|
Sexual Assault
Outline · Serious Injuries
· Notification · Chaperone · Consent
· Gather Supplies · Labels
· Requisitions · History
· Clothing · Photographs
· Combings · Mouth Exam
· Hands · Change of Clothing
· Tests · Antibiotics
· Contraception · Follow-up
· Evidence Disposition · Patient Instructions
· Children · Military
Settings
Sexual assault is any sexual act performed by one person on another person without that
person's consent.
The incidence of sexual assault is not known. Published statistics only
encompass reported sexual assault. In some cases:
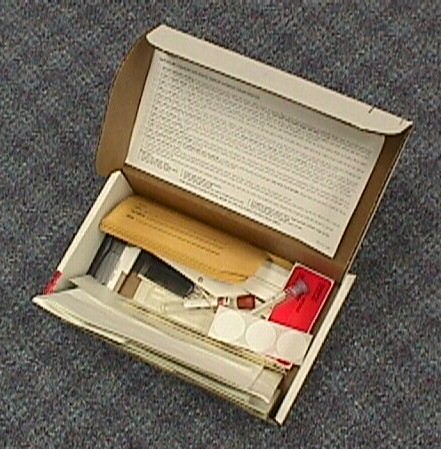
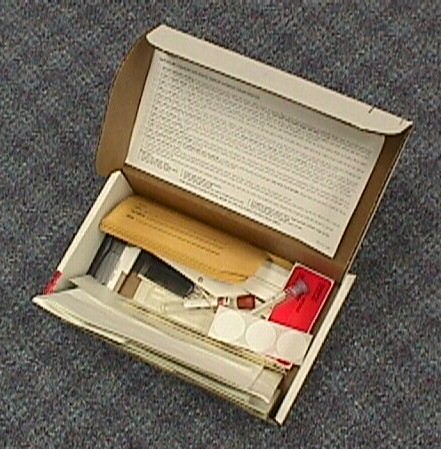
Prepackaged Sexual Assault Kit |
-
The victim is unwilling to notify authorities or seek medical attention
for fear of personal humiliation.
-
The victim is unwilling to notify authorities because she fears
retribution.
-
The victim, particularly in cases of incest or close personal
relationships, does not wish to disturb the family or friendship unit,
dysfunctional though it may be.
-
The victim is not aware that the crime occurred. (eg, when illegal drugs
or alcohol are involved)
Sexual assault is usually not a crime of sexual gratification, but rather
expresses power, anger, hostility or aggression.
Although the stereotypical perpetrator of sexual assault is a stranger, in
real life, the rapist is often known to the victim. This situation is known as
"acquaintance rape" or, when applicable, "date rape."
Sexual assault is an act of violence with medical, mental and legal
issues which should to be addressed. Described below is a standard medical
approach to sexual assault when resources are available and clinical
circumstances allow.
Outline of Management
-
Evaluate the patient for serious injuries (fractures, hemorrhage, etc.) which might
require immediate treatment.
-
Obtain a brief history, explaining to the patient what will occur next. Obtain patient's
consent.
-
Gather all necessary materials and notify legal and administrative authorities.
-
Examine the patient, obtaining various specimens.
-
Offer treatment for STDs, pregnancy.
-
Arrange for follow-up care.
Serious injuries come first
If the patient has serious injuries, take care of the injuries before worrying about
collecting legal evidence. Patient care takes priority.
Notify Legal and Administrative Authorities
Early in this process, legal and administrative authorities need to be
notified that a sexual assault has been reported and medical care is being
provided. Depending on your location, this might include local, county, state or
federal law enforcement agencies.
Notify Social Services
In some settings, a sexual assault counseling service is functioning and can
be contacted. In other settings, social workers or other support personnel are
used for this purpose. Sometimes, a chaplain serves the role of a social service
provider and should be notified of this occurrence.
Chaperone
Customs vary regarding the use of a chaperone in general OB-GYN practice,
but they don't vary at all in the context of a sexual assault victim. It is
important to have a medical chaperone (preferably someone from the nursing
community) who can be a witness, both to the history-taking and the physical
exam. This person can also provide valuable comforting and support to the
victim.
