a. Give Frequent Explanations to the Patient.
(1) Explain to the patient what she is to expect, especially if she did not attend childbirth classes.
(2) Give simple and straightforward answers.
(3) Inform the patient of all progress. Do not give specific times for progress.
(4) Emphasize that pain diminishes between contractions. Encourage the patient to relax. Have her close her eyes and sleep.
(5) Ease panic associated with pain. Remind the patient of safety measures required for the baby and encourage concentration during the contractions.
b. Provide Comfort Measures.
(1) Ensure that there is clean and dry bedding and a clean gown.
(2) Inform the patient of frequent oral hygiene, especially after vomiting. This includes brushing the teeth and using mouthwash.
(3) Provide ice chips.
(4) Provide a cool cloth for the patient’s face, if necessary.
(5) Give back rubs or pressure, especially over the lower sacrum area.
(6) Position the patient as needed. The side lying position is recommended. Lying on the left side is preferred because it increases placental flow. Place pillows behind the patient’s back and between her legs, as necessary.
(7) Provide for a quiet room. Dim the lights if possible to encourage relaxation.
(8) Have the patient void every 2 hours; assist as needed.
c. Encourage the Use of Psychoprophylaxis.
Psychoprophylaxis refers to the mental and physical education of the parents in preparation for childbirth, with the goal of minimizing the fear and pain and promoting positive family relationships. This includes relaxation techniques and exercises learned during prepared childbirth classes.
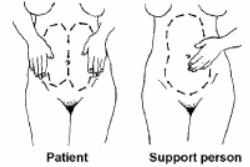
(1) Relaxation techniques include breathing during contractions, concentration on the focal point, and effleurage (see figure4-2). Effleurage is a light, rhythmic stroking techniques used during childbirth.
(2) The pelvic tilt and abdominal exercises are the exercises to be used.
d. Explain the Effects of Analgesic Medications During Labor.
(1) Fetus. What the patient in labor receives crosses the placenta and goes to the fetus. The fetus becomes sedated as a result of the medication. It may cause respiratory distress in the fetus if it is not worn off by the time of delivery. Medication is not usually given if the fetus is premature due to problems they have detoxifying the drug due to the immature system. It is, also, not usually given if the fetus is already showing signs of compromise or distress.
(2) Mother. The medication will make the patient sleepy or drowsy. It will not totally eliminate the discomfort. When given during the active phase, it may cause appropriate maternal relaxation that results in more rapid dilatation. It is not generally given during the latent phase (less than 4 cm dilatation) because it may interrupt a regular contraction pattern. It is not generally given in the transitional phase (greater than 8 cm dilatation) as delivery time cannot be predicted exactly and the infant may be born under the full impact of the medication.
(3) Labor and delivery process. Medications may slow labor down and space contractions further apart. In addition, it may speed the labor due to the relaxed state of the patient.
