LESSON OBJECTIVES
4-1. Select from a list, three reasons why patients are weighed.
4-2. Select from a list, six principles related to weighing patients.
4-3. Match terms related to body temperature with the correct definition.
4-4. Select from a list, the converted Fahrenheit to Centigrade temperature or vice versa.
4-5. Identify patients who are at risk of hypothermia.
4-6. Identify methods for obtaining an oral, rectal, and axillary temperature.
4-7. Identify precautions, which must be taken when obtaining an oral, rectal, and axillary temperature.
4-8. Identify anatomical sites where a pulse may be taken.
4-9. Select from a list, factors which affect the pulse rate.
4-10. Match terms describing a pulse with the correct definition.
4-11. Match terms related to breathing patterns with the correct definition.
4-12. Match terms related to blood pressure with the correct definition.
4-13. Select from a list, the correct statements relating to a normal adult blood pressure.
4-14. Identify factors, which influence blood pressure values.
4-14. Identify anatomical sites where the blood pressure may be taken.
4-16. Select from a list, principles related to obtaining the blood pressure.
4-1. INTRODUCTION
Soon after a patient arrives on the nursing unit you should begin your nursing assessment. You should take several measurements to establish a baseline for further observations of that patient. Among these measurements are height, weight, and vital signs. The vital signs are the body temperature, the pulse or rate of heartbeats, the respiration or rate of breathing, and the blood pressure. The vital signs are abbreviated TPR and BP for temperature, pulse, respirations and blood pressure. These readings are called vital signs because they all must be present for life to continue.
4-2. HEIGHT AND WEIGHT
The patient’s height and weight are recorded on admission for several reasons.
a. Diet Management. The patient’s ideal weight may be determined. The health care team will also be able to monitor weight loss or gain.
b. Observation of Medical Status. Taking the patient’s height and weight may indicate that the patient is overweight, underweight, or is retaining fluids (edema). The health care team can observe changes in weight caused by specific disease processes and determine the effectiveness of nutrition supplements prescribed to maintain weight.
c. Calculation of Medication Dosages. Drug dosage is often prescribed in relation to a patient’s weight when a specific blood concentration of the drug is desired. Larger doses may be required in a heavier person.
4-3. MEASURING HEIGHT AND WEIGHING THE PATIENT
a. To measure height, have the patient stand on the scale with the back to the measuring bar.
b. Ask the patient to stand straight. Lower the bar so that it lightly touches the top of the patient’s head.
c. Record the height in inches or centimeters in accordance with local policy.
d. If the patient cannot stand, obtain an approximate height in bed.
(1) Have the patient lie on his back and stretch as much as possible.
(2) Place a mark on the bottom sheet at the patient’s heel and at the top of the patient’s head.
(3) Measure between these two marks on the taut bottom sheet.
e. Principles related to weighing the patient.
(1) Weigh the patient before breakfast, at the same time each day.
(2) Use the same scale each time.
(3) Ensure that the scale is properly balanced.
(4) Weigh the patient in the same amount of clothing each day (i.e., hospital gown or pajamas).

(5) Have the patient void before weighing.
(6) Avoid weighing any equipment attached to the patient such as drainage bags or telemetry units. Hold the equipment while actually weighing the patient.
f. A helpless patient may be weighed while lying down on a litter scale. This scale is a sling-type device that looks like a suspended hammock. You will need assistance to place the patient on the scale.
g. Record the patient’s weight on the graphic sheet and in the nurses’ notes.
4-4. TEMPERATURE
Being human, we are homeothermic; we are warm-blooded and maintain body temperature independently of our environment. Our body generates heat as it burns food. It loses heat through the lungs (breathing), through the skin (sweating), and in body discharges (urine, feces, vomitus, or blood). Body temperature is defined as the measure of the heat inside the body: the balance between heat produced and heat lost.