Materials Needed
-
Authorization (consent) forms for examination, medical treatment, collection of
specimens, release of information to proper authorities, and, if indicated, photography.
-
Laboratory requisition forms:
-
Pregnancy test (HCG)
-
VDRL or RPR
-
HIV
-
Hepatitis B
-
3 gonorrhea cultures
-
1 chlamydia test
-
9 Paper envelopes
-
2 Combs, new and unused
-
1 Tongue blade
-
6 twin-packs of cotton-tipped applicators, sterile
-
1 Flashlight
-
5 ml of distilled or sterile water (not saline)
-
3 glass microscope slides with the frosted ends labeled in pencil with the patient's
last name and SSN
-
3 Slide holders (cardboard, not plastic). If only plastic are available, use them, but
don't seal the ends...use cellophane tape to partially cover the end, allowing air to
circulate freely, but disallowing the glass slide to fall out.
-
25 Labels, with name, SSN, date, identity, location, initials
-
2 pieces of filter paper
-
2 Red-top blood tubes
-
2 wooden toothpicks
-
1 vaginal speculum
-
1 pair of latex examination gloves
-
Lubricating jelly (such as KY or Surgilube)
-
2 pieces of plain white paper, 8.5" x 11"
-
3 Chocolate Agar plates
-
1 Chlamydia test kit
-
Fresh clothing for the patient
-
Mouthwash and cup
-
Toothbrush and toothpaste
-
Betadine douche (mix small amount of Betadine with 100 ml water and load in a 30-50 ml
syringe)
-
Emesis basin or similar small basin
-
Camera and color negative film for taking photographs of traumatized areas, if indicated.
|
Gather your supplies before starting your exam
Before you actually examine the patient and begin collecting your exam specimens, it is
best to gather all the materials you will need first. This saves you time and spares the
patient the unpleasantness of a prolonged examination. It also helps you avoid forgetting
something. If you think you have completed your exam, but you still have some supplies
left, you probably forgot about something.
In many areas, "Sexual Assault Investigation Kits" are prepared in advance,
containing everything needed for this examination. If a pre-packaged kit is not available,
you may wish to consider making your own prior to the need for it arising. All specimens
should be properly labeled and maintained by precise chain of custody.
Labels
Every specimen taken from the patient must be properly labeled. The label should
include:
-
Patient's name
-
SSN
-
Date
-
Time
-
Identity of specimen (e.g., "fingernail scrapings)
-
Location (e.g., "right hand")
-
Examiner's initials
It is helpful to make up your labels before you examine the patient. In addition
to labels for all of the specimens, you will need to label lab requisitions, your medical
report, and the consent forms. You will need at least 25 labels, not counting any labels
used on laboratory requisitions.
Consent
Consent should be obtained from the patient to:
-
Examine her and provide medical treatment.
-
Collect evidence.
-
Taking photographs (if indicated).
-
Release medical reports and evidence to legal authority.
History
There may be a balance between obtaining enough information to effectively
treat the patient and asking questions that make the patient uncomfortable.
While some assault victims are anxious to discuss what just happened to them,
many more are silent and withdrawn, exhausted from their experience.
Ask the patient what happened. Ideally, she will need to be as specific as possible
about exactly what was done to her, when, where, by whom, etc.
Write down her description of what happened, but remember
that you are not in a position to judge whether a rape or sexual assault occurred...you
are simply repeating what the patient told you. For example, you might say, "Patient
states she was raped today at 4:00 pm by an unknown person in Municipal
Park."
You
should not write, "The patient was raped at 4:00 pm," because that implies a legal
conclusion on your part. You should also not say, "The patient was allegedly raped at
4:00 pm," because this use of the word "allegedly" has been interpreted by
some people to imply that you didn't believe that a rape occurred. It is better to simply
condense and repeat what the patient told you.
