a. Definitions.
A wound is a break in the continuity of the skin, the break caused by violence or trauma to the tissue.
A wound may be open or closed. In a closed wound or bruise, the soft tissue below the skin surface is damaged, but there is no break in the skin. In an open wound, the surface of the skin is broken.
Here are some terms referring to wounds that you should become familiar with.
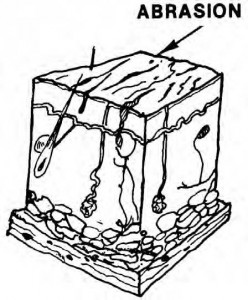
(1) Abrasion. In this type of wound, the outer layers of skin or mucous membrane are rubbed or scraped off (figure 1-1).
(2) Incised. This type of wound is cut smooth and straight. The rate of bleeding varies and there is minimal contamination. A surgeon makes this type of wound (incision).
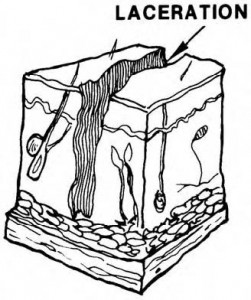
(3) Laceration. This wound is a torn, jagged cut which has gone through the skin tissues and blood vessels (figure 1-2). The wound can be made by blunt instruments such as shell fragments. Lacerations are usually very dirty.
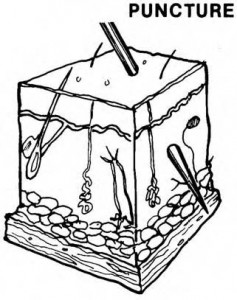
(4) Puncture. A puncture wound (figure 1-3) is made by a sharp object such as a splinter, knife, nail, or some other pointed object. These wounds bleed very little although the object may pass through nerves, bones, and organs, causing internal damage. Puncture wounds are usually very dirty.
(5) Perforating. A perforating wound is one in which there is an entrance and/or an exit. Such a wound might be made by a bullet.
(6) Mutilating. This is the term for wounds which result in disfigurement or loss of a body part.
(7) Contusion. This wound is caused by a blunt object. The damage is done to underlying tissues or organs, and the wound is closed with no broken skin (figure 1-4).
b. Wound Healing.
Wound healing is a complicated process. A wound is a break in the continuity of tissue. The body must have a special procedure to take care of the skin injury and dead tissue. The injured area must be able to signal distress, and there must be some way to get rid of the dead cells and replace them with new cells. The process of wound healing is a way of restoring living tissue so that the entire body is covered with skin.
(1) The body’s first response to cell damage is inflammation. The reaction is similar regardless of the cause–cut, burn, bruise, or pinch. The injury starts a reaction which may be the release from the dead or injured cells of one of their substances such as histamine. The released substances affect the capillaries. The capillaries dilate, widely increasing the blood supply that they can bring to the injured
area. If the injury takes place in the skin or in the tissue close to the skin, the increased amount of blood in that area causes the area to look red. Because the injured area has a greater blood supply than the surrounding area, the wound site is warm to the touch.
(2) As the capillaries dilate, the “mesh” of their walls also is opened.
Normally, capillary walls allow water and electrolytes to pass through, but now these walls also permit extra fluid and some protein plasma to escape. This extra fluid in tissue spaces produces swelling. Because the fluid is extra, the patient feels discomfort and a throbbing sensation. Sometimes just the swelling is enough to stimulate the pain receptors. The changes in the blood vessels are responsible for the basic symptoms of inflammation: swelling, pain, redness, and heat.
(3) One of the substances released by injured cells attracts leukocytes. Leukocytes pass through capillary walls into damaged tissues. In an injury with extensive tissue damage, large amounts of the substance which attracts leukocytes are released. This substance may be absorbed and circulated in the blood stimulating the production of more white cells. If a blood count is taken at this time, there will be an increase above normal in the number of white cells (leukocytosis).