4-5. TEMPERATURE REGULATION
a. Heat is produced through the metabolism of food (chemically). Food is used as energy by muscles and glands to generate most of the heat in the body. Heat is also gained (physically) from the environment.
b. During exercise, the muscles become active and the person feels warm. Increasing muscular tone (shivering or gooseflesh) produces heat. The process of digestion also increases body temperature.
c. When a person becomes angry or excited, the adrenal glands become very active and the body warms as a result of the action of certain body chemicals such as epinephrine.
d. Cold, shock, and certain drugs, which depress the nervous system, decreases heat production.
e. The hypothalamus is the body’s thermostat. It is located in the central nervous system at the base of the brain. This heat-regulating center in the brain senses any changes in the temperature of blood it receives and makes the appropriate adjustments.
f. Heat loss occurs through the following:
(1) Conduction–direct physical contact with an object.
(2) Convection–when body heat warms surrounding air which rises and is replaced by cooler air.
(3) Radiation–body heat warms surrounding objects without physical contact.
(4) Evaporation–perspiration that is removed from the body surface by change from a liquid to a vapor.
4-6. NORMAL BODY TEMPERATURE
A thermometer is placed in the patient’s mouth to obtain an oral temperature, in the anal canal to obtain a rectal temperature, and in an axilla (armpit) to obtain an axillary temperature. Table 4-1 shows the average normal temperature for well adults at these various body sites.
| Table 4-1. Average, normal temperatures for well adults. | ||
|---|---|---|
| Oral | Rectal | Axillary |
| 98.6 | F 99.5 | F 97.7 |
| 37.0 | C 37.5 | C 36.5 |
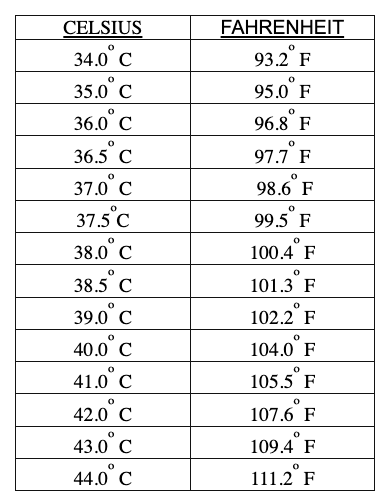
a. Temperature is measured on the Fahrenheit (F) or the Celsius (C) scale. The average, normal, oral temperature for an adult is 98.6 degrees Fahrenheit or 37.0 degrees Celsius (old term: centigrade).
b. You can convert Fahrenheit to Celsius or vice versa. To convert Fahrenheit to Celsius, subtract 32 and multiply by 5/9. To convert Celsius to Fahrenheit, multiply by 9/5 and add 32. See Table 4-2 for a conversion chart.
c. Body temperature may wary by 0.5ºF either way and still be within normal limits.
4-7. FACTORS WHICH INFLUENCE NORMAL BODY TEMPERATURE
a. Individual metabolism differs. An increase in the emotional state of the patient may increase the temperature.
b. Body temperature is usually lowest in the morning and highest in the late afternoon or evening.
c. Normal temperature for infants and children is usually higher than the normal adult temperature. At birth, heat-regulating mechanisms are not fully developed, so a marked fluctuation in body temperature may occur during the infant’s first year of life.
d. In some women, ovulation may be signaled by a slight drop in body temperature 12 to 24 hours before a postovulation rise in temperature of about 0.4ºF to 0.8ºF.
4-8. TERMINOLOGY RELATED TO BODY TEMPERATURE
Body temperature rises when heat production increases or when heat loss decreases; both may be going on at the same time.
a. Everyone has a temperature; when the temperature is elevated, then pyrexia or a fever is present. A fever is a symptom of some disorder. It often accompanies illness; usually when the body is fighting an infection. An antipyretic is a fever-reducing agent such as aspirin.
b. A temperature significantly below normal is called hypothermia. Such temperatures often precede normal death. Hypothermia may occur as a result of overexposure to winter elements or to cold water. Accidental hypothermia is life threatening and must be treated immediately. Clinical hypothermia is often used to perform surgical procedures because the lowered body temperature slows metabolism and thus decreases the need for oxygen.
c. The patients most at risk of hypothermia are:
(1) Postoperative patients.