Gynecologic History
Particularly important are:
-
LMP
-
Use of contraceptives, such as BCPs
-
Any significant past gynecologic history
-
Sexual history: You need not obtain a detailed sexual history, but two issues are
important to explore with the patient: first, whether she has ever had sexual intercourse
prior to the sexual assault, and second, the last time sexual relations occurred within
72 hours prior to the assault.
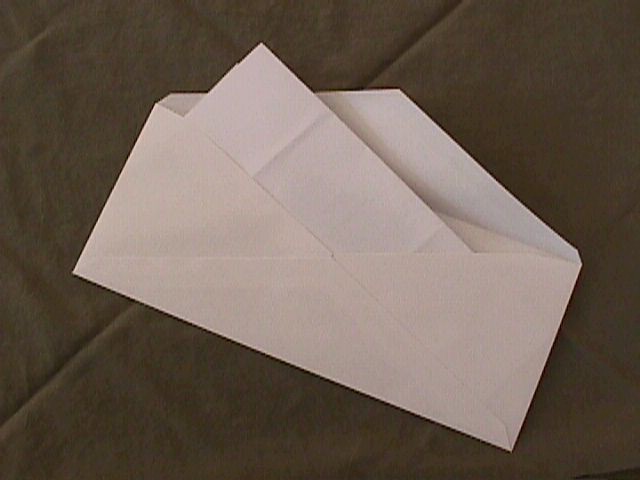
Clothing
If any clothing contains moist or dry stains, remove the clothing, let it dry
completely, and place it in a paper bag (not plastic).
-
Use one paper bag for each piece of clothing.
-
Seal each bag and label it.
-
The clothing should be given to the law enforcement authorities and signed out using a
chain of custody form.
-
Give the patient a property receipt card for her clothing.
Physical Exam
Start at the patient's head and work downward, explaining to her what you are doing as
you examine her and collect specimens. If you encounter any physical evidence of trauma,
you should draw a picture of your findings and, if possible, photograph the evidence.
Photographs
Take the photographs yourself, without a photographer being present,
particularly if the trauma involves areas around the breasts or perineum.

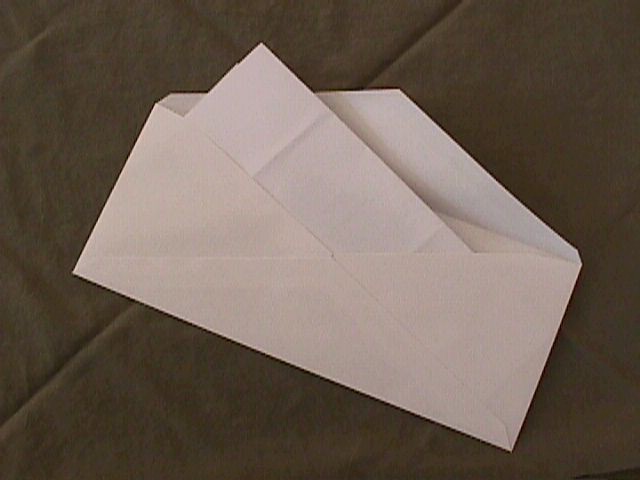
Collect head combings over a white paper.
