a. The Uterus.
(1) Major changes in the uterus. Immediately after the placenta and membranes are delivered, the placenta site is elevated, irregular, and partially obliterated by vascular constriction and thrombosis.
In other words, the placental attachment site is sealed in order to prevent bleeding.
The uterus gradually returns to its approximate prepregnant size. This is accomplished by a decrease in the size of the individual myometrial cells and is usually accomplished by 4 to 6 weeks postpartum. The process is referred to as uterine involution. The uterine size usually increases slightly after each pregnancy.
A soft and boggy uterus, due to relaxation, requires immediate massage until it is contracted again. This is done to stop bleeding. The height of the uterus after delivery can be used to measure the process of uterine involution while the mother is hospitalized. See figure 6-1 to view the following changes of the uterus:
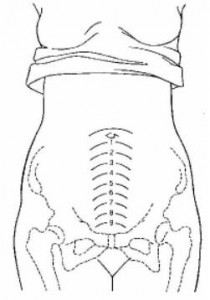
(a) Immediately after delivery- midway between the umbilicus and symphysis pubis.
(b) Twelve hours after delivery-above the umbilicus.
(c) After that – the fundus descends about one fingerbreadth every 24 hours.
(d) After the tenth day of postpartum–the uterus should not be palpable abdominally.
(2) Afterpains. Afterpains are referred to as uterine contractions which continue following delivery, but occur less frequently than during labor and have an irregular pattern. Periodic relaxations add contractions. This is common and causes the afterpains for multiparas. They may last two to three days. Breast-feeding intensifies the afterpains. This is due to oxytocin being released by the posterior pituitary in response to stimulation of the nipple. Nursing measures used to relieve afterpains are as follows:
(a) Have the mother to assume a prone position.
(b) Have the mother to place a hot water bottle on her abdomen.
(c) Have the mother to void often to keep the bladder empty.
(d) Inform the mother to drink hot liquid, this will help to ease the pain.
(e) Give analgesics per physician’s order.
b. Lochia Flow.
One of the most unique capabilities of the uterus is its ability to rid itself of the debris remaining after delivery. This process is known as lochia flow. This is the vaginal discharge during the puerperium consisting of blood, tissue, and mucous. It may last up to six weeks after delivery. It is important for the nurse, as well as the patient, to be concerned with the following facts about lochia flow:
(1) Types of lochia (in order of occurrence).
(a) Lochia rubra-a red, distinctly blood-tinged vaginal flow that follows delivery. It lasts from two to four days after delivery.
(b) Lochia serosa-a serous, pinkish brown, watery vaginal discharge that follows lochia rubra. It lasts until about the 10th day after delivery.
(c) Lochia alba-a thin, yellowish to white, vaginal discharge that follows lochia serosa on about the 10th post delivery day. It may last from the end of the third to the sixth post delivery week.
(2) Lochia with a foul-smell or a green-tinge may indicate infection.
(3) Lochia clots whereas normal menstrual flow does not.
(4) Normal lochia flow should stop within three to four weeks postpartum.
(5) An increase in lochia flow may indicate a retained placenta or a patient who is not getting enough rest.
(6) Lochia flow is slightly heavier after breast-feeding, which is due to the release of oxytocin. Oxytocin causes the uterus to contract.
c. Changes in the Cervix.
Initially, the cervix appears soft and edematous and has little tone. Multiple small lacerations may be seen. The cervix constricts rapidly and regains its shape by the end of the first week. Then, it is firm and thicker. The external os is contracted, only about one cm dilated. The cervix is healed by the fourth to sixth week after delivery. The extended os will assume a typical transverse slit of a parous woman.
d. Changes in the Vagina.
Initially, the vagina is swollen and has poor tone following vaginal delivery. It remains distensible, regains its tone and returns to its original size by the fourth to sixth week of the postpartal period. The patient can help to improve tone and contractibility of the vaginal orifice by performing the Kegel’s exercise (perineal tightening). Lacerations resulting from childbirth heal completely.
e. Changes in the Perineum.
Initially, swelling and tenderness as a result of childbearing is present. Bruising and rupture of blood vessels are usually evident. By the fourth to sixth week postpartum, the episiotomy or laceration is usually evident. There is no more swelling and tenderness in the perineum area.