(2) Newborn infants exposed to room temperatures before their body temperature has stabilized.
(3) Elderly or debilitated patients.
4-9. TAKING THE TEMPERATURE
Regardless of the type of thermometer or measuring probe used, certain rules apply.
a. The bulb or electronic probe is placed so it will be completely surrounded by body tissues.
b. Multi-use thermometers and temperature probes are covered when used. The cover is removed and discarded after the temperature is taken. Prelubricated covers are used for rectal thermometers.
c. The temperature is recorded on the patient’s graphic chart to the even two tenths of a degree (unless the electronic thermometer is used). An electronic thermometer is not calibrated with multiple numbers. It displays only the measured temperature. Record the measured temperature.
4-10. TYPES OF THERMOMETERS
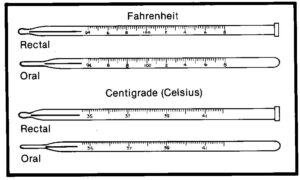
a. Clinical. The clinical thermometer is a glass bulb containing mercury, with a stem in which the mercury can rise. The stem has lines representing the measuring scale. It must read below normal range before the temperature is taken. It should be rinsed in cold water to avoid distribution of the mercury and breakage. If the thermometer is kept in a chemical solution, dry it with a wipe in a twisting motion starting at the bulb. The clinical thermometer may be oral or rectal.
(1) The oral thermometer has a long, slender bulb. It may also be used for axillary measurement.
(2) The rectal thermometer has a blunt, short, fat bulb. It should not be stored with the oral thermometers.
b. Electronic. The electronic thermometer is portable and battery operated. It registers the temperature in 10 seconds or less and displays it digitally. It must be fully charged to give an accurate reading, so be sure the thermometer’s base is plugged into an electrical outlet between uses. Separate oral and rectal probes are supplied with each unit.
c. Disposable. The disposable is single-use and has a sensor at the end of the shaft, which measures the temperature.
d. Patch. The thermometer patch is a strip, which contains liquid crystals that change colors as the temperature changes. It is usually placed on the forehead. The scale is adjusted to convert skin-surface temperature to inner-body temperature. The calibration is not as detailed as that of a glass thermometer.
4-11. METHODS OF OBTAINING A TEMPERATURE
a. To obtain an oral temperature, place the thermometer in the sublingual pocket and have the patient close his mouth around it. Instruct him not to bite down. Leave the thermometer in place 3 to 4 minutes. If the patient has been eating, drinking, smoking, brushing his teeth, or chewing gum within the past 15 minutes, wait at least 15 minutes to take the temperature.
b. To obtain a rectal temperature, lubricate the bulb and the area up to 1 inch above it. Use a lubricated probe cover with an electronic thermometer. Turn the patient on his side, fold back the bedding and separate the buttocks so that you can easily see the anal opening. Insert the thermometer approximately 1.5 inches into the anus. Hold the thermometer in place for 3 to 4 minutes.
c. To obtain an axillary temperature, place the thermometer in a dry axilla. Keep the arm close to the body to ensure contact with the bulb or probe for 8 to 10 minutes. Axillary is the method of choice for an infant.
d. Precautions.
(1) Oral temperatures are contraindicated for an unconscious patient, for an infant, or when the patient must breathe through the mouth.
(2) The rectal method of obtaining the temperature is contraindicated if the patient has diarrhea, rectal disease, or has recently had rectal surgery.
4-12. PULSE
The pulse is the vibration of each wave of blood going through the arteries as the heart beats. The pulse rate is usually equal to heart rate, but may be lower if there is an obstruction of the artery or if the heart rhythm is weak or irregular. You can feel it by placing your fingers over one of the large arteries that lie close to the skin, especially if the artery runs across a bone and has very little soft tissue around it.
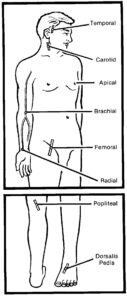
a. There are eight common arterial pulse sites. (See figure 4-2).
