LESSON OBJECTIVES
1-2. Select the functions of the practical nurse during the physical examination.
1-3. Identify the health care providers who could perform the physical examination.
1-4. Identify the body systems that the health care provider would usually examine during a physical examination.
1-5. Select the physiological measurements/ values which are routinely made during a complete physical examination.
1-6. Identify the supplies and equipment that should be available in the examination room.
1-7. Select the nursing implications, which apply during the physical examination of a patient.
1-8. Match the correct body position with the description or an illustration of the body position.
1-9. Select the purposes for draping a patient during the physical examination.
1-10. Select the nursing implications, which relate to evaluation of the patient’s condition in terms of the need for assistance during a physical examination.
1-1. INTRODUCTION
The history and the physical exam provide much of the information known about the patient’s health status. As a practical nurse, you may be called upon to assist the physician or other health care providers during a physical examination. You should know the basics of the examination in order to have the appropriate equipment and supplies on hand, and so that you may place the patient in the proper position and drape him correctly.
1-2. PURPOSES FOR PERFORMING A PHYSICAL EXAMINATION
The physical examination can be performed by the following health care providers: a physician, nurse practitioner, or physician assistant. The health care provider makes specific and general observations as he examines the patient from head to toe. The exam should include the eyes, ears, nose, mouth, throat, neck, chest, breasts, abdomen, and extremities. A vaginal or rectal examination is performed if indicated. The purposes for performing a physical examination are:
a. To determine the patient’s level of health or physiological function.
b. To arrive at a tentative diagnosis when there is a health problem or disease.
c. To confirm a diagnosis of disease or dysfunction.
d. To evaluate the effectiveness of prescribed medical treatment and therapy.
1-3. FUNCTIONS OF THE PRACTICAL NURSE DURING THE EXAMINATION PROCEDURE
a. Ensure that the patient feels comfortable and is not embarrassed. Prior to the examination, tell the patient what will take place and explain the reason for the procedure. The patient who knows what to expect will be more relaxed and cooperative.
b. Ask the patient to void into a urine specimen cup in order to empty the bladder and save the urine specimen for urinalysis. Have the patient put on a hospital gown so that his body is more accessible for examination.
c. Arrange equipment and supplies. Be sure that you have everything needed (see Table 1-1). Test all equipment to make certain that it works correctly.
| Table 1-1. Supplies and equipment. | |
|---|---|
| Hospital gown | Tongue depressors |
| Sheet or disposable paper drapes | Ophthalmoscope (for examining eyes) |
| Bath blanket (to prevent chill) | Otoscope (for examining ears) |
| Tray with flashlight, gloves, lubricant, normal saline, cotton- tipped applicators, and tissues | Tuning fork |
| Basin for soiled instruments | Blood pressure apparatus and stethoscope |
| Waste container for paper goods | Percussion hammer (to check reflexes) |
| Scale with height measuring rod | Red and blue pencils (to mark skin) |
| Gooseneck lamp or hospital light | Small speculum (for nose examination) |
| Gloves | Head mirror (to reflect light into body orifice, such as the throat |
| Thermometer (oral or rectal) | You may also need slides, blood tubes, a vaginal speculum, or other equipment; medications; and a surgical permit if a biopsy or other tests are to be done. |
| Tape measure | |
d. Accompany the patient to the examination room and assist him onto the table. Your presence lends support and reassurance to the patient. If a male is examining a female patient, or vice versa, stay in the room to protect the patient, the health care provider, and the hospital or clinic.
e. Wash your hands and measure the patient’s vital signs (temperature, pulse, respiration, blood pressure), height, and weight. Wear gloves if the patient has a draining wound, is bleeding, is vomiting, or has an infection. (See Universal Body Substance Precautions in this subcourse).
f. Have the patient’s chart available. The physician needs to know the information that has already been obtained via the nursing observations and lab reports. Call the physician’s attention to any abnormal lab values. Do this away from the patient.
g. Have all lab slips and x-ray slips ready with the patient’s name, rank, social security number, date, and other required information.
h. Assist the patient to assume the proper position for each part of the examination (see figures 1-1 to 1-7). To provide continuing privacy, be sure to adjust the drapes each time the patient assumes a different position. If the patient is asked to stand erect, place paper towels on the floor or have the patient put on slippers.
