a. General Information. Junctional arrhythmias create an inverted P wave because the atria are depolarized by the retrograde conduction.
These abnormal conditions will depolarize the ventricles in the normal manner (normal QRS). An inverted P wave can occur before, during, or after the QRS complex. All junctional rhythms will create an inverted P wave, but some low atrial impulses can also cause inverted P waves.
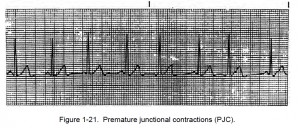
b. Premature Junctional Contraction. Analysis of premature junctional contraction (PJC) is given below and an example is shown in figure 1-21.
(1) Premature junctional contraction is another form of heart abnormality. This condition occurs when a small region of the heart becomes more excitable than normal. This causes an occasional abnormal impulse to be generated between the normal impulses. The abnormal impulse is generated from the region of the heart called the ectopic focus. A wave of depolarization spreads out from the ectopic focus and causes a premature contraction. The regularity depends on the regularity of the underlying rhythm and the rate depends on the rate of the underlying rhythm.
(2) P waves will be inverted and can fall before, during, or after the QRS complex.
(3) The PR interval can only be measured if the P wave precedes the QRS Complex.
(4) The QRS complex lasts less than 0.12 of a second. What happens is that the AV node takes over the pacemaking function.
NOTE: The normal inherent rate of atrial ventricular junction is 40 to 60 beats per minute. If higher pacemaker sites fail, a junctional escape pacemaker might take control of the heart. The rhythm would then be called a junctional escape rhythm. Inherent rates are as follows: atria–75 beats/minute; AV node — 60 beats/minute; ventricles–40 to 60 beats per minute; and normal heart rate — 60 to 100 beats per minute.