(1) Radial.
(2) Temporal.
(3) Carotid.
(4) Apical (listening to the heart directly).
(5) Brachial.
(6) Femoral.
(7) Popliteal.
(8) Pedal (dorsalis pedis)
b. The rate that the heart beats varies with the patient’s age, size, and weight. The normal rate for an adult is 60 to 80 beats per minute. Women have a slightly higher average rate than men. The pulse of an infant ranges from 120 to 140 beats per minute. Rates for children vary according to the size and the age of the child.
c. Activity affects the pulse rate. Exercise or heavy physical work cause the heart to beat faster and the pulse rate to increase. Excitement, anger, and fear increase the rate. Some drugs, such as caffeine, may also increase the pulse rate. If the patient has a fever, the pulse rate increases in proportion to the body’s temperature: the pulse rate goes up about 10 beats for every 1ºF (0.56ºC). These conditions cause a temporary increase in the heartbeat and pulse rate. The heartbeat and pulse rate that is consistently above normal may be a sign of heart disease, heart failure, hemorrhage, an overactive thyroid gland, or some other serious disturbance. The term for an abnormally rapid heartbeat is tachycardia. When the heartbeat is continuously slow, below 60 per minute, the condition is called bradycardia.
4-13. DESCRIBING THE PULSE
a. Pulse rate describes how often the heart beats.
b. Pulse volume describes the force with which the heart beats. The volume of the pulse varies with the volume of blood in the arteries, the strength of the heart contractions, and the elasticity of the blood vessels. A normal pulse can be felt with moderate pressure of the finger. When every beat is easily felt, the pulse is described as strong. When greater pressure exerted by the finger cannot blot out the pulse, it is called full or bounding. A pulse with little force is described as weak or thready.
c. Pulse rhythm is the spacing of the heartbeats. When the intervals between the beats are the same, the pulse is described as normal or regular. When the pulse skips a beat occasionally, it is described as intermittent or irregular. A pulse may be regular in rhythm but irregular in force, with every other beat being weak. To obtain an accurate assessment of the heart rate, the pulse is counted by listening directly to the heart (apical pulse).
4-14. FACTORS, WHICH AFFECT THE PULSE RATE
The pulse rate is an indicator of how fast the heart beats. The pulse rate is affected by several factors.
a. Age. A normal pulse for infants range from 90 to 170 and the rate gradually decreases up to age 14 when it is equal to the normal adult pulse rate of 60 to 100.
b. Body Build and Size. A short, fat person may have a higher rate than a tall, slender person.
c. Blood Pressure. As the blood pressure decreases, the pulse will frequently increase.
d. Medications. Stimulants will increase the pulse rate; depressants will decrease the pulse rate.
e. Exercise and Muscular Activity. An increase in pulse rate will occur with increased activity to meet increased oxygen and nutrient demands. A regular aerobic exercise program can lower the resting pulse. A person, who exercises a great deal, such as an athlete, will develop bradycardia that is a normal, health condition. The body slows the heartbeat to compensate for the greater volume of blood pumped with each beat.
f. Food Intake. Digestion increases the pulse slightly.
g. Elevated Body Temperature. The pulse increases approximately 10 beats per minute for every 1 F (0.56º C) increase in body temperature. These conditions cause a temporary increase in the heartbeat and pulse.
h. Emotional Status. Fear, anger, and anxiety will all increase the pulse rate.
i. Pain. When the patient is in pain, the pulse rate will increase.
4-15. MEASURING THE PULSE
a. Measuring a Radial Pulse.
(1) Wash your hands to prevent the spread of infection.
(2) Supporting the patient’s arm and hand with the palm down, press the first, second, and third finger of your dominant hand gently against the radius bone until you feel the contraction and expansion of the artery with each heartbeat. Do not use your thumb; it has a strong pulse of its own and you may be counting your pulse.
(3) Count the pulsations for 30 seconds using a watch with a second hand or digital display to time yourself. Multiply the count by 2 to determine the rate for 1 minute. If the pulse is abnormal in any way, count for a full minute to get a more accurate reading.
