a. Good Nutrition. Good nutrition during pregnancy is essential for:
(1) The well-being of the mother and the developing fetus.
(2) Development of effective uterine musculature.
(3) Development of breast tissue.
(4) Development of an adequate functioning placenta. Poorly nourished mothers have placentas with fewer and smaller cells. Also, poorly developed placentas have a reduced ability to synthesize substances needed by the fetus, to facilitate the flow of needed nutrients, and to inhibit passage of potentially harmful substances.
(5) Development of infant’s weight, length, bones, and brain. A nutritionally deprived fetus may have decreased development of brain cells. If optimum nutrition is provided after birth, the effects on the brain may be reversible.
(6) Continued development of the infant after birth.
b. Chronic Malnutrition. This has been shown to be related to reproduction problems (this includes difficulties during pregnancy, labor, and delivery), increased perinatal mortality, low birth weight, and other problems with the newborn.
c. Nutritional Risk Factors in Pregnancy that Require Observation.
(1) Risk factors at the onset of pregnancy.
(a) Adolescence. Many adolescents are nutritionally at risk due to a variety of complex and interrelated emotions and social and economic factors that may adversely affect dietary intake. Their nutritional needs are greater and pose much concern from nurses and physicians.
(b) Frequent pregnancies. These pregnancies may have depleted nutrient stores. This situation can compromise maternal and fetal health and well-being.
(c) Poor reproductive history. Previous poor weight gain, pregnancy-induced hypertension (PIH), previous stillbirth or small for gestational age (SGA) baby, premature delivery, and prenatal infection are all common in women who are or have been poorly nourished in the past. These women may need more than the usual nutrition guidance.
(d) Economic deprivation. This refers to the pregnant patient who is not able to afford proper food. There are several programs that help with the purchase of food or that offer supplements.
(e) Bizarre food patterns. This includes faddish diets. A woman may enter pregnancy either having or continuing to be on a faddish or otherwise nutritionally inadequate diet.
(f) Vegetarian diets. This diet may not contain any or enough protein or vitamins for a developing fetus. Intense nutritional counseling will be required to work out a diet pattern during the prenatal period.
(g) Smoking, drug addiction, and alcoholism. Physiologic problems may have been present. Pregnant patients who indulge in this category may have major physiologic problems. There is the possibility that the patient may not consume sufficient quantities of nutritious foods and, in addition, can cause major problems to the fetus.
(h) Chronic systemic disease. There may have been medical problems, which may have interfered with ingestion, absorption, or utilization of nutrients. Drugs used to treat these conditions may also affect nutrition by similar interference. Counseling should include general nutrition guidelines for prenatal care and diet therapy.
(i) Pre-pregnant weight. This may be at risk if the patient is fifteen percent or more below or twenty percent or more above the standard weight for health.
(2) Risk factors identified during pregnancy.
(a) Anemia of pregnancy. Many pregnant patients have a lack of iron stores large enough to meet the needs of pregnancy.
(b) Pregnancy-induced hypertension (PIH). This may be seen in more patients with poor diets. However, there is no definite documentation of PIH’s relationship to the diet.
(c) Inadequate weight gain. This may be an indication of maternal and fetal malnutrition (intrauterine growth retardation (IUGR)). It is important to document the pattern of weight gain in pregnancy as well as the total amount of weight gained.
(d) Excessive weight gain. This may be due to fluid retention. However, the pregnant woman should be carefully assessed for PIH.
d. Caloric Requirements of Pregnancy.
(1) Daily caloric requirements for a pregnant woman are about 300 more than their normal requirements of 2300 to 2700 calories. The exact requirements are dependent on the patient’s age, multiple birth, and the patient’s activity. Calories should be selected for quality rather than quantity. “Empty calories” do not count.
(2) Pregnancy is not the time to correct weight problems. Maintenance of a minimum of 1500 calories a day is essential for fetal development throughout the pregnancy. Patients who gain extra weight the first seven months then decide to cut back so as not to go overweight deprive the fetus of:
(a) Nutrients necessary when the fetal brain cells are growing the fastest.
(b) Nutrients necessary when the protective layer of fat is being developed.
(3) Foods rich in protein, iron, and essential nutrients are recommended to be eaten on a daily basis. During the first two trimesters of pregnancy, iron is transferred to the fetus in moderate amounts, but during the last trimester when the fetus builds its reserve, the amount transferred is accelerated ten times.
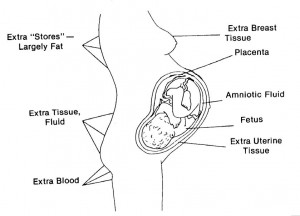
(4) Recommended weight gain for a normal pregnancy is 24 to 30 pounds.
See figure 9-1 for the distribution of weight gained after 40 weeks of pregnancy.
e. Menu planning. A diet consisting of a variety of foods can supply needed nutrients. The increased quantities of essential nutrients needed during the pregnancy may be met by skillful planning around the basic four food groups. The recommended daily intake from the basic four food groups are as follows:
(1) Milk group-32 oz or 1000 ml per day.
(2) Meat group-4 servings per day to include:
(a) Beef, veal, pork, poultry, or fish.
(b) Eggs each day.
(c) Liver once a week.
(3) Vegetable and fruit group.
(a) 2 servings daily of dark green or yellow vegetables.
(b) 2 servings daily of fruit.
(4) Bread and cereal group-4 servings per day.
