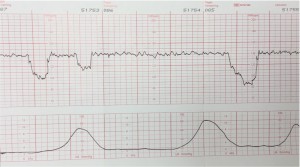
Variable decelerations are variable in onset, duration and depth.
They may occur with contractions or between contractions.
Variable decelerations must be at least 15 BPM below the baseline, and last at least 15 seconds
Typically, they have an abrupt onset and rapid recovery, in contrast to other types of decelerations which gradually slow and gradually recover.
Variable decelerations are thought to represent a vagal response to some degree of umbilical cord compression. When this happens, there is an immediate rise in fetal blood pressure.
30% of the fetal cardiac output goes to the placenta and if that flow is even partially obstructed, the fetus will rapidly develop significant hypertension. The normal fetus will respond to this hypertension by quickly slowing it’s heart, sending a signal through the vagus nerve. When the umbilical cord obstruction is released, the vagal response disappears and the fetal heart returns to normal.
Because this cord obstruction and the fetal cardiac response are brief, they have no effect on overall fetal oxygenation and acid-base balance. Variable decelerations, unlike late decelerations, are not caused by hypoxia.
But if severe enough, frequent enough and persistent enough, variable decelerations can ultimately lead to fetal acidosis. In such cases, the variable decelerations are usually accompanied by fetal tachycardia between decelerations, and ultimately loss of variability.
Interventions to treat variable decelerations may include:
- Changing maternal position to improve uterine blood flow
- IV hydration to increase maternal blood volume, presumably leading to increased uterine blood flow
- Administering oxygen to the mother to try to get some additional oxygen through to the fetus. While commonly employed, this is not particularly useful, since the maternal hemoglobin oxygen saturation is likely already 99%. The effect of breathing additional oxygen will have minimal effect on the oxygen saturation, and consequently minimal to no clinical effect on oxygen delivery to the fetus.
- Amnioinfusion to improve oligohydramnios
- Decreasing or discontinuing oxytocin infusion to slow down or stop contractions that are provoking the decelerations. Slowed contractions may not resolve the variable decelerations, but may provide enough more “recovery time” between contractions to reduce the adverse effects of the variable decelerations.
- Tocolytic drugs to slow down or stop contractions that are provoking the decelerations.
- Digital elevation of the fetal head out of the maternal pelvis to ease pressure on the umbilical cord.
- Expedited delivery of the baby
Occasional variable decelerations are common and not considered threatening. They are seen in the majority of laboring patients at some time or other. They are more common in the second stage of labor.
Severe variable decelerations dip at least 60 BPM for at least 60 seconds (“60 x 60”). If persistent and not correctable by simple means, they can be threatening to fetal well-being. Like persistent, non-remediable late decelerations during the first stage of labor, fetuses demonstrating persistent, non-remediable severe variable decelerations, particularly in the absence of variability, should be delivered promptly, preferably vaginally, but by cesarean section if necessary.
