An abscess is an infection that results in a collection of purulent material in a circumscribed and closed cavity.
When an abscess is in the early stages of development, it may be treated with warm compresses. If this treatment is unsuccessful, incision and drainage (I & D) may need to be performed on a wound that has abscessed.
Incision and drainage is the release of the collection of pus by making an incision in the skin and draining the pus. An I and D is commonly performed in a clinic setting. Indication of the need for an I and D is an abscess that is localized, erythematous, tender, and fluctuant.
a. General Considerations. There are few, if any, contraindications to the procedure of abscess incision and drainage. Recurrent episodes of abscess may indicate an underlying problem, such as malnutrition, poor hygiene, diabetes, or immune deficiencies. These are not considered contraindications. Additionally, follow the considerations listed below.
(1) Be sure sterile procedure is used to avoid secondary contamination.
(2) Obtain informed consent before performing an incision and drainage procedure.
b. Equipment Needed. Gather the following equipment.
(1) Sterile gloves, drapes, and surgical gowns.
(2) Antiseptic cleansing solutions such as povidone-iodine (Betadine®), 3% hydrogen peroxide, or isopropyl alcohol.
(3) Syringe containing 0.5 percent or 1 percent lidocaine (Xylocaine®).
(4) Disposable 3 ml or 10 ml syringe (depending on the size of the abscess).
(5) Disposable 25 gauge needle.
(6) One-fourth or one-half inch iodoform or plain sterile gauze packing or silverlon packing material.
(7) 4-inch by 4-inch (4×4) gauze pads for dressing.
(8) Nonallergenic adhesive tape for dressing.
(9) Hydrogen peroxide.
(10) Safety razor.
(11) Scalpel with a #11 pointed I & D blade.
(12) Hemostat (curved or straight).
(13) Plain forceps.
(14) Surgical scissors.
(15) Cotton-tipped sterile applicators.
(16) Culture swabs.
c. Preparation of Area of Abscess and Surrounding Skin. Proceed in this manner.
(1) Shave the area, if needed. Only shave the area if absolutely necessary to observe the wound.
(2) Wash the area.
(3) Prepare the area with povidone-iodine or isopropyl alcohol.
(4) Drape the area.
d. Anesthesia. Follow the procedure given below.
(1) Infiltrate 0.5 percent or 1 percent lidocaine into the incision site over the abscess.
(2) Anesthetize the area well beyond the incisional area so that drainage can occur without the hindrance of pain.
(3) Delay the incision for several minutes after the injection to be sure there is a complete anesthetic block.
e. Procedure. Use the following procedure for abscess incision and drainage.
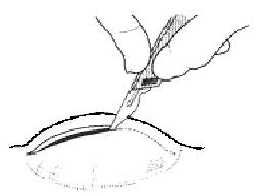
(1) Using the #11 blade, incise the abscess deeply from one side of the fluctuant area, to the opposite side of the area of fluctuance (figure 1-1). This is necessary to ensure complete evacuation of the purulent drainage.
(2) Express purulent material from wound.
(3) Obtain cultures from the drainage.
(4) Perform intra-cavity exploration to break up any adhesions. For smaller abscesses, soak a cotton-tipped applicator with hydrogen peroxide. Then, explore the cavity with the applicator to remove all pus, debris, and sebaceous materials.
(5) Following exploration, clean the cavity with four to six hydrogen peroxide soaked, cotton-tipped applicators. You may also irrigate the cavity with a sterile saline solution.
(6) Observe the incision for hemostasis. Hemostasis should occur spontaneously, but may be aided by subsequent packing.
(7) The abscess may be loosely packed using one-fourth or one-half inch iodoform or plain gauze packing. This helps in keeping the cavity open and permits adequate drainage.
(8) Apply a sterile gauze dressing and secure the dressing with nonallergenic adhesive tape.
f. Follow up Care.
(1) Initial patient education. Care the day of surgery entails advising the patient that the initial dressing should be left in place until the next day. Also tell him to elevate the affected extremity and that analgesics are seldom necessary. The day after surgery, the patient should remove the external dressing but leave the packing in place.
He should soak the site in warm water compresses or take a tub bath for 20 to 30 minutes. The site should be submerged during soaks. A sterile dressing should be reapplied after each soak.
CAUTION: If the packing falls out, DO NOT reinsert it!
(2) Follow up: health care provider. Reevaluate the patient 36 to 48 hours after the incision and drainage procedure has been done. Wound care at this point includes the following steps.
(a) Remove the external dressing.
(b) Gently remove the packing from the I & D cavity.
(c) Cleanse the abscess cavity with a cotton-tipped applicator soaked in hydrogen peroxide. Anesthesia is not necessary, but analgesics should be provided to the patient.
(d) DO NOT repack the cavity, especially if it is clean and if pain and tenderness have significantly diminished.
(e) Reapply a sterile gauze dressing to the open wound site.
(3) Follow up: patient education.
(a) Instruct the patient to continue soaks three to four times daily.
(b) Continue these soaks for five to seven days or until the incision has healed.
(c) If the abscess was adequately drained, the I & D will close spontaneously by secondary intention within five to seven days post-procedure.
NOTE: Wound healing by secondary intention depends on the size of the wound. A small puncture wound may heal in seven days. A wound that requires packing may take three weeks or longer to heal.
NOTE: Remind the patient to remove the dressing before each soaking, to pat the area dry, and to reapply the dressing.
g. Cardinal Rules for Incision and Drainage Procedure. Note the following rules.
(1) Adequate local anesthesia permits complete drainage of the abscess.
(2) The incision must encompass the entire diameter of the abscess cavity so that the cavity can be evacuated easily.
(3) Frequent postoperative warm water soaks to the abscess site hasten resolution of the inflammatory process and promote healing.