Fold the paper and seal it in an envelope
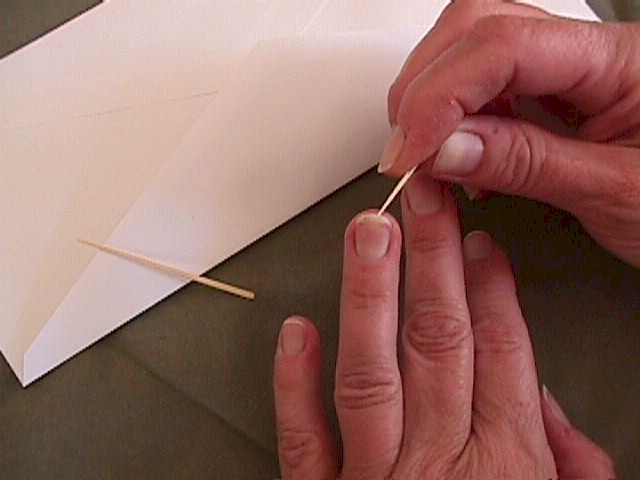
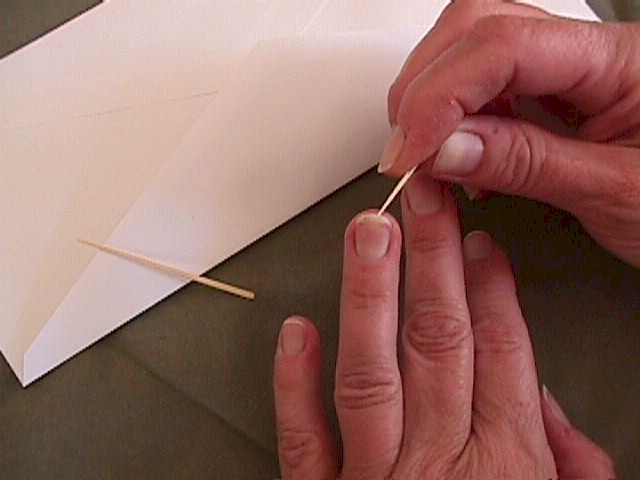
Collect fingernail scrapings with
toothpicks, and seal them in an envelope.

Inspect the Vulva |
Head Combings
Lightly comb the patient's hair over a plain white sheet of paper. Fold the paper over
the comb and any loose hairs and place everything in an envelope. Seal and label it.
Do not pluck hairs from the head to serve as controls. While obtaining plucked hairs is
recommended by some law-enforcement agencies, this is a painful and humiliating experience
for the patient and almost never makes any difference in the final legal outcome of the
case.
If the law-enforcement jurisdiction in which you are located later requires plucked
hairs, they can ask for them at that time.
Mouth
Using two dry cotton-tipped applicators, gently obtain a specimen from each side of the
gums, both right and left, top and bottom. Smear the specimen on a glass slide and let it
air-dry. Place the dried glass slide in a cardboard slide holder, label it and seal it.
Let the cotton swabs air-dry and then place in an envelope, label it and seal it.
Use another dry cotton swab to obtain a specimen for smearing on a chocolate agar plate
or specialized collectioin medium
to test for gonorrhea. Label the plate, discard the swab and send the plate to the
laboratory.
Ask the patient to place one piece of filter paper in her mouth to become saturated
with saliva. She should not chew the filter paper. When saturated, ask her remove it from
her mouth with her own fingers and place it in an envelope. Do not touch the filter paper
yourself. Let the filter paper air-dry. Then seal it.
Carefully inspect the oral cavity, using a tongue blade and
flashlight, noting any evidence of trauma.
After examining the mouth, offer the patient
a toothbrush and toothpaste and mouthwash to rinse her mouth. Particularly if oral contact
was involved in the assault, she will feel much better after cleansing her mouth. This
will also give her a psychological break in the exam.
Neck, Back, Breasts, Abdomen and Arms
Inspect and palpate for any evidence of trauma, lacerations, bruises, abrasions,
tenderness, etc. Record any significant findings.
Hands
Collect fingernail scrapings using the wooden toothpicks, one for each hand. The
patient may do this herself with you observing.
Place the scrapings and the toothpicks in two envelopes, one for the right hand and one
for the left hand. Label and seal them.
Pubic Hair Combings
Lightly comb the pubic hair over a plain white piece of paper. Fold the comb and any
loose hairs into the paper, place in an envelope, label and seal it. There may not be any
loose hairs.
Do not pluck hairs from the pubic area to serve as controls. While obtaining plucked
hairs is recommended by some law-enforcement agencies, this is a painful and humiliating
experience for the patient and almost never makes any difference in the final legal
outcome of the case.
If the law-enforcement jurisdiction in which you are located later requires plucked
hairs, they can ask for them at that time.
