When taking a patient’s breathing (ventilation) rate, you should note his breathing rate, the depth and rhythm of his ventilations, the quality of his ventilations, and any factor (such as coughing) that is not normal.
Breathing should be effortless and barely noticeable. If it is labored or noisy, too fast, or too slow, then it is not normal and should be treated aggressively.
a. Rate.
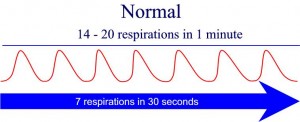
A normal adult will breathe at a steady rate. A breathing rate from 12 to 20 breaths per minute is normal. Children have a normal breathing rate of 20 to 28 breaths per minute. Infants have a normal range of 30 to 60 breaths per minute.
(1) Normal. A patient’s breathing rate is said to be normal if it is within the appropriate range. For example, a breathing rate of 26 is normal for a young child, slow for an infant, and rapid for an adult.
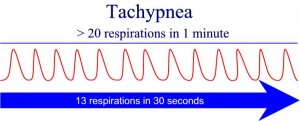
(2) Rapid. If a patient’s breathing rate is higher than the normal range, then his breathing is rapid. Rapid breathing is also known as hyperventilation.
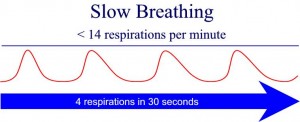
(3) Slow. If a patient’s breathing rate is below the normal range, his breathing is slow.
b. Depth.
The depth of ventilation refers to the amount of air that is inhaled and exhaled. The amount of air inhaled and exhaled in one cycle is called the tidal volume. The more the chest cavity expands, the greater the depth of the ventilation. Full expansion of the chest wall with full relaxation on exhalation is a good indicator of adequate depth of breathing and adequate tidal volume.
Many books will try and apply numbers in milliliters per breath to calculate tidal volume. This is not possible to measure in the field, so it is important to asses the expansion of the chest to help determine tidal volume.
(1) Normal. Normal depth of breathing is hard to determine. The chest will not expand to its full capacity with each breath. If a patient is not showing signs of distress, is alert, and has a normal skin color, then you can gauge that the breathing depth is normal and adequate for his condition. Airflow of about 500 ml each breath is normal in an adult.
(2) Shallow. If a patient’s chest and abdomen rise and fall only slightly, the patient’s breathing is shallow. A patient with shallow breathing will probably breathe at a rapid rate. If a patient has a pattern of rapid, shallow breathing, he is said to be “short of breath.” Rapid and shallow breathing will not get a high enough tidal volume to allow the air to reach the lungs for good oxygenation. A pattern of slow, shallow breathing is called “hypoventilation.”
(3) Deep. A patient’s breathing is deep when the chest cavity expands to almost its full capacity. A person who is gasping for air expands his chest to its full capacity. A breathing pattern of rapid, deep breathing is called “hyperventilation.”
c. Rhythm.
The rhythm includes the entire breathing (inhalation and exhalation) cycle.
(1) Regular. The normal breathing rhythm (pattern) is: inhalation, pause, exhalation, pause. The exhalation phase of the cycle usually lasts about twice as long as the inhalation phase. The cycles are repeated at a steady pace.
(2) Irregular. A change from the normal breathing pattern is an irregular pattern. An irregular breathing pattern may indicate the presence of illness. It is not unusual for painful breathing to be associated with an irregular breathing pattern. Some irregular patterns are given below.
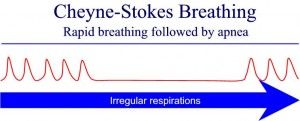
(a) Cheyne-Stokes. Cheyne-Stokes breathing is a pattern in which the breathing increases and decreases in depth with regularly recurring periods when the patient does not breathe at all. Cheyne-Stokes breathing is usually associated with severe head trauma that interrupts the breathing center in the brain, causing the irregular breathing pattern. It can also be seen in acute mountain sickness as the body tries to compensate for the lower oxygen levels at higher altitudes.
(b) Kussmaul. Kussmaul breathing pattern is a compensatory mechanism that is often seen in diabetic patients. This breathing pattern is very deep and rapid as the body attempts to lower the acid levels that are created in diabetic ketoacidosis. It is also associated with crush syndrome (renal failure following the crushing of a large muscle mass).
(c) Agonal. Agonal breathing is the body’s last attempts to save itself. The patterns of occasional gasping breaths that can often occur after the heart has stopped are not effective in moving air. This is a primal reflex that is seen as a patient dies.
d. Quality.
Breathing can be of normal or abnormal quality.
(1) Normal. Normal breathing does not require conscious effort. It is automatic, regular, and even. It produces no noise, discomfort, or pain.
(2) Abnormal. Breathing that is not normal is abnormal.
(a) Pain. Injuries to the chest and certain diseases can cause pain when breathing.
(b) Labored breathing. Labored breathing occurs when the person is trying to get as much air into his lungs as possible. It is also called “air hunger” and “dyspnea.” Labored breathing is normal when due to vigorous work or athletic activity.
(c) Wheezing. Wheezing is difficult breathing accompanied by whistling sounds on exhalation. Wheezing often occurs in patients with asthma (difficulty in breathing caused by spasms in the bronchial tubes and excessive mucous production) and emphysema (a condition caused by damaged lung tissue).
(d) Noise. Sounds such as rattling or bubbling sounds indicate breathing problems.
(e) Stridor. Stridor is a high-pitched whistling sound, usually with inhalation. Stridor is a serious sign that indicates an upper airway obstruction.
e. Unusual Position.
Sometimes a patient will position himself in order to make breathing easier. For example, a patient may lean forward and brace his arms against his knees or the bed in order to breathe more normally. This is known as the tripod position and should be noted during your assessment.
f. Coughing.
A cough is a sudden and noisy expulsion of air from the lungs. It is usually produced to remove secretions and foreign matter (dust, smoke, sprays, and so forth) from the lungs. A cough can be acute or chronic, productive or nonproductive.
(1) Acute. An acute cough is a cough that came on suddenly.
(2) Chronic. A chronic cough is a cough that has existed for a long time (not acute).
(3) Productive. A productive cough is a cough accompanied by sputum expelled from the lungs.
(4) Nonproductive. A nonproductive cough does not contain sputum. It is also called a dry cough.
g. Sputum.
Sputum is mucous material that is expelled (coughed up) from the lungs. It is not saliva. Saliva is produced by the salivary glands in the mouth to keep the mouth moist and to help in the chewing and swallowing of food. If the patient’s cough is productive, note the amount, color, character, and odor of the sputum.
(1) Amount. The amount may be scant, moderate, or copious.
(a) Scant. Scant means a small amount.
(b) Copious. Copious means a large amount.
(c) Moderate. A moderate amount is more than scant but less than copious.
(2) Color. Normal sputum is clear. Abnormal sputum, such as caused by a lung disease, may be green, yellow, reddish or pinkish (mixed with blood), or gray.
(3) Character. Sputum may be watery, semi-liquid, viscous, or frothy.
(a) Watery. Watery sputum is thin and usually colorless.
(b) Viscous. Viscous sputum is very thick, firm, and stays together.
(c) Semi-liquid. The normal thickness of sputum is semi-liquid. It is thicker than watery sputum but not as thick as viscous sputum.
(d) Frothy. Frothy sputum is foam-like and contains many small air bubbles.
(4) Odor. Normal sputum has little or no odor. Abnormal sputum may have a sweaty smell or a foul and offensive smell.