenderness in the adnexa are suggestive.
The diagnosis is often made on the basis of clinical suspicion but can be confirmed with chlamydia culture. Such cultures are frequently performed routinely in high-risk populations.
Treatment*
Treating persons infected with C. trachomatis prevents adverse reproductive health complications and continued sexual transmission, and treating their sex partners can prevent reinfection and infection of other partners. Treating pregnant women usually prevents transmission of C. trachomatis to neonates during birth. Chlamydia treatment should be provided promptly for all persons testing positive for infection; treatment delays have been associated with complications (e.g., PID) in a limited proportion of women.
Recommended Regimens
- Azithromycin 1 g orally in a single dose
OR - Doxycycline 100 mg orally twice a day for 7 days
Alternative Regimens
- Erythromycin base 500 mg orally four times a day for 7 days
OR - Erythromycin ethylsuccinate 800 mg orally four times a day for 7 days
OR - Levofloxacin 500 mg orally once daily for 7 days
OR - Ofloxacin 300 mg orally twice a day for 7 days
A meta-analysis of 12 randomized clinical trials of azithromycin versus doxycycline for the treatment of urogenital chlamydial infection demonstrated that the treatments were equally efficacious, with microbial cure rates of 97% and 98%, respectively. These studies were conducted primarily in populations with urethral and cervical infection in which follow-up was encouraged, adherence to a 7-day regimen was effective, and culture or EIA (rather than the more sensitive NAAT) was used for determining microbiological outcome. More recent retrospective studies have raised concern about the efficacy of azithromycin for rectal C. trachomatis infection, however, these studies have limitations, and prospective clinical trials comparing azithromycin versus doxycycline regimens for rectal C. trachomatis infection are needed.
Although the clinical significance of oropharyngeal C. trachomatis infection is unclear and routine oropharyngeal screening for CT is not recommended, available evidence suggests oropharyngeal C. trachomatis can be sexually transmitted to genital sites; therefore, detection of C. trachomatisfrom an oropharyngeal specimen should be treated with azithromycin or doxycycline. The efficacy of alternative antimicrobial regimens in resolving oropharyngeal chlamydia remains unknown.
In a double-blinded randomized control trial, a doxycycline delayed-release 200 mg tablet administered daily for 7 days was as effective as generic doxycycline 100 mg twice daily for 7 days for treatment of urogenital C. trachomatis infection in men and women and had a lower frequency of gastrointestinal side effects. However, this regimen is more costly than those that involve multiple daily doses. Delayed-release doxycycline (Doryx) 200 mg daily for 7 days might be an alternative regimen to the doxycycline 100 mg twice daily for 7 days for treatment of urogenital C. trachomatisinfection. Erythromycin might be less efficacious than either azithromycin or doxycycline, mainly because of the frequent occurrence of gastrointestinal side effects that can lead to nonadherence with treatment. Levofloxacin and ofloxacin are effective treatment alternatives, but they are more expensive and offer no advantage in the dosage regimen. Other quinolones either are not reliably effective against chlamydial infection or have not been evaluated adequately.
Other Management Considerations
To maximize adherence with recommended therapies, onsite, directly observed single-dose therapy with azithromycin should always be available for persons for whom adherence with multiday dosing is a concern. In addition, for multidose regimens, the first dose should be dispensed on site and directly observed. To minimize disease transmission to sex partners, persons treated for chlamydia should be instructed to abstain from sexual intercourse for 7 days after single-dose therapy or until completion of a 7-day regimen and resolution of symptoms if present. To minimize risk for reinfection, patients also should be instructed to abstain from sexual intercourse until all of their sex partners are treated. Persons who receive a diagnosis of chlamydia should be tested for HIV, GC, and syphilis.
Follow-Up
Test-of-cure to detect therapeutic failure (i.e., repeat testing 3–4 weeks after completing therapy) is not advised for persons treated with the recommended or alterative regimens, unless therapeutic adherence is in question, symptoms persist, or reinfection is suspected. Moreover, the use of chlamydial NAATs at <3 weeks after completion of therapy is not recommended because the continued presence of nonviable organisms can lead to false-positive results.