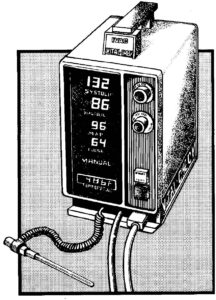
(4) The pulse rate may also be determined by the electronic vital signs monitor (see figure 4-3).
(5) If there is any doubt about the rhythm or rate of the heart, take an apical pulse.
b. Measuring an Apical Pulse.
(1) Warm the stethoscope in your hands. A cold stethoscope may surprise the patient and alter the pulse rate.
(2) Place the stethoscope at the apex (pointed end) of the heart, in the left center of the chest, just below the nipple. The pulse can usually be heard best at the apex.
(3) Count the pulse for one full minute.
c. Measuring the Apical-Radial Pulse.
(1) If the apical-radial (A-R) pulse is ordered by the physician, two nurses carry out the procedure together.
(2) Using the same watch, one nurse counts the patient’s apical pulse for 1 minute while the other nurse counts the radial pulse for 1 minute. One nurse gives the signal to start counting, and both start at the same time. The two figures are identified and charted (A-R pulse 76/72, for example). Normally, these two readings should be the same. If there is a difference, it is called the pulse deficit.
NOTE: An apical pulse will never be lower than the radial pulse.
4-16. RESPIRATION
Respiration is the process that brings oxygen into the body and removes carbon dioxide waste. The exchange occurs in the lungs. Respiration occurs in two phases: internal and external.
a. Internal respiration is the process by which oxygen is taken from the bloodstream into the cell and carbon dioxide is removed from the cell to the bloodstream.
b. External respiration refers to delivery of oxygen to the lungs so that it can be taken into the bloodstream. External respiration (breathing) has two components: Inspiration, the process of taking air into the lungs; and expiration, expelling air from the lungs.
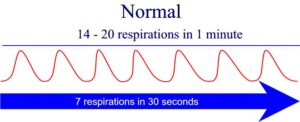
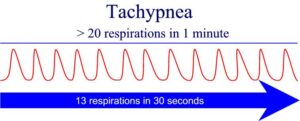
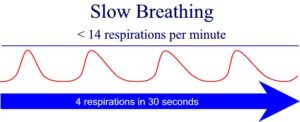
c. It is the rate of external respiration that is measured. The normal adult rate is 14 to 20 breaths per minute. Women have a more rapid rate than men. Newborns have a normal rate of about 40. Children have a normal rate of 25 to 30.
d. Respiration is controlled and regulated by the respiratory center in the brain and by the amount of carbon dioxide in the blood. Respiration is involuntary and automatic. You can control the action of your breathing to some extent, but only for a limited time. If automatic breathing does not occur, a breathing disorder exists.
4-17. BREATHING PATTERNS
a. Normal breathing is relaxed, effortless, and regular.
b. Rapid breathing is a rate above 20 breaths per minute, associated with increased activity or a disease process. The medical term is tachypnea.
c. Slow breathing is a rate below 14. It may also be described as shallow if the patient takes in and breathes out small amounts of air.
d. Difficult breathing describes when a person is making a definite effort to get more oxygen and get rid of carbon dioxide. Dyspnea is the term for difficult breathing. Dyspnea is also the term used for painful breathing, a subjective pattern, which must be stated by the patient. Dyspnea may be a temporary condition, such as when a runner gasps at the end of a race or when a person pants “to get his breathe” after climbing stairs. In some diseases, such as pneumonia, emphysema, or some types of heart conditions, breathing difficulty is more or less constant. Signs of breathing difficulties are: heaving of the chest and the abdomen, and cyanosis (a bluish tinge in the skin).
e. Orthopnea is the term used if the patient can breathe only when in an upright position.
f. Apnea is the absence of respirations.
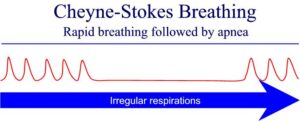
g. Cheyne-Stokes is the term for cycles of breathing characterized by deep, rapid breaths for about 30 seconds, followed by absence of respirations for 10 to 30 seconds. Cheyne-Stokes respirations constitute a serious symptom and usually precedes death in cerebral hemorrhage, uremia, or heart disease.
