a. Local.
Local anesthetics produces anesthesia only in the area where injected.
It is used in the superficial nerves of the perineum to make or repair episiotomy. Lidocaine® 1percent drug normally used and is short acting. Local anesthetics are used frequently for delivery.
b. Regional.
Regional anesthetics include paracervical block, pudendal block, saddle block (low spinal), and caudal or lumbar epidural. (See figure 4-4.)
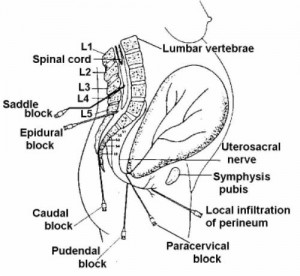
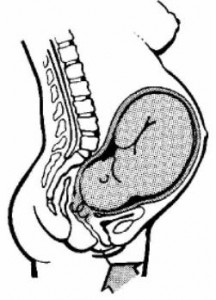
(1) Paracervical block. Paracervical block (see figures. 4-4 and 4-5) is an injection of a dilute local anesthetic into the paracervical nerve endings through the vagina. There is relief within five minutes after administration and is good for about 45 to 60 minutes. The patient doesn’t feel the cervical pain related to the uterine contractions.
When the anesthetic is injected into the tissues lateral to the cervix, it is picked up by the circulation, which quickly involves the uterus and placenta. When overdosage occurs, the fetus may exhibit bradycardia because of the quinidine-like effect of the anesthetic on the myocardium or quinidine due to a reduction in uterine blood flow. In addition, CNS medullary depression may develop and the neonate may show vascular collapse and apnea at delivery. These are potential complications and continuous fetal monitoring is required.
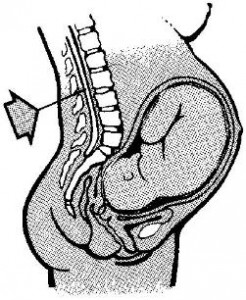
(2) Pudendal block. Pudendal block (see figures. 4-4 and 4-6) is an injection of local anesthetic on both sides of the vagina. It is administered just prior to delivery. It numbs the perineal area, vulva, and the vagina. It is used frequently in labor and delivery in combination with local anesthesia.

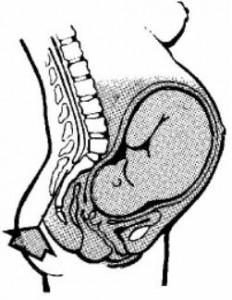
(3) Saddle block (low spinal). Saddle block (low spinal) (see figure 4-7) is an injection of anesthetic agent directly into the spinal canal below the spinal column to cause loss of sensation below the injection site. The patient has to sit up on the table with legs crossed or hanging over the side. The doctor should numb just the areas that would be touched. The saddle block numbs the abdominal and pelvic areas below the umbilicus to include the perineum, legs, and feet. It blocks the urge to push although the ability is still there. The patient will usually feel contractions. The side effects are severe maternal hypotension due to vasodilation and decreased oxygen to the fetus as a result of hypotension.
(4) Caudal or lumbal epidural.
(a) Caudal is an injection of anesthetic agent in the peridural space through the sacral hiatus (see figure 4-8). Lumbar epidural is an injection of anesthetic agent on top of the dura space through the 3rd and 4th or 5th lumbar space. These anesthetics numb the abdominal and pelvic areas below the umbilicus to the midthigh. The patient doesn’t feel contractions or perineal stretching. The urge to push may be blocked, although the ability is still present.
(b) The advantages of caudal or lumbar epidural are that they are a good pain relief, the patient is alert and cooperative, and there is decreased danger of neonatal depression.
(c) The side effects include:
1 Hypotension secondary to peripheral vasodilation.
2 If dura infusion — lower extremity sensory changes and loss of the ability to move lower extremities.
3 If blood stream infusion — ringing in the ears, lightheadedness, circumoral (around mouth) tingling, numbness, metallic taste, and seizures.
4 Burning at the site of injection.
(d) The patient should be informed about the pressure she may feel. She may have a “crazy bone” feeling in her legs, hip, or back at the time the catheter is inserted if it touches a nerve.
(e) Both the caudal and the lumbar epidural require frequent observation and a physician’s administration, which limits their use.
