Jaundice is a marked accumulation of serum bilirubin levels.
a. Classifications.
(1) Physiologic. Jaundice occurs after 24 hours past delivery and generally disappears seven to ten days after delivery. It is caused by the inability of the infant’s immature liver to modify bilirubin so it can be excreted from the body.
(2) Pathologic. Jaundice occurs before the baby is 24 hours of age and persists beyond seven days. It may be caused by Rh or ABO incompatibility sepsis, excessive bruising, or metabolic disorders.
b. Signs and Symptoms.
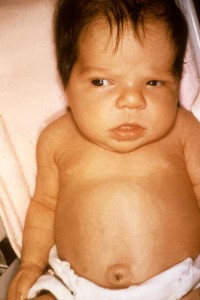
(1) Appearance. Jaundice is a yellowish appearance in the skin, sclera of the eye, or oral mucosa. The onset of jaundice is usually on the face with advancement to the trunk and extremities. Blanching the skin on a bony prominence allows for easy assessment.
NOTE: The blanch test refers to applying pressure with the thumb over a bony area for several seconds to empty all capillaries in that spot. The blanched area will look yellow before the capillaries of jaundice is present.
(2) Lethargy.
(3) Poor feeding.
(4) Dark stools.
(5) High-pitched cry and diminished or absent moro and sucking reflex – with ensuing neurologic damage.
(6) Hyperirritability, hypertonia, seizures, and opisthotonos (tetanic spasm resulting in an arched hyperextended position of the body-with advanced neurological damage).
(7) Cerebral palsy, seizure disorders, deafness, and death – with permanent neurological damage.
c. Complications.
(1) Kernicterus-a yellowish discoloration of specific areas to brain tissues by unconjugated bilirubin. This accumulation of bilirubin rises to toxic levels and is deposited in the brain causing brain damage.
(2) Nephrotoxic bilirubin-this refers to the bilirubin level in the blood being toxic and is, therefore, destructive to kidney cells.
(3) Hearing loss.
d. Treatment/Nursing Care.
(1) Early feedings. This is important to stimulated digestive processes in the intestines which are necessary to establish bacterial flora and to decrease enterohepatic circulation of bilirubin.
(2) Phototherapy. This allows for the utilization of alternate pathways for bilirubin excretion. Lights break down the pigment in the skin so that it can be excreted. The nurse must:
(a) Monitor the infant’s temperature.
(b) Apply meticulous eye care. Ensure patches are in place over the infant’s eyes.
(c) Monitor I&O, skin turgor, daily weights, and skin breakdown.
(3) Albumin. This method transports bilirubin to the liver for modification. Albumin-bound bilirubin is not able to penetrate the blood-brain barrier, which aids in the prevention of kernicterus.
(4) Exchange transfusion. This is the most direct method of eliminating bilirubin. Transfusion is generally reserved for more severe cases secondary to complications. The goal is to exchange the neonate’s blood with fresh donor blood.
(5) Observance.
(a) For appearance of an increase in jaundice.
(b) For changes in urination frequency or pigmentation.
(c) For behavioral changes.
