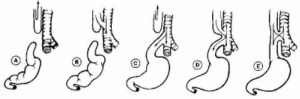
a. Tracheoesophageal fistula is a developmental anomaly characterized by an abnormal connection between the trachea and the esophagus and usually accompanies esophageal atresia (see figure 11-3).
Esophageal atresia is failure of the esophagus to form a continuous passage from the pharynx to the stomach. There are some cases of Tracheoesophageal fistula without esophageal atresia.
b. Signs and symptoms vary according to location of fistula and atresia.
(1) The infant appears to swallow normally but soon after coughs, struggles, become cyanotic, and stops breathing.
(2) Stomach distention may cause respiratory distress.
(3) Air and gastric contents may reflux through the fistula into the trachea resulting in chemical pneumonitis.
(4) If there is esophageal atresia without a fistula, as secretions fill the esophageal sac and overflow into the oropharynx, the infant develops mucus in the oropharynx and drools excessively.
(5) Repeated episodes of pneumonitis, pulmonary infection and abdominal distention may be present.
c. Diagnosis.
(1) Catheter passed through the nose meets an obstruction.
(2) Chest x-ray.
(3) Abdominal x-ray.
(4) Cinefluorography.
d. Treatment.
(1) Tracheoesophageal fistula and esophageal atresia requires surgical correction and are usually considered a surgical emergency.
(2) The type of surgical procedure and when it is performed depends on the nature of the anomaly, the patient’s general condition, and the presence of coexisting congenital defects.
e. Postoperative complications.
(1) Tracheoesophageal fistula.
(a) Recurrent fistulas.
(b) Esophageal mobility dysfunction.
(c) Esophageal stricture.
(d) Recurrent bronchitis.
(e) Pneumothorax.
(f) Failure to thrive.
(2) Esophageal atresia.
(a) Impaired esophageal motility.
(b) Hiatal hernia.
(c) Reflux esophagitis.
f. Nursing interventions.
(1) Monitor respiratory status.
(b) Perform pulmonary physiotherapy.
(c) Suction as necessary.
(2) Administer antibiotics and parenteral fluids as ordered.
(3) Accurate I&O.
(4) Observe for signs of complications (that is, pneumothorax).
(5) Maintain gastrostomy tube feedings.
(6) Give the baby a pacifier to satisfy his sucking needs but only when he can safely handle secretions.
(7) Offer the parents support and guidance and encourage bonding.
(8) Positioning before and after surgery varies with the doctor’s philosophy and the child’s anatomy.
(a) Supine with his head low to facilitate drainage.
(b) Head elevated to prevent aspiration.
