LESSON OBJECTIVES
2-1. Select the principles, supplies and equipment, and procedures, which apply to obtaining a sample for throat culture.
2-2. Select the principles, supplies and equipment, and procedures, which apply to obtaining a sputum specimen.
2-3. Select the principles, supplies and equipment, and procedures that apply to obtaining a stool specimen.
2-4. Identify the steps of the procedure for correctly obtaining a midstream urine specimen, a 24-hour urine collection, and urine for a pregnancy test.
2-5. Identify abnormalities in the color and odor of urine.
2-6. Select the reason for obtaining a blood culture.
2-1. INTRODUCTION
One means of gathering information about the patient’s health status is by identifying pathogens and analyzing urine, blood, sputum, and feces. As a practical nurse, you may be responsible for collecting and labeling specimen for analysis and ensuring their delivery to the lab. For self-protection and to prevent the spread of disease, wear gloves whenever you work with body fluids. Washing your hands carefully also prevents the spread of disease.
2-2. THROAT CULTURE
Throat cultures are done to isolate and identify any pathogens, which may be medium. The slide or medium is incubated in the laboratory to determine which organisms causing a throat disorder. A sample of mucus and secretions from the back of the throat is collected on a cotton-tipped applicator and applied to a slide or culture are present. A determination of which drug is most effective against a particular organism may be done also. A full culture and sensitivity test takes several days because the organisms must have time to grow. If strep infection is suspected a quick strep test may be done, so that antibiotic therapy can be started immediately.
2-3. SUPPLIES AND EQUIPMENT
The supplies and equipment required to obtain a sample for throat culture are:
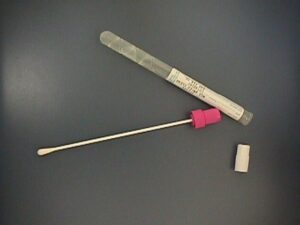
a. Sterile cotton-tipped applicator specimen collection kit (culturette).
b. Tongue depressor.
c. Laboratory request form.
d. Flashlight.
2-4. PROCEDURE FOR A THROAT CULTURE
Always wash your hands before the procedure. Explain to the patient what you are going to do. Have the patient sit comfortably on a bed or chair and tilt his head back.
a. Use the flashlight to illuminate the back of the throat. Check for inflamed areas using the tongue depressor.
b. Ask the patient to say “Ahhh” as you swab the tonsillar areas from side to side. Be sure to include any inflamed of purulent sites.
c. Avoid touching the tongue, cheeks, or teeth with the applicator, as this will contaminate it with oral bacteria.
d. Place the cotton-tipped applicator into the culture tube immediately.
e. Label the culture tube with the patient’s name, SSN, and ward number if applicable.
f. Complete the request form (SF 553) with the following information:
(1) Patient’s name.
(2) Patient’s rank or status.
(3) Family member prefix and sponsor’s social security number.
(4) Ward number if inpatient, or phone number if outpatient.
(5) Source of the specimen (that is, throat).
(6) Any antibiotics the patient is taking.
(7) Date and time the specimen was obtained.
(8) Name of the physician who ordered the culture.
2-5. SPUTUM SPECIMEN
For some respiratory disorders, a sputum specimen is obtained for culture or other examination to determine if any pathogens or blood are present. The specimen should be collected early in the morning before the patient eats, brushes his teeth, or uses mouthwash. The specimen is more likely to contain sputum at this time, rather than just saliva. Specimens are often taken for three consecutive days because it is difficult for the patient to cough up enough sputum at one time, and an organism may be missed if only one culture is done.
2-6. SUPPLIES AND EQUIPMENT
Supplies and equipment required to collect a sputum specimen are
a. Sterile container with tight-fitting lid.
b. Box of tissues.
c. Gloves.
d. Laboratory request form (SF 553).
2-7. PROCEDURE FOR SPUTUM SPECIMEN
a. Wash your hands and gather the equipment.
b. Provide privacy for the patient and explain the procedure. Place the tissues nearby and have the patient rinse his mouth with clear water to remove any food particles.
c. Assist the patient to a sitting position, if necessary and ask him to cough deeply and spit into the container. Tell the patient to avoid touching the inside of the container because it is sterile.
d. A sputum specimen is considered highly contaminated and must be treated with caution. To prevent contamination by particles in the air, keep the container closed until the patient is ready to spit into it. Close the container immediately after collecting the specimen to prevent the spread of any organisms from the specimen. Offer tissues for the patient to wipe his mouth.
e. Wash your hands, label the container, and complete the laboratory request form. Take the specimen to the laboratory immediately; allowing the specimen to remain in a warm place will result in overgrowth of any organisms that may be present.
f. Record the amount, consistency, and color of the sputum collected, as well as the time and date in the nursing notes.
