a. Hospital Admission.
After a physician or nurse has evaluated the patient, an admission order is written. At this point, your duties as a practical nurse are as follows:
(1) Establish a rapport with the patient and significant others.
(2) Explain all procedures or routines, which will be carried out prior to performing them. These include:
(a) NPO except ice chips while in labor.
(b) Activities allowed and disallowed according to ward policies (i.e. bathroom privileges).
(c) Use of fetal monitors.
(d) Progress reports.
(e) Visitation policies.
(f) Where patient’s personal belongings will be maintained.
(3) Orient the patient to the surroundings (that is, room, call bell).
(4) Initiate the patient’s labor chart.
(5) Review the information obtained originally in the exam room, verify and transfer the OB health record to the labor chart per ward policies. You will review the following information:
(a) Obstetric history.
1 Gravida/para.
2 Estimated date of confinement (EDC) or due date.
3 Duration of previous labors.
4 Problems with previous pregnancies/deliveries.
(b) General condition.
1 Rh status.
2 Allergies.
3 History of medical problems.
(c) Current pregnancy.
1 Onset of labor (contractions regular, 5 minutes or less).
2 Frequency, duration, and intensity of contractions.
3 Membranes-ruptured or intact.
4 Amount and character of show or vaginal bleeding.
5 Vital signs.
6 Rate, location of fetal heart tones.
7 Plans to bottle or breast feed.
8 Any problems with this pregnancy.
(6) Evaluate the patient’s current emotional status.
(7) Evaluate the patient’s preparation for labor through classes.
(8) Evaluate for possible danger signs.
(a) Increased pulse or temperature.
(b) Excessive vaginal bleeding.
(c) Presence of meconium (fetal feces) in the amniotic fluid of a mother with a vertex position.
(d) Alteration in fetal heart tones (FHT’s) above 160 or below 120.
(e) Obvious change in the character of uterine contractions.
(9) Perform the admission physician’s orders to include but not limited to the following:
(a) Administer and maintain intravenous fluids–per physician’s order and SOP. This is usually done on all patients.
(b) Draw lab work–CBC, serologic testing, type and screen, or per SOP.
(c) Send uterine activity (UA) which was obtained prior to admission to the lab.
b. Perineal Preparation.
Shaving of pubic hair to prevent infection of perineal episiotomy/lacerations is rarely done anymore. There must be a physician’s order to perform this task.
c. Cleansing Enema.
(1) A cleansing enema may range from “mini-” or “Fleets” to a full, soap-suds enema. Giving an enema is no longer considered routine. There must be a physician’s order to perform this task.
(2) The patient must be evaluated to determine if she has had a recent bowel movement.
(3) If a cleansing enema is given, it is usually a small fleet.
(4) Some physicians consider giving fleets to:
(a) Prevent fecal contamination of the perineum during delivery.
(b) Cleanse the bowel. This provides more room for fetal passage.
(c) Stimulate uterine contractions.
(5) Some physicians consider not giving fleets because the following factors may be present or begin:
(a) Vaginal bleeding.
(b) Premature labor.
(c) Presenting part not engaged.
(d) Abnormal presentation–breech or transverse.
(e) Already rapid moving labor.
(f) Advanced labor.
(g) Membranes are ruptured or danger of prolapsed cord.
(h) Results of enema may produce unmanageable amounts of loose stool at delivery.
d. Evaluation of Uterine Contractions.
(1) The purpose of this evaluation is to assess the ability of the uterus to dilate the cervix, help in determining the progress of labor, help to detect abnormalities of uterine contractions (such as lack of uterine relaxation), and help to evaluate any signs of fetal distress.
(2) This evaluation will help you in identifying the frequency (how often in minutes contractions occur), intensity (strength of contractions when palpitations are identified as mild, moderate, or strong [severe]), and duration (how long the contractions lasts in seconds).