A high prevalence of C. trachomatis infection has been observed in women and men who were treated for chlamydial infection during the preceding several months. Most post-treatment infections do not result from treatment failure, but rather from reinfection caused by failure of sex partners to receive treatment or the initiation of sexual activity with a new infected partner, indicating a need for improved education and treatment of sex partners. Repeat infections confer an elevated risk for PID and other complications in women. Men and women who have been treated for chlamydia should be retested approximately 3 months after treatment, regardless of whether they believe that their sex partners were treated. If retesting at 3 months is not possible, clinicians should retest whenever persons next present for medical care in the 12-month period following initial treatment.
Management of Sex Partners
Sex partners should be referred for evaluation, testing, and presumptive treatment if they had sexual contact with the partner during the 60 days preceding the patient’s onset of symptoms or chlamydia diagnosis. Although the exposure intervals defined for the identification of at-risk sex partners are based on limited data, the most recent sex partner should be evaluated and treated, even if the time of the last sexual contact was >60 days before symptom onset or diagnosis.
Among heterosexual patients, if health department partner management strategies (e.g., disease intervention specialists) are impractical or not available for persons with chlamydia and a provider is concerned that sex partners are unable to promptly access evaluation and treatment services, EPT should be considered as permitted by law (see Partner Services). Compared with standard patient referral of partners, this approach to therapy, which involves delivering the medication itself or a prescription, has been associated with decreased rates of persistent or recurrent chlamydia. Providers should also provide patients with written educational materials to give to their partner(s) about chlamydia in general, to include notification that partner(s) have been exposed and information about the importance of treatment. These materials also should inform partners about potential therapy-related allergies and adverse effects, along with symptoms suggestive of complications (e.g., testicular pain in men and pelvic or abdominal pain in women). EPT is not routinely recommended for MSM with chlamydia because of a high risk for coexisting infections (especially undiagnosed HIV) among their partners, and because data are limited regarding the effectiveness of this approach in reducing persistent or recurrent chlamydia among MSM. Having partners accompany patients when they return for treatment is another strategy that has been used to ensure partner treatment (See Partner Services). To avoid reinfection, sex partners should be instructed to abstain from sexual intercourse until they and their sex partners have been adequately treated (i.e., for 7 days after a single-dose regimen or after completion of a 7-day regimen) and have resolved any symptoms.
Special Considerations
Pregnancy
Doxycycline is contraindicated in the second and third trimesters of pregnancy. Human data suggest ofloxacin and levofloxacin present a low risk to the fetus during pregnancy, with a potential for toxicity during breastfeeding; however, data from animal studies raise concerns about cartilage damage to neonates. Thus, alternative drugs should be used to treat chlamydia in pregnancy. Clinical experience and published studies suggest that azithromycin is safe and effective. Test-of-cure to document chlamydial eradication (preferably by NAAT) 3–4 weeks after completion of therapy is recommended because severe sequelae can occur in mothers and neonates if the infection persists. In addition, all pregnant women who have chlamydial infection diagnosed should be retested 3 months after treatment. Detection of C. trachomatis infection at repeat screening during the third semester is not uncommon in adolescent and young adult women, including in those without C. trachomatis detected at the time of initial prenatal screening. Women aged <25 years and those at increased risk for chlamydia (e.g., those who have a new sex partner, more than one sex partner, a sex partner with concurrent partners, or a sex partner who has a sexually transmitted infection) should be rescreened during the third trimester to prevent maternal postnatal complications and chlamydial infection in the infant.
Recommended Regimens
- Azithromycin 1 g orally in a single dose
Alternative Regimens
- Amoxicillin 500 mg orally three times a day for 7 days
OR - Erythromycin base 500 mg orally four times a day for 7 days
OR - Erythromycin base 250 mg orally four times a day for 14 days
OR - Erythromycin ethylsuccinate 800 mg orally four times a day for 7 days
OR - Erythromycin ethylsuccinate 400 mg orally four times a day for 14 days
Because of concerns about chlamydia persistence following exposure to penicillin-class antibiotics that has been demonstrated in animal and in vitro studies, amoxicillin is now considered an alternative therapy for C. trachomatis in pregnant women. The frequent gastrointestinal side effects associated with erythromycin can result in nonadherence with these alternative regimens. The lower dose 14-day erythromycin regimens can be considered if gastrointestinal tolerance is a concern. Erythromycin estolate is contraindicated during pregnancy because of drug-related hepatotoxicity.
*CDC 2015 STD Treatment Guidelines