2-8. STOOL SPECIMEN
Stool specimen are collected for many examinations. The most common is the ova and parasites test, a microscopic examination of feces for detecting parasites such as amebas or worms. Stools specimen are often tested for blood. Guaiac or HemOccult test may be done in the laboratory but are sometimes done at the nursing station to test a stool for occult blood.
2-9. SUPPLIES AND EQUIPMENT
Supplies and equipment required to collect a stool specimen are
a. Gloves
b. Clean bedpan and cover (an extra bedpan or urinal if the patient must void).
c. Specimen container and lid.
d. Wooden tongue blades.
e. Paper bag for used tongue blades.
e. Labels.
f. Plastic bag for transport of container with specimen to laboratory.
2-10. PROCEDURE FOR STOOL SPECIMEN
a. Explain the reason for the test and the procedure to the patient. Ask the patient to tell you when he feels the urge to have a bowel movement.
b. Wear gloves when handling any bodily discharge (see universal precautions in the introduction to this subcourse).
c. Give the bedpan when the patient is ready. If the patient wants to urinate first, give a male the urinal or give a female the extra bedpan.
d. Remove the bedpan. Use the tongue blade to transfer a portion of the feces to the specimen container. Do not touch the specimen because it is contaminated. It is not necessary to keep this specimen sterile however, because the gastrointestinal tract is not sterile.
e. Cover the container and label it with the patient’s name and social security number.
f. Complete the appropriate laboratory request form, noting any special examination ordered.
g. Take the specimen to the lab immediately; examination for parasites, ova, and organisms must be made while the stool is warm.
h. If an infant’s stool is to be examined, place the diaper in a leakproof bag, label it, and take the diaper and request form to the lab immediately.
2-11. GUAIAC TEST
The purpose of this test, using guaiac as a reagent, is to detect the presence of occult blood (blood that appears from a nonspecific source, with obscure signs and symptoms), which is not visible. Each method of testing has a specific procedure, which must be followed to get accurate results. If it is done at the nursing station, instructions should be kept with the reagents used. Follow the manufacturer’s instructions or consult hospital standing operating procedures (SOP).
2-12. URINE SPECIMENS
Urinalysis is included in a health examination, and as part of the admission process for all inpatients. Simple urine tests, such as for sugar and acetone, are often performed by the nurse in the hospital or by the patient at home. Urine is assessed first for its physical appearance:
a. Color. Freshly voided urine is transparent and light amber in color. The amount and kinds of waste in the urine make it lighter or darker. Blood in the urine colors it; if the amount of blood in the urine is great, the urine will be red. During a flare-up of chronic nephritis, the small number of red blood cells present in the urine give it a smoky appearance.
b. Odor. Freshly voided urine has a characteristic odor. When urine stands, decomposition from bacterial activity gives it an ammonia-like odor. Refrigerate the urine sample if it is not to be examined at once.
2-13. MIDSTREAM URINE SPECIMEN
Midstream (clean-catch) urine collection is the most common method of obtaining urine specimens from adults, particularly men. This method allows a specimen, which is not contaminated from external sources to be obtained without catheterization.
a. Supplies and Equipment.
(1) Sterile specimen cup.
(2) Zephiran, a soap solution, or three antiseptic towelettes.
(3) Three cotton balls (to use with zephiran or soap solution).
(4) Laboratory request form.
b. Procedure.
(1) Instruct the patient to clean the urethral area thoroughly. This will prevent external bacteria from entering the specimen. The female should wipe from front to back to avoid contaminating the vaginal and urethral area from the anal area. She should clean each side with a separate cotton ball or towelette, then use the last one for the urethral area itself. The male should cleanse the penis, using the first cotton ball or towelette for the urethral meatus, the next cotton ball to clean the end of the penis, and the last to cleanse the urethral opening.
(2) Instruct the patient to void a small amount of urine into the toilet to rinse out the urethra, void the midstream urine into the specimen cup, and the last of the stream into the toilet. The midstream urine is considered to be bladder and kidney washings; the portion that the physician wants tested.