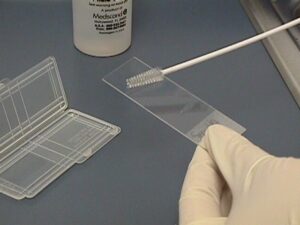
i. Hand instruments and supplies to the physician. Properly label and care for all specimens collected.
j. See that the patient is returned safely to his room and is comfortable.
k. Place all instruments in the proper area for disinfection or sterilization and dispose of all wastes. Wash your hands again. See that the examination room is cleaned. Decontaminate the room if necessary. Change the cover on the tables. Replace all equipment.
1-4. POSITIONING A PATIENT FOR EXAMINATION OR TREATMENT
Patients are put in special positions for examination, for treatment or test, and to obtain specimens. You should know the positions used, how to assist the patient, and how to adjust the drapes.
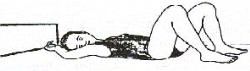
a. Horizontal Recumbent Position. Used for most physical examinations. Patient is on his back with legs extended. Arms may be above the head, alongside the body or folded on the chest.
b. Dorsal Recumbent Position. Patient is on his back with knees flexed and soles of feet flat on the bed. Fold sheet once across the chest. Fold a second sheet crosswise over the thighs and legs so that genital area is easily exposed.
c. Fowler’s Position. Used to promote drainage or ease breathing. Head rest is adjusted to desired height and bed is raised slightly under patient’s knees.
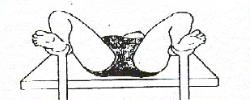
d. Dorsal Lithotomy Position. Used for examination of pelvic organs. Similar to dorsal recumbent position, except that the patient’s legs are well separated and thighs are acutely flexed. Feet are usually placed in stirrups. Fold sheet or bath blanket crosswise over thighs and legs so that genital area is easily exposed. Keep patient covered as much as possible.
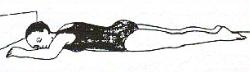
e. Prone Position. Used to examine spine and back. Patient lies on abdomen with head turned to one side for comfort. Arms may be above head or alongside body. Cover with sheet or bath blanket.
NOTE: An unconscious patient, or one with an abdominal incision or breathing difficulty usually cannot lie in this position.
f. Sim’s Position. Used for rectal examination. Patient is on left side with right knee flexed against abdomen and left knee slightly flexed. Left arm is behind body; right arm is placed comfortably.
NOTE: Patient with leg injuries or arthritis usually cannot assume this position.
g. Knee-Chest Position. Used for rectal and vaginal examinations and as treatment to bring uterus into normal position. Patient is on knees with chest resting on bed and elbows resting on bed or arms above head. Head is turned to one side. Thighs are straight and lower legs are flat on bed.
NOTE: Do not leave patient alone; he/she may become dizzy, faint, and fall.

1-5. BODY SYSTEMS USUALLY EXAMINED BY THE PHYSICIAN
a. Musculoskeletal System. The patient should be examined for symmetry of parts, for mobility, and for coordination.
b. Integumentary System. The patient’s skin should be observed for intactness, color, the presence of scars or rashes, and the skin should be felt for warmth and unusual texture.
c. Eyes, Ears, Nose, and Throat. The patient should be examined for patency of passages and cavities, state of balance (equilibrium), and the receptiveness of the sense organs.
d. Cardiovascular System. The heart is listened to with a stethoscope to measure the rate, character, and regularity of the heartbeat, as well as to detect any abnormal sounds. Status of the heart and blood vessels is determined by indirectly measuring blood pressure and by directly measuring central venous or arterial pressure. Circulation and pulses in various parts of the body, especially the extremities, may be checked. By looking at blood vessels in the retina with an ophthalmoscope, the physician can infer the condition of the blood vessels in the rest of the body.
e. Respiratory System. The respiratory system is evaluated for respiratory rate, adequacy of ventilation and gas exchange membranes, clear lung fields, and symmetry of the chest. The physician can learn a lot about the chest and estimate the size and location of the heart and lungs by auscultation (listening) and by percussion (tapping and thumping). Arterial blood may be drawn to be analyzed for blood gases.