(3) When palpating for contractions, place your hand over the fundal area of the patient’s uterus. Contractions can be felt by your fingers before the patient actually becomes aware of them. See figure 2-3 for patient experiencing contractions.
e. Monitoring and Recording Color and Amount of Show.
As labor progresses, the show becomes more blood-tinged. A sharp increase in the amount of bloody show coupled with frequent severe contractions may indicate labor is progressing too rapidly. Report this immediately to the Charge Nurse or physician and be prepared for possible delivery.
f. Fetal Monitoring.
(1) Fetal monitoring is done to detect presence of fetal life at time of admission and to detect development of fetal distress during labor. A fetoscope or fetal monitor may be used to obtain FHTs. Normal fetal heart rate ranges from 120 to 160 beats per minute (BPM).
The rate may increase or decrease by 30 BPM during a contraction. It should return to the baseline immediately after the contraction. A continued fetal heart rate of greater than or less than 30 BPM from the normal baseline after contractions may be indicative of fetal distress as defined by:
(a) Fetal tachycardia–FHTs sustained at greater than 160 BPM.
(b) Fetal bradycardia–FHTs sustained at less than 120 BPM.
(2) Fetal distress may be indicated by FHT’s, between contractions that are consistently abnormal. Any variations should be reported immediately.
(3) The FHTs should be checked and recorded on admission, every 15 minutes during the first stage of labor, every 5 minutes during the second stage of labor, and immediately after rupture of membranes. This helps to identify the location of the prolapsed cord.
NOTE: The prolapsed cord is referred to as the umbilical cord that protrudes beside or ahead of the presenting part of the fetus. Pressure of the presenting part on the umbilical cord can endanger fetal circulation.
(4) Fetal monitoring continued. According to the National Institute of Health (NIH), electronic fetal monitoring of the fetus is not necessary during normal labor. However, if either the mother or fetus is considered at risk, a more precise measurement of fetal response is indicated.
(5) Candidates for continuous fetal monitoring includes a patient with a multiple pregnancy, a patient with obstetric complications, a patient receiving oxytocin infusions, any high risk patient, a patient with meconium stained amniotic fluid, or any patient whose pregnancy is not progressing normally.
(6) Most medical facilities are using continuous fetal monitoring during labor. Alternative birth centers often use intermittent monitoring.
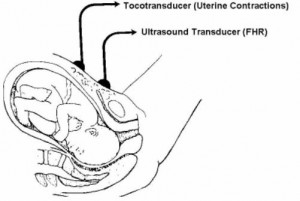
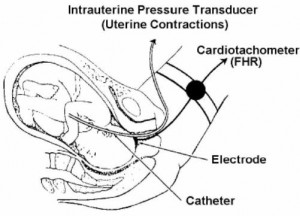
(7) Methods of fetal monitoring (see figures. 2-4 and 2-5). A transducer is placed on the abdomen over the uterus for external monitoring. An electrode is attached to the presenting part of the fetus, but NOT placed on the sutures, fontanels, face, or scrotum for internal monitoring.
g. Vital Signs. Monitor the patient’s vital signs.
(1) On admission.
(2) Every hour during early labor.
(3) Blood pressure (BP), pulse (P), and respiratory rate (R) every 30 minutes during active, transition, and the second stage of labor, to include the temperature every hour.
(4) Blood pressure, P, and R every 15 minutes while on Pitocin®, to include the temperature every hour.
(5) More frequently if complications arise.
h. Patient Given an Opportunity to Void.
You should offer the patient an opportunity to void every 2 hours during labor. The discomfort of contractions often causes the patient to be unaware that her bladder is full. A full bladder may impede the progress of labor.
i. Patient is NPO During Labor.
The patient may have ice chips to prevent drying and chapping of the lips. Vaseline may be applied to her lips to prevent chapping. Gastric emptying time is prolonged once labor is established. The administration of analgesics also prolongs gastric emptying. The patient may vomit and aspirate since her stomach contents may not be absorbed. Being unaware of when possible complications could arise could necessitate an emergency C-section with general anesthesia.
j. Positioning During Labor.