(4) Inflammation is sometimes accompanied by fever. It is not clear how inflammation influences the body’s temperature-regulating center. It is possible that a substance absorbed from the injured cells is the signal that stimulates the response of fever.
(5) Although the effects of inflammation are uncomfortable, they may actually prove beneficial. Protein escapes into damaged tissue and forms a gelatin type substance; this substance keeps materials from moving out of the wound site into the rest of the body. The patient experiences swelling and pain, both of which encourage
him to be rather quiet and rest the injured area. This keeps infection in the injured area from spreading to other parts of the body. Bacteria, or a substance such as a foreign
chemical, could harm other tissues if spread by activity to other parts of the body.
(6) Signs and symptoms of inflammation are so easy to see that
inflammation attracts a great deal of attention. A doctor relies on inflammation to help locate and identify the place and type of body injury. It is possible to decide whether the body is overcoming the problem or needs additional help by watching the sequence of
inflammation symptoms.
c. Complications.
Wound complication refers to anything abnormal in the healing process. The term also refers to the loss of function of a body organ, the function loss caused by the initial wound. Infection is the single most common wound complication. Other complications of wound healing include continued bleeding, dying tissue, and improper healing.
(1) Continued bleeding. Bleeding must be stopped to allow the healing process to proceed.
(2) Dying tissue. Tissues at the site of severe injuries may have been
severely damaged by being deprived of their blood supply with its oxygen and nutrients. These tissues will die and must be removed or carried away in the capillaries for healing to take place properly.
(3) Results of improper healing.
(a) A keloid is excessive scar tissue growth. It can appear in an area of injury, looking like a smooth overgrowth of fibroblastic tissues (tissues composed of spindle-shaped cells). Keloids occur primarily in dark-skinned people, but given the proper conditions, anyone can develop a keloid. Keloids can be removed surgically for cosmetic reasons.
(b) A localized infection in which there is an accumulation of pus is an abscess. Pus is a liquid accumulation of phagocytes (also called leukocytes). An abscess is caused by an infecting microorganism. The particular microorganism determines whether the pus is white, yellow, pink, or green.
(c) Inflammation of the cellular tissue surrounding the wound is
cellulitis.
(d) If pus collects in an already existing cavity such as the gallbladder or lung, the term used is empyema.
(e) A fistula is an abnormal passage between two internal organs. A wound that heals improperly can cause this passage.
d. Anemia.
In anemia, hemoglobin levels are lower resulting in tissue hypoxia (abnormally low amount of oxygen in the body tissues). This changes collagen synthesis and epithelialization, both functions in the healing process. The body compensates by increasing blood circulation in a person with mild anemia. If the volume percentage of red blood cells in the whole blood drops below 20 percent, the lower oxygen tension in the tissues can disrupt local metabolism for cell regeneration.
e. Immunosuppression.
When a wound to the body occurs, inflammation is the immediate response. Body tissue around the wound becomes red, swollen, a little hot, sometimes painful, and sometimes there is a loss of function in that body part. Immuno-suppression is a change, in a negative way, of the body’s response to a foreign substance. The body produces fewer, poorer quality leukocytes (white blood cells), fewer immunoglobulins (proteins functioning as specific antibodies), or a lesser ability for collagen synthesis. All of these are necessary for tissue repair.
f. Foreign Body in the Wound.
A foreign body in a wound serves as a focal point for infecting microbes or preventing tissue granulation (formation of small, fleshy masses on the surface of a healing wound). Heart pacemakers and artificial legs, for example, are necessary but also qualify as foreign objects that can harbor microorganisms and cause infection. Sutures (stitches used in surgery to unite two surfaces) also qualify as foreign substance and can be the source of infection. Sutures that are too tight can also cause a wound to heal improperly. The sutures can disrupt the collagen network, compromising the tensile strength. After the scab shrinks, the final scar is wider than normal.
g. Blood Supply.
Since blood supplies the products used in healing, any factor which restricts blood circulation to a wound area interferes with healing. Dead or edematous tissue, restrictive bandages, and damaged arteries can all slow the healing process.