f. Gastrointestinal (GI) System. The GI tract is examined for intactness of mucosal membranes, adequacy of digestive process, and regular elimination of solids. Because portions of the digestive tract cannot be seen directly, X-ray procedures, such as a GI series, or gallbladder series are often ordered. Feces may also be examined for the presence of blood or pathogens. The physician may explore the rectum with a gloved finger. The patient is often in the Sims’ position for this examination.
g. Neurologic System. The neurologic examination evaluates normal reflexes, adequate motor and sensory innervation, development of intellectual and psychological processes. It may consist of assessing the patient’s orientation to time and place, assessing sensation by stimulating various parts of the body, and assessing the patient’s sense of balance or ability to control body movements. A percussion hammer is used to test reflexes in various parts of the body. In addition, the pupils are checked with a flashlight for reflex. The pupils should quickly contract when a bright light is shined into the eye. The pupils should be round, regular, and of equal size. This is reported as PERRLA (pupils equal, round and reactive to light and accommodation). Accommodation is adjustment, especially of the eye, to variation in distance.
h. Genitourinary System. Genitourinary evaluation is to determine adequacy of urinary control and elimination, patency of membranes and passages, and appropriate development of reproductive organs. A vaginal or pelvic examination is done to discover any signs of irritation, growths, displacement, or other abnormal conditions in the pelvic organs or external genitalia. A rectal examination is usually included in the physical examination of a man over 35 years old. This exam aids in discovering cancer of the rectum or prostate gland while it is still in an early stage.
i. Endocrine System. The physician may palpate (use hands and fingers to examine) the sex glands and the thyroid gland to determine size and detect any growths. The adequacy of hormonal activity is assessed by observing certain characteristics of body function, growth, and development.
1-6. ASSISTING WITH AN INFANT OR CHILD
a. Make every effort to get the child’s cooperation during the examination. If the child is too young or too ill to cooperate, use restraint when necessary. Position the child’s arms along side the body and wrap the child in a sheet or blanket. Stand on the opposite side of the table from the examiner during the chest and abdominal examination. Hold the child’s arms above his head with one of your hands and his feet at the ankles with your other hand.
b. The equipment used to examine an infant or child is the same as for adult except some items are smaller.
1-7. PHYSIOLOGICAL MEASUREMENTS ROUTINELY MADE
a. The patient’s vital signs (temperature, pulse, respirations), blood pressure, height, and weight should be taken before the examination but 10 to 15 minutes after the patient has rested.
b. Routine examinations such as complete blood count (CBC) with differential, urinalysis, electrolytes, and chest x-ray are usually ordered. Complete the lab and x-ray request slips with the patient’s name, rank, social security number, date, and all other required information.
c. Have the results from all lab tests available so that the health care provider can observe/assess and be aware of any abnormal lab values.
1-8. PURPOSES FOR DRAPING THE PATIENT DURING THE PHYSICAL EXAM
The patient should be drapped:
a. To prevent unnecessary exposure of the patient’s body.
b. To help the patient relax—a patient who is embarrassed will be tense and less cooperative.
c. To prevent chilling — the drapes will provide warmth.
1-9. EVALUATION OF A PATIENT’S CONDITION AND NEED FOR ASSISTANCE
Your presence will be comforting for most patients. Some parts of the examination may be uncomfortable or painful. Evaluate the patient’s condition and his need for assistance prior to the physical examination. Some factors to consider are:
a. Age. Elderly patients will probably need help getting to the examination room, getting on the examination table and assuming certain positions. Infants and children will not be cooperative and may need restraining.
b. Level of Understanding. Patients who are confused, unable to understand English, or very young may need nonverbal communication such as a smile or soft pat to assure them. Most patients will not understand medical terms. Assist them by explaining the examination and answering their questions in common language.
c. Ability to Move. Disabled patients who move poorly or not at all may need assistance.
d. State of Health. Some patients may be just too sick to tolerate a lengthy physical examination. Do not leave very ill or debilitated patients alone; assist them to move and remain in the various positions and observe them for fatigue.
1-10. CLOSING
The practical nurse that is assigned to assist in the physical examination plays an important role in supporting both the patient and the physician or other health care providers. Upon completion, chart that the examination was done, by whom, the patient’s reaction, and any specimens sent to the lab or special procedures to be followed.