a. Blood Volume.
(1) Blood volume increases gradually by 30 to 50 percent (1500 ml to 3 units). This results in decrease concentration of red blood cells and hemoglobin. This explains why the need for iron is so important during pregnancy.
(2) By the time pregnancy reaches term, the body has usually compensated for the decrease resulting in an essentially normal blood count.

(3) Blood count is interpreted as anemia by the physician if the hemoglobin falls below 10.5 grams per 100 ml and the hematocrit drops below 30 percent.
(4) Increased blood volume compensates for hypertrophied vascular system of enlarged uterus. It improves the placental performance. Blood lost during delivery, less than 500 cc is normal (300 to 400 cc is average).
b. Cardiac Output.
(1) Cardiac output increases about 30 percent during the first and second trimester to accommodate for hypervolemia. This is not a problem for patients with a normal heart. A patient with a diseased heart is especially at risk for cardiac decompensation 28 to 35 weeks of pregnancy when the blood volume and cardiac load are at their peak; also, during labor and immediately after delivery when rapid hemodynamic changes occur.
(2) Change in output is reflected in the heart rate. It usually increases by 10 beats per minute.
(3) Nursing implication. Patients with a diseased heart need to be advised to get plenty of rest and to report any shortness of breath or unusual symptoms to their physician.
c. Blood Pressure.
(1) Normally, the patient’s blood pressure will not rise.
(2) Nursing implications.
(a) The patient’s blood pressure should be checked carefully and often since a significant increase is one of the indicators of toxemia of pregnancy.
(b) When monitoring the blood pressure, be sure it is done under the same circumstances (that is, patient sitting and left arm).
d. Venous Return.
(1) The lower extremities are often hampered in the last months of pregnancy due to the expanding uterus restricting physical movement and interfering with the return of blood flow. This results in swelling of the feet and legs.
(2) Nursing implications.
(a) Advise the patient to rest frequently. This will improve venous return and decrease edema.
(b) Have the patient to elevate her feet and legs while sitting.
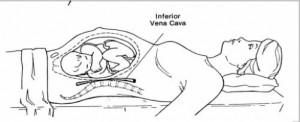
(c) Remind the patient not to lie in a supine position since this inhibits return blood flood flow as the heavy uterus presses on the vessels. This leads to the vena cava syndrome (see figure 5-2) or supine hypotension. The patient may complain of feeling dizzy, nauseated, or weak.