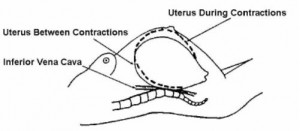
Assist the patient in turning from side to side. Elevate the head of the bed 30 degrees; this makes it easier for the patient to breathe. Try to keep the patient off her back to prevent supine hypotensive syndrome. This syndrome results in pressure of the enlarged uterus on the vena cava, reduces blood supply to the heart, decreases blood pressure, and reduces blood circulation to the uterus and across the placenta to the fetus. The patient may complain of being nauseated and feeling cool and clammy. The best position for the patient is on her left side since this increases fetal circulation.
k. Prevention of Infection.
Handwashing is essential before and after performing any procedure. Fresh, clean scrub suits should be worn in the delivery area. Unauthorized persons should not be allowed in the area. A patient with infections should be separated from other patients.
l. Vaginal Exams.
Only the physician or a trained nurse performs this exam.
It is done to evaluate cervical effacement, cervical dilatation, status of membranes, and station of presenting part. Care must be taken to perform good perineal cleansing before and after the procedure (vaginal exam). Once membranes rupture, the exam should be limited even further to prevent the risk of infection. See figure 2-6 for vaginal palpation of cervical dilatation, effacement, amniotic membranes, and presenting part.
m. Artificial Rupture of Membranes.
(1) Rupture of the membranes is done by the physician to induce or hasten labor. Apply an internal fetal monitor lead or a uterine catheter.
(2) The FHTs should be checked immediately following rupture. Determining fetal distress is secondary to compression of the cord. The cord may be displaced by the sudden “gush” of waters, which may yield a prolapsed cord.
(3) Fluids should be carefully examined for meconium if the fetus is in the vertex presentation, (that is, head first). You should check for:
(a) Slight green color–called light meconium.
(b) Green to dark color–called moderate meconium.
(c) Dark green with chucks of meconium–called heavy meconium.
(4) Record the following information:
(a) Time of the procedure (rupture of membranes).
(b) Amount of fluid expelled (small, moderate, or large).
(c) Color–clear or meconium stained (extent of staining–light, moderate, or heavy).
(d) Fetal heart rate immediately after the procedure and five minutes after the procedure.
(e) Instrument used, if other than an amnihook, to provide a slow, controlled release of fluid. Other instruments may be a fetal scalp electrode or spinal needle.
NOTE: The amnihook is used to tear a small opening in the amniotic sac.
n. Emotional Support.
(1) First phase–latent. Offer support and explanations. Instruct or reinforce breathing techniques (breathe slowly and deeply and use deep chest or abdominal breathing). Remind the patient to not push down during the first stage since it could causes cervical edema. It could also cause cervical lacerations and fetal hypoxia.
(2) Second phase–active. Continue to give support, offer encouragement, and give explanations. Include significant other in these procedures. Reinforce breathing and relaxation techniques. Accelerated shallow panting may be used, and also, effleurage (stroking movement used in massage, usually of the abdomen).
(3) Third phase–transition. Encouragement is especially important now since the patient is most likely losing control at this point. She may be nauseated or flushed and may vomit. Assist the patient to turn on her side or to sit up to prevent aspiration. Wipe her face and mouth with a cool cloth. Be aware that the patient may want to be left alone, but don’t leave; stay and support her.
Remind the patient that this is the shortest stage and that the baby will be born soon. Encourage her to concentrate on relaxation and breathing techniques. Use more intensive breathing techniques (high chest, pant-blow). Make sure to give instructions in short, simple phrases. Remind the patient that she still can’t push even though she may have a strong urge to do so.
o. Preparation of the Delivery Room.
Preparation is usually done by the paraprofessional on duty if the scrub technicians are not employed. Strict aseptic technique is maintained. The room is prepared while the patient is in the first stage of labor. The local SOP will determine how soon before anticipated delivery the room can be set up. It is usually 2 to 12 hours if the tables are covered and rooms are closed.