4-18. BLOOD PRESSURE
Two things determine the blood pressure: the rate and force of the heartbeat and the ease with which the blood flows into the small branches of the arteries. When the heart rate or force is increased by exertion or illness, blood pressure increases. If the volume of blood within the circulatory system is reduced (as in hemorrhage), and other factors remain the same, blood pressure decreases.
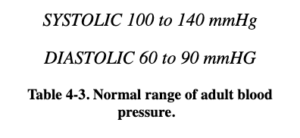
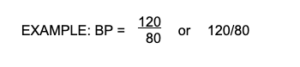
a. Blood pressure is the pressure exerted by the blood on the walls of the blood vessels within the systemic arterial system. Normal systolic pressure for a young adult is 100 to 120 mmHg (millimeters of mercury); diastolic pressure is about 80. Blood pressure increases gradually with age. Normal systolic pressure for a person 60 years of age is 130 to 140. Hypertension is blood pressure above normal limits (above 140/90); it is a sign of a circulatory problem. Hypotension is blood pressure below normal limits (below 90/60) and may indicate shock. See table 4-3.
b. Systolic blood pressure is greatest. It is the pressure against the wall of the blood vessels following ventricular contraction. Using the auscultatory (listening) method, the systolic blood pressure is recorded at the highest point at which two consecutive beats are heard (Korotkoff sounds).
c. Diastolic blood pressure is lowest. It is the pressure against the blood vessels when the heart is relaxed before it begins to contract again.
d. The mean arterial pressure (MAP) denotes the average pressure within the arteries. An electronic vital signs monitor can determine and display an accurate average pressure or MAP.
e. Shock or other difficulty is usually indicated by a systolic reading of 80 or less. A diastolic reading over 100 is usually considered dangerously high.
4-19. MEASURING BLOOD PRESSURE
Blood pressure is usually measured indirectly using a stethoscope and an instrument called the sphygmomanometer. The most common site is the arm just above the antecubital area, using the brachial artery. Blood pressure may be measured directly by means of a catheter or probe inserted into a blood vessel or the heart.
a. Direct Measurement.
(1) One means of direct blood pressure measurement is to place a special tube in a vein and monitor central venous pressure (CVP). Central venous pressure may be used to determine fluid needs in shock, hemorrhage, or severe burns, to detect pulmonary edema, and to determine the extent of circulatory overload.
(2) Another method of direct blood pressure measurement is internal or invasive monitoring. A large, flexible catheter, such as a Swan-Ganz catheter measures pressures within the heart itself.
b. Indirect Measurement. The sphygmomanometer (often called a blood pressure apparatus) includes a wide, cloth-covered rubber cuff with two rubber tubes extending from it. One tube is connected to a bulb air pump that has a valve, which can be opened or closed. The other tube is connected to a glass cylinder containing mercury (mercury manometer) or to a dial (aneroid manometer), which attaches to the arm wrap. You obtain the indirect blood pressure reading with the manometer by listening to the heartbeat with a stethoscope.
(1) Cleanse the stethoscope and earpiece with an alcohol wipe before and after the procedure (unless you use your own stethoscope).
(2) Have the patient lie down or rest comfortably in a chair with the arm supported and the palm turned upward to expose the brachial artery on the inside of the elbow.
(3) Let the air out of the cuff. Wrap the cuff firmly around the arm, just far enough above the elbow to leave the space over the brachial artery free, and fasten the clip or Velcro closure.
(4) Find the pulse in the artery and place the stethoscope over the spot where you can feel the strongest pulsations.
(5) Pump the manometer bulb to 20 mm above a possible systolic pressure. Release the valve on the manometer bulb to gradually release air from the cuff.
(6) Note the level on the mercury column or dial at which you first hear a heartbeat. This is the systolic pressure.
