1-50. AMPUTATION
a. Surgical amputation of a limb is done to remove dead or unhealthy tissue that cannot be treated by any other means. In many cases, amputation is done as a lifesaving measure. Reasons for amputation include the following.
(1) Trauma. Injuries from combat, explosions, crushing injuries, and other trauma may necessitate amputation if the extent of the injury is quite severe.
(2) Thermal injuries. Electrical injuries, frostbite, and burns may be severe enough for amputation to be necessary.
(3) Peripheral vascular disease. Most nonemergency amputations are done because of severely compromised circulation due to vascular disease.
(4) Infection. In case of severe infection of the bone or soft tissue of a limb, amputation may be required. Osteomyelitis and gas gangrene are two such examples.
(5) Congenital deformity. In some cases, amputation is advised to remove a deformed and useless limb to permit the fitting of a functional prosthesis.
(6) Tumors. Malignancy that does not respond to any form of therapy and threatens to metastasize throughout the bone often results in amputation of all or part of a limb.
(7) Chronic pain. An extremity may be painful because of a circulatory problem or other disease process. Amputation may be indicated if the pain cannot be controlled in any other way.
b. Whatever the reason, amputation is a major operation. Long-range planning is necessary for the patient’s rehabilitation; continuous care and teaching are necessary while the patient recovers.
1-51. THE SITE OF AMPUTATION
a. The exact location for the amputation of a limb is based on several factors. The physician will always strive to preserve as much of the limb as possible, but there are other considerations involved in the decision. For example:
(1) The blood supply available to the remaining limb.
(2) The functional ability of the remaining limb.
(3) The fitting of a functional prosthesis.
(4) The patient’s age and overall physical condition.
(5) The patient’s muscle strength.
(6) The patient’s ability to learn.
b. The usual sites for amputation of a lower extremity include the foot, the ankle, below the knee (BKA), above the knee (AKA), at the hip (hip disarticulation), or at the pelvis (hemipelvectomy). Usual sites involved in amputation of part of an upper extremity include the fingers, at the wrist, below the elbow (BEA), above the elbow (AEA), and at the shoulder (shoulder disarticulation). The shoulder disarticulation, hip disarticulation, and hemipelvectomy are normally done only in cases of extensive injuries, malignancy, or gangrene. They are disabling and traumatic procedures, and done only as a last recourse.
c. Two basic types of amputation procedures are utilized. They are referred to as open, or guillotine amputation and closed, or flap amputation.
(1) The open amputation is performed when infection is present or likely to develop due to the circumstances of the injury or amputation. Tissue and bone are severed at the same level, and the wound is not closed, but left open to drain. Bulky dressings cover the stump end.
(2) The closed amputation is the preferred method as it usually heals faster and allows the patient to be fitted for and begin using a prosthetic device much sooner. When the tissue and bone are severed, skin flaps are left to cover the stump end. Drains are placed in the wound and the skin flaps are sutured.
1-52. NURSING CARE AND PATIENT EDUCATION
a. Preoperative care and patient education can be done in cases of elective amputation. There is time to prepare the patient for what lies ahead. In the case of a traumatic amputation, this may not be possible. Preoperative nursing care and patient education for the patient about to undergo amputation of all or part of a limb includes the following.
(1) Build the patient’s strength by implementing muscular exercises for the unaffected limbs.
(2) Improve the patient’s nutritional status by encouraging a balanced diet high in vitamins and minerals and with adequate protein to enhance wound healing. Maintain adequate hydration.
(3) Follow the physician’s orders for therapeutic measures used to stabilize any chronic medical conditions such as diabetes, hypertension, or any other condition that may interfere with surgery or rehabilitation.
(4) If ordered, arrange preoperative counseling with the physical therapist. If a mobilization aid such as a walker or crutches is to be used postoperatively, it is easier to provide instruction in the preoperative period. The physical therapist will also inform the patient about his postoperative rehabilitation program.
(5) If authorized by the physician, schedule a visit from the prosthetic specialist. This may help to alleviate some of the patient’s anxieties about the fitting and wear of prosthetic devices.
b. Postoperative nursing care involves routine nursing observation, pain control, positioning and exercise, stump conditioning, and patient education. Patient education should be done in conjunction with all nursing interventions.
(1) Monitor the patient’s vital signs closely for changes in pulse or blood pressure that may indicate hemorrhage under the bulky dressing. A temperature elevation may indicate the presence of infection.
(2) Check the stump dressing regularly. Evidence of bloody drainage should be marked with date and time, and excessive bleeding reported to the physician. Check the proximal end of the stump dressing for swelling. The dressings are applied to provide some compression of the stump, but a dressing that is too tight may cause ischemia at the stump end.
(3) Observe the patient for pain. Pain medication may be required for several days post-operatively. Some patients experience a phenomenon known as “phantom pain” or “phantom sensation” in which they “feel” the lost limb.
(4) Maintain the prescribed position of the stump. Depending upon the type of procedure used, the extremity may be in a splint, in traction, or elevated on pillows. Proper positioning will prevent contracture of the involved muscles.
(5) Encourage prescribed exercises to preserve the range of motion in the affected limb and to strengthen the remaining limbs.
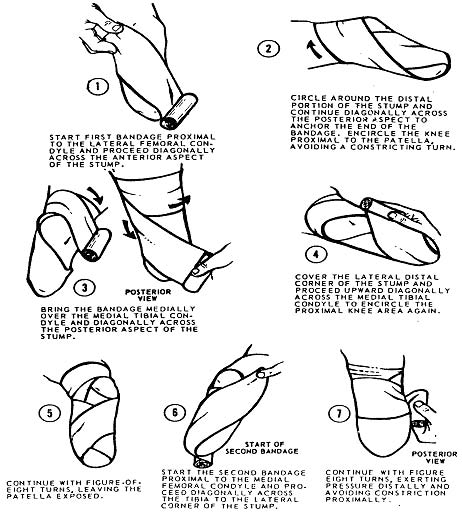
(6) Remove and reapply the bandage. When the wound is healed, the stump must be conditioned and shaped for the proper fitting of a prosthesis. A special bandaging technique is used to shrink and mold the stump to a smooth, conical shape. During the shaping process, the bandage is worn day and night. It is customarily removed and reapplied twice daily or as ordered by the physician. Different methods are employed in wrapping the bandage, but the objective is the same: to provide equal, firm compression to the stump. A criss-cross or spiral pattern is used to avoid constricting the stump and interfering with circulation. One technique for wrapping a stump is illustrated in figure 1-20.
c. Patient education and quality nursing care are important, but the nursing staff must be aware of how the patient feels about the amputation. Trying to compensate for a lost limb is a difficult adjustment for anyone to make. It can easily produce feelings of uselessness or inadequacy in the patient. How “handicapped” the patient feels will depend upon how he adjusts to the loss. Some patients may refuse to learn to care for the stump, or even look at it, while others may be eager to reach a speedy recovery. Each patient will require individualized assistance in learning to cope with his amputation. It is important for the nursing personnel to remember that any amputation results in a permanent loss that may interfere with the psychological, physical, or social needs of the individual.