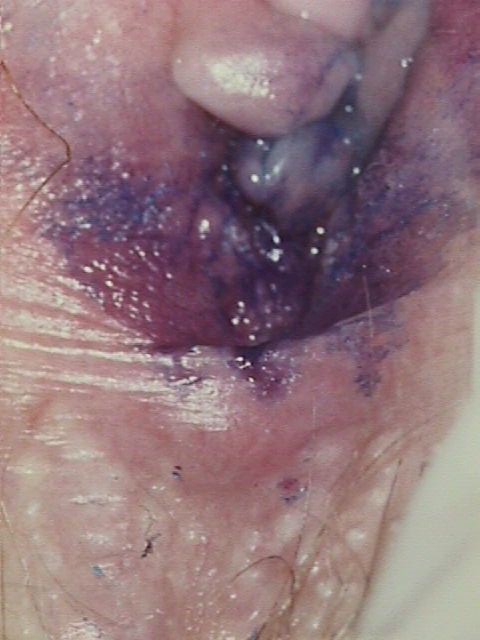
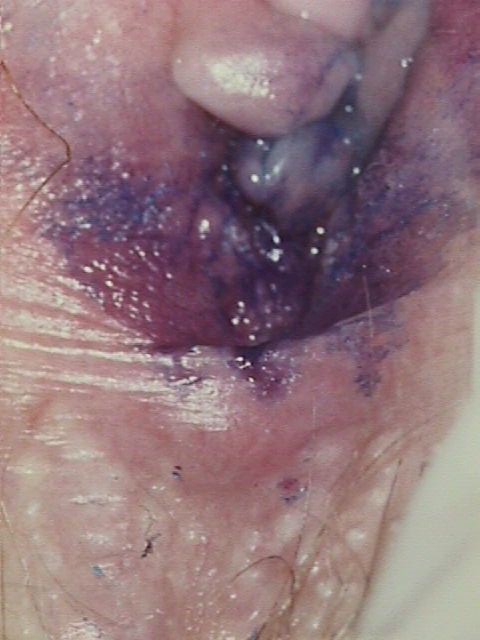
Inspect the Vulva
Using good light, carefully inspect the vulva for signs of trauma,
lacerations, bruises, abrasions, etc. Note the status of the hymen.
Application of toluidine blue dye (rinsed with vinegar) can highlight
recent trauma. The dye is retained by metabolically active cells.
Before Toluidine Blue Dye |
After Toluidine Blue Dye |
 |
 |
|
 |
 |
Visualize the Cervix
Using good light, carefully inspect the vulva for signs of trauma,
lacerations, bruises, abrasions, etc. Note the status of the hymen.

Visualize the Cervix

Rectal Laceration |
After moistening the vaginal speculum with warm water, insert it into the
vagina and inspect the vagina and cervix for signs of trauma.
Vaginal Swab
Using two dry cotton-tipped applicators, swab the vaginal walls and
posterior fornix (area beneath the cervix). Smear this specimen on a glass
slide, allow it to air-dry and place it in a cardboard slide holder. Label and
seal the slide holder. Let the cotton swabs air-dry and then place them in an
envelope. Label and seal the envelope.
Do not try to examine the vaginal or cervical specimens for motile sperm
unless you are experienced in this technique. Forensic pathologists will
examine the dried slides and their skills are considerable. You may jeopardize
later legal proceedings if you inartfully look for motile sperm and reach
conclusions which are different than those of the forensic pathologist. From
this perspective, it is better to leave the microscopic examinations to the
experts unless you have experience and training in this area.
Chlamydia Culture
Use your chlamydia test kit to obtain a cervical specimen.
Gonorrhea Culture
Use a dry cotton swab and chocolate agar plate or other suitable technique to obtain a specimen from the endocervical canal. Label the plate and send it to
your laboratory.
Rectal Inspection and Examination
In the case of rectal assault, inspect carefully for tears or breaks in
the skin of the rectum.
Toluidine Blue dye can be helpful. An anoscope can be
used to inspect the lower rectum.
Use two cotton-tipped applicators, moistened with
distilled water, to obtain a specimen from just inside the rectal
sphincter. Smear this specimen on a glass slide, allow it to air-dry and
place it in a cardboard slide holder. Label and seal the slide holder.