(3) Complete the laboratory request form, label the specimen container with patient identifying information, and send to the lab immediately. A delay in examining the specimen may cause a false result when bacterial determinations are to be made.
(4) Wash your hands and instruct the patient to do likewise.
(5) Record that the specimen was collected. Note any difficulties the patient had or if the urine had an abnormal appearance.
2-14. 24-HOUR URINE SPECIMEN
A 24-hour urine collection always begins with an empty bladder so that the urine collected is not “left over” from previous hours. This specimen shows the total amounts of wastes the kidneys are eliminating and the amount of each.
a. Supplies and Equipment.
(1) Large, clean bottle with cap or stopper.
(2) Measuring graduate.
(3) Bedpan or urinal.
(4) Refrigerated storage area.
(5) Gloves.
b. Procedure.
(1) Label the bottle with patient identifying information, the date, and time the collection begins and ends.
(2) Instruct the patient to void all urine into a bedpan or urinal. Measure each specimen of urine voided and pour into the refrigerated bottle. Wash your hands before and after each collection. Record each amount on the intake and output (I&O) sheet.
(3) Exactly 24-hours after beginning the collection, ask the patient to void. This will complete the specimen collection.
(4) Send the bottle and laboratory request form to the lab.
2-15. PREGNANCY URINE TEST
Most pregnancy tests are based on the fact that the hormone human chorionic gonadotropin (HCG) is secreted by the chorionic villi of the placenta. This hormone can be detected in small amounts in both the urine and the blood of a pregnant woman by the 15th day of pregnancy. Urine tests are available for home use and offer quick results with 90 percent to 95 percent accuracy.
a. Supplies and Equipment. Only a urine specimen cup is required.
b. Procedure.
(1) Instruct the patient to void the very first urine when she gets up in the morning into the specimen cup.
(2) Label the specimen cup with the patient’s identifying information, complete a laboratory request form (Chemistry I, SF 546) requesting an HCG test and send both to the lab.
(3) Only the physician or a registered nurse should tell the patient the results of the test.
2-16. BLOOD CULTURES
Blood cultures are done to identify a disease-causing organism, especially in patients who have an elevated temperature for an unknown reason. Drawing blood from HIV positive patients is done in accordance with the hospital or clinic’s local policy (see universal precautions).
2-17. SUPPLIES AND EQUIPMENT
Supplies and equipment required for a blood culture are
a. Sterile syringe (20 cc) and three needles (usually 20 gauge).
b. Two blood culture bottles (one for anaerobic and one for aerobic specimens).
c. Betadine solution.
d. Sterile cotton balls or gauze pads.
e. Gloves.
f. Tourniquet.
g. Band-aid®.
h. Chux® (to protect the bed)
i. Laboratory request form.
2-18. PROCEDURE FOR BLOOD CULTURES
a. Explain the procedure and the reason for doing the procedure to the patient.
b. Gather all supplies and equipment and bring to the patient’s bedside.
c. Assist the patient to a comfortable position. If the patient is uncooperative or disoriented, get someone to help you.
d. Carefully wash your hands.
e. Clean the top of both culture bottles with betadine solution.
f. Put the needle on the syringe.
g. Apply the tourniquet.
h. Put on the gloves and clean the drawing site with betadine solution.
i. Draw at least 10 cc of blood from the patient (5 cc is needed for each bottle).
j. Loosen the tourniquet.
k. Remove the syringe and needle while applying pressure to the venipuncture site with the cotton ball or gauze pad. Have the patient apply pressure to the site.
l. Replace the needle on the syringe with another sterile needle.
m. Inject 5 cc of blood into the anaerobic bottle; do not allow air to enter the bottle.
n. Replace the needle on the syringe with another sterile needle.
o. Inject 5 cc of blood into the aerobic bottle and while the needle is still in the bottle, disconnect it from the syringe so that air enters the aerobic bottle.
p. Gently mix the blood with the solution in both bottles.
q. Label both bottles with patient identifying information and the type of culture hat is, aerobic or anaerobic).
r. Complete laboratory request forms and send the specimens to the laboratory immediately.
s. Place a band-aid over the patient’s venipuncture site.
2-19. CLOSING
The role you play in collecting and labeling specimens and ensuring their timely delivery to the lab for analysis is a very important one. Carefully follow the steps of each procedure to prevent contaminating the specimen or spreading infection. Always document that the procedure was done and by whom.
