Needle decompression is the removal of air and fluid from the chest cavity by puncture.
a. Indications for Needle Decompression. Indications for needle depression include the following.
(1) Under combat conditions, if a casualty has unilateral chest trauma and an increase in respiratory effort, these are the only conditions needed to indicate the need for immediate chest needle decompression.
(2) Under more controlled conditions, the following signs and symptoms should be observed prior to chest needle decompression.
(a) Severe respiratory distress.
(b) Jugular vein distention.
(c) Hyper resonance on the affected side.
(d) Absent or diminished breath sounds on the affected side.
(e) Pulseless paradox (the radial pulse fades or disappears upon inspiration).
(f) Tracheal deviation may be seen, but is considered a very late and grave sign.
b. Procedure for Needle Decompression. Follow this procedure.
(1) Confirm the diagnostic need for the needle decompression procedure.
(2) Obtain a 14 gauge 3 to 3.5-inch needle.
(3) If available, give the patient supplemental oxygen. This is normal procedure for a patient in respiratory distress.
NOTE: Always provide the optimum condition the situation allows
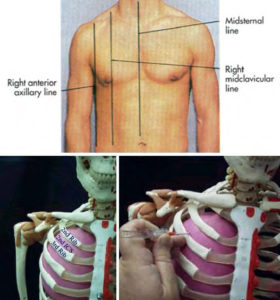
(4) Identify your site (figure 3-4). The primary site is the second intercostal space in the midclavicular line. You can alternately use the third through sixth intercostal space moving toward the anterior axillary line, making sure to stay clear of the major organs, especially on the left side of the chest.
(5) Anesthetize the area locally if time permits. Remember, this is a lifesaving emergency procedure. The patient’s airway is compromised and the chest needle decompression is the fix. Do not waste time getting the airway open.
(6) Position the patient. You may position him in an upright position if you have determined that he does not have a cervical spine fracture.
(7) Insert the thoracentesis needle into the skin. Direct the needle just over the rib into the intercostal space.
(8) Puncture the parietal pleural space.
(9) Aspirate as much air as necessary to relieve the patient’s acute symptoms.
(10) Leave the plastic catheter in place and apply a bandage or a small dressing.