Let the cotton swabs air-dry and then place them in an envelope. Label
and seal the envelope.
Use another moistened cotton-tipped applicator and a
chocolate agar plate to test your patient for gonorrhea. Send this
specimen to your lab.
Bimanual Exam
After collecting all specimens, perform a bimanual exam. Using the
lubricating jelly, palpate each of the pelvic structures, noting any enlargement
or tenderness.
Betadine Douche
Once the pelvic examination is completed, a cleansing douche of Betadine
mixed in water may be appreciated by the patient. 50 to 100 cc of
solution can be used to rinse the vagina, using a 30 or 50 cc syringe. Collect
the rinse in the emesis basin and discard.
Let the patient shower and change clothes
This is important for her psychological health. Usually, there are no
major physical injuries after a sexual assault, but the psychological injuries
can be great. A part of your treatment will be to reassure her that she's "OK"
and to assist her in the cleansing process (physical and mental). Once the
specimens are collected, she should be given the opportunity to shower and
change clothes, in a sense "washing away" some of the unpleasantness of her
recent experience. Some women will decline, preferring to shower later, but many
will appreciate the offer and will feel better afterward.
Blood and Urine Tests
-
VDRL or RPR - repeat in 1 month
-
Hepatitis B - repeat in 1 month
-
HIV - repeat in 1 month and 6 months
-
Pregnancy test - repeat weekly until next menstrual flow
-
1 extra red-top tube for the Investigator (MAA or NIS)
-
Place 4-5 drops of the patient's blood (taken from the needle or
drawn from one of the red-top tubes) on a piece of filter paper and
let it air-dry. Place the filter paper in an envelope, label it and
seal it.
Offer Antibiotics
The risk of acquiring gonorrhea from a sexual assault is approximately 6 to
12% (CDC), and the risk of acquiring chlamydia probably a little higher. The
risk of acquiring syphilis is estimated at about 3%. The risk of developing AIDS
from a sexual assault cannot be precisely estimated as it depends on too many
factors but is considered to be quite low.
-
Standard prophylaxis:
-
Alternative prophylaxis:
-
During Pregnancy:
Postexposure hepatitis B vaccination (without HBIG) should adequately
protect against HBV. Hepatitis B vaccine should be administered to victims of
sexual assault at the time of the initial examination. Follow-up doses of
vaccine should be administered 1-2 and 4-6 months after the first dose. For
those known to have completed a full HBV vaccination program, additional
Hepatitis B vaccine need not be given.
Offer Emergency Contraception
The exact risk of pregnancy following a sexual assault is estimated at about
2-4%, but depends to a large extent on where the woman was in her menstrual
cycle and, of course, whether she was protected by some contraceptive method.
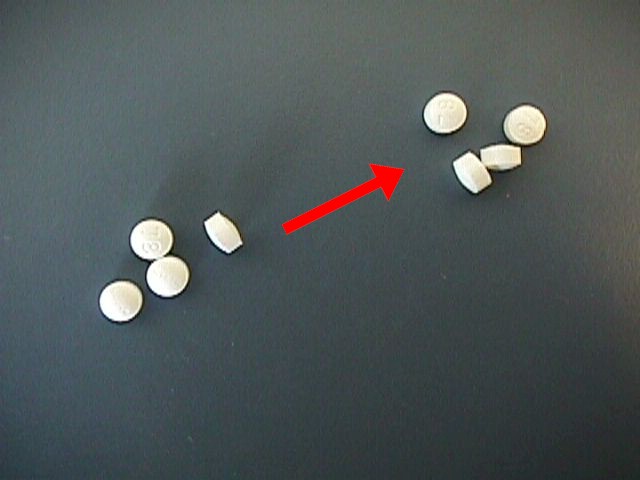
Taking 2 medium-strength BCPs (Ovral)
right away and again 12 hours later has been used successfully by many
physicians to prevent pregnancy. Alternatively, 4 LoOvral can be taken
immediately and again 12 hours later.