(7) Continue gradually releasing air from the cuff. Note the point on the mercury column or dial at which the heartbeat cannot be heard, or at which there is a distinct change in the sound. This is the diastolic pressure.
(8) Release the remaining air from the cuff. Record the blood pressure reading on the patient’s chart by writing the systolic pressure above the diastolic pressure. Use only even numbers.
c. Alternate Site for Measurement. If it is impossible to measure the blood pressure in the arm, the leg is used. When blood pressure is taken in the leg, the popliteal space (popliteal artery) is used, and the cuff is applied above the knee. If you measure the blood pressure at any site other than the arm, use the appropriate size cuff and indicate the site on the chart.
d. Electronic Blood Pressure Apparatus. The cuff of the electronic blood pressure apparatus is applied and manipulated in basically the same manner as with the mercury or aneroid manometer. The cuff is usually inflated and deflated automatically. It is important to place the microphone under the cuff so the arrow that indicates “artery” is in the correct location. Systolic and diastolic pressures will be printed out on the screen within a few seconds.
4-20. FACTORS WHICH INFLUENCE BLOOD PRESSURE VALUES
a. Age. Children normally have lower blood pressure at birth (80/60), which gradually increases until the age of 18 when it becomes equal to the normal adult pressure. Older adults frequently have higher blood pressure due to a decrease in blood vessel elasticity.
b. Sex. Men have higher blood pressure than women of the same age.
c. Body Build. Blood pressure is usually elevated in an obese person.
d. Exercise. Muscular exertion will temporarily elevate the blood pressure. A regular exercise program can eventually decrease the resting blood pressure.
e. Pain. Physical discomfort will usually elevate the blood pressure.
f. Emotional Status. Fear, worry, or excitement can elevate the blood pressure.
g. Disease States and Medication. Some disease conditions and/or the medications influence the blood pressure.
4-21. PRINCIPLES RELATED TO OBTAINING THE BLOOD PRESSURE
a. The patient’s arm must be at the level of the heart. If the arm is below the heart, false elevated pressures are obtained. If the arm is above the heart, false lowered blood pressures are obtained.
b. The arm should be supported during the entire procedure to prevent elevation due to muscle contractions used to maintain the position.
c. The cuff and stethoscope should be placed directly on the skin. Light pressure should be applied when placing the stethoscope over the artery.
d. The cuff should be quickly deflated to zero, once the last measurement is heard. Wait a minimum of 30 seconds before measuring the blood pressure again.
4-22. THE GRAPHIC SHEET
a. A graphic sheet is maintained so that all vital sign readings are easily accessible to members of the health care team. Each reading is recorded as a dot in the proper space, with lines connecting the dots. Readings throughout the patient’s illness are indicated across the page in unbroken lines. The form used to graphically record the patient’s vital signs in a United States (US) Army hospital is SF 511, Clinical Record–Vital Signs Record.
b. Recording data.
(1) Enter the patient’s identification data in the space at the bottom of the form.
(2) Number the “Hospital Day” line of blocks with the day of admission as one, and continue consecutively. Use the “Post-op Day” line as applicable. The day of surgery is the operative day. The day following surgery is noted as the first post-operative day.
(3) Label the day/hour blocks properly.
(4) Represent temperature by dots placed between the columns and rows, and joined by straight lines. If the temperature is other than oral, indicate so by (R) for rectal or (A) for axillary.
(5) Show pulse by use of a circle connected by straight lines.
(6) Enter the respiration and blood pressure on the indicated rows below the graphic portion.
(7) Record frequent blood pressure readings on the form’s graphic portion by entering an “X” between the columns and rows of dots, at points equivalent to systolic and diastolic levels. Connect the two with a vertical solid line.
(8) Use blank lines at the bottom of the sheet to record special data such as the 24-hour total of the patient’s intake and output.
4-23. CLOSING
Measuring and recording vital signs is not complicated; however, these are important tasks because these measurements are indicators of functions, which are necessary to sustain life. The patient’s current vital signs can be compared with those previously obtained or with normal values and changes in health can be detected and treated quickly.