a. Definition and General Considerations. Paronychia (figure 1-2) is defined as the inflammation of the tissues around the nail.
Another name for this condition is whitlow. General conditions that are pertinent to this condition are listed below.

(1) Paronychia is most often caused by a bacterial infection, but is occasionally caused by a viral or fungal infection.
(2) This condition usually occurs around the fingernails rather than the toenails.
(3) The condition is generally painful because of the tissue tension.
(4) If untreated, paronychia can lead to abscess formations.
b. Conservative Treatment. If the condition is treated early, conservative treatment may be all that is necessary. Such treatment includes:
(1) Soaks.
(2) Zinc oxide dressing.
(3) Elevation of the hand (if a fingernail is affected).
(4) Antibiotics.
c. Indications for Incision and Drainage. Incision and drainage procedure is indicated to:
(1) Control pain.
(2) Speed healing.
(3) Prevent the spread of infection.
NOTE: The patient usually feels immediate relief as the pressure of pus is relieved.
d. Preparation for Incision and Drainage of Active Paronychia. A minimum of preparation and supplies is required. The I & D procedure can be performed painlessly through the necrotic tissue at the cuticle with a needle point scalpel or an 18 gauge needle. Gather this equipment:
(1) Syringe with 25 and 21 gauge needle.
(2) One percent lidocaine (Xylocaine®) without epinephrine for digital block.
(3) Scalpel with a #11 blade.
(4) Small scissors.
(5) Mosquito forceps.
(6) Gauze packing.
e. Procedure. Use the following procedure for the incision and drainage.
(1) Anesthesia. Use the cutaneous nerve block rather than local infiltration. The digital cutaneous nerves run along the medial and lateral aspects of each finger. These nerves can be blocked at any level above the distal phalanx. See figure 1-3.
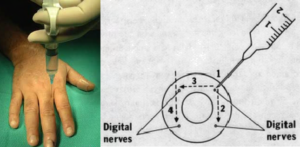
(a) Use a 25-gauge needle to raise a skin wheal by administering approximately 0.25 ml of lidocaine directly over the lateral and medial cutaneous nerve.
(b) Change to a 21-gauge needle.
(c) Advance the 21-gauge needle perpendicularly to the nerve (and the finger).
(d) Inject 1 ml of lidocaine along each nerve as indicated in figure 1-3.
(e) Slide the needle up and down on the dorsal and volar sides of the finger.
NOTE: It takes five to ten minutes for complete anesthesia to develop.
(2) Incising the inflamed tissue proximal to the nail. Use the following procedure.
(a) Using a scalpel, make an incision parallel to the axis of the finger.
(b) This incision should be an extension of the lateral and medial nail groove and deep enough to enter the abscess being treated.
(c) Using the scissors, debride any necrotic tissue.
(3) Infection under the nail. For an infection that has spread under the nail, you must remove the proximal nail in the following manner.
(a) Use mosquito forceps to lever up and hold the nail.
(b) Cut the nail off in a straight line using the scissors.
(c) Place gauze packing under the flap of the overhanging tissue and the cuticle.
(4) Culturing the infected material. To determine what caused the infection, culture the infected material you have removed from under the nail.
(5) Antibiotics. Usually drainage is sufficient to clear up the infection. Antibiotics may be considered, however.
f. Follow-up Care.
(1) Short term care. Tell the patient to elevate his hand for one to two days to prevent throbbing from the dependent position. The patient should return in two to three days for the packing to be removed. After the packing is removed, he should soak the affected finger in warm water for 15 minutes, three or four times a day. After each soaking, a dry, nonstick dressing should be applied.
(2) Long term care. The nail must be protected from being torn away from the nail bed until it regrows from its base. This regrowth process may take several months. After the healing process is complete, the nail and cuticle may be deformed.