Such a dosage is well-tolerated by most women, but half will
experience nausea which might require anti-nausea medication. After
using this protocol, the woman's normal menstrual cycle should not be
disturbed and she will not have any withdrawal bleeding after she
completes this 4-pill regimen.
This method reduces the risk of pregnancy by 75%. It's exact mechanism of
action is not known but may involve postponing ovulation and may involve
prevention of implantation. Should a pregnancy occur despite the use of
emergency contraception there is no convincing evidence of any harm to the
fetus, although theoretical concerns will likely always be present.
You need to advise your patient of these issues, and let her decide whether
she wishes to take emergency contraception.. Whatever her decision, you should
document in the medical record your discussion and her decision.
Read more about Emergency
Contraception
Follow-up exam
About 2 weeks after the assault, the patient should be re-examined for any
lingering injury and also to provide reassurance that at least physically,
everything is totally back to normal. At this time, she will have had a
menstrual flow (typically), and she can have her follow-up labs (HIV, VDRL, Hep
B) done at the same time. This will also allow you an opportunity to see how she
is dealing with the psychological issues related to the assault.
Ideally, serologic tests for syphilis and HIV infection should be repeated
6, 12, and 24 weeks after the assault if initial test results were negative
For psychological reasons, some women may need to be seen earlier than 2
weeks to reassess their adaptation to this trauma.
Release from Medical Department
After the patient has been examined and treated and all specimens collected,
she may be released. She should not be released alone, but rather in the company
of someone she knows and trusts. It is important that she feels she is going to
a safe place.
Write your Report
Make this factual, but it need not be lengthy.
Do not draw legal conclusions about whether a sexual assault occurred or
did not occur.
That is for the courts to decide.
Give Evidence to Investigator
Using a proper Chain-of-custody form, sign over the evidence to the law
enforcement representative, consisting of:
-
Clothing
-
Copy of Consent to Release Information
-
Copy of your Medical Report
-
Glass slide of oral specimen
-
Glass slide of vaginal specimen
-
Glass slide of rectal specimen
-
Swabs of oral specimen
-
Swabs of vaginal specimen
-
Swabs of rectal specimen
-
Filter paper with saliva
-
Filter paper with 4-5 drops of patient blood
-
Combings of head hair
-
Combings of pubic hair
-
1 red-top tube of patient's blood
Give specimens to your lab
The laboratory specimens which you obtained for patient care reasons should
go to your laboratory, but may be handled in the routine fashion and not
following a Chain-of-Custody procedure. They will consist of:
Give prescriptions and Instructions to patient
The patient should have everything she needs to get her follow-up
medications. In addition, she should have written instructions on where to be
and for what purpose:
-
Antibiotics
-
BCPs (antiemetics optional but recommended)
-
Dates for weekly pregnancy tests
-
Date for 2-week follow-up exam and labs (VDRL, Hep
B and HIV)
-
Date for 6, 12 and 24-week follow-up lab (VDRL, HIV)
-
Name and phone number or location of law enforcement Investigator
-
Name of Chaplain (or social service person) and phone number or
location.
The special case of children
Children who are victims of sexual assault need special attention and may
require some modifications of the general outline.
Small children may not have an appreciation of exactly what happened
to them, or may be unable to express themselves. Some experienced
examiners will have the child use dolls to demonstrate what happened.
During sexual assault of a prepubertal child, serious internal injuries may
occur, including laceration of the vaginal wall and tearing of the uterus from
its' supports at the top of the vagina. Rectal injury may occur. Because of
this, it may be necessary to obtain other tests (upright abdomen looking for
free air in the abdomen), or to examine a child under anesthesia to determine
the extent of the injuries. Intra-abdominal injuries promptly diagnosed and
treated will usually have an excellent prognosis. The same injuries diagnosed
after peritonitis has become well-established are more grave.
Military Settings
In some advanced military settings, it may not be possible to follow
the all of the recommendations listed here. In such circumstances, an
abbreviated exam, lab evaluation and treatment are often possible, using the
resources you have available to you.
|