Hospital Corpsman Sickcall Screener's Handbook
BUMEDINST 6550:9A
Naval Hospital Great Lakes
1999
Orthopedics
Back Problems: Affects 85% of the population at some time.
Anatomy:
The spine is composed of 7 cervical, 12 thoracic, 5 lumbar vertebrae, and the sacrum. They are separated from each other by a disc that cushions the vertebrae. To understand the back you have to understand the anatomy and know how the vertebrae - disc - vertebrae unit work.
Looking from the side you can see a hole (foramen) that serves as a window through which a nerve root from the spinal cord exists. This nerve can be pinched if the disc herniates into the intervertebral foramen. This disturbs the muscular function and effects the deep tendon reflexes the nerve controls. Each nerve serves a different part of the body. Disc problems most often affect the L4, L5, and 51 nerve roots. Evaluating the function of these nerve roots is part of examining a person with back pain
Most back problems are due to muscle stain and involve the paravertebral (para - around) muscles, which include the latissimus dorsi and trapezious muscles.
Physical Examination:
With the patient standing: Check symmetry, curvatures, ROM (range of motion) include extension, flexion and side to side; gait, heel - toe walking (heel walk L-5, and tiptoe S-I), and look for paravertebral muscle spasm.
Note: A malingerer will complain of pain when pressing down on the head; and may have an abnormal gait or limp. Have patient walk backwards - it is impossible to limp backwards unless it is genuine.
With the Patient sitting: Check deep tendon reflexes (DTRs) - patellar (L4) and achilles (S-I). Check extension strength of the great toe (ability to pull it up against resistance L-5).
With the patient supine: Straight leg raising test - Raise the patients relaxed and straightened leg until pain occurs This places a stretch on nerve roots normally L-5. Then dorsiflex the foot, this will increase the pain if the nerve root is being compressed. Increased - in the affected leg when the opposite leg is raised (crossed straight leg raising sign) strongly confirms nerve root involvement.
|
 |
|
Operational Medicine CD
Text, images,
videos and manuals
The essential text for military healthcare providers
www.brooksidepress.org |
Lower Back Strain / Pain:
A painful condition involving the lower back, related to physical activity and may be recurrent.
S: Moderate pain in the lumbar area made worse by movement such as bending.
O: Tenderness and spasm of paravertebral muscle in the lumbar area with limited ROM.
Remainder of exam is normal - no nerve root involvement.
A: Lower Back Pain
P: Bed rest may be needed, heat to area, Motrin 800 mg TID, and a muscle relaxant like
Flexeril 10 mg TID.
Herniated Disc: A syndrome of severe back pain as a result of impingement of a nerve root by a bulging intervertebral disc.
S: Backache, worse with coughing, sneezing and movement. Pain may radiate into leg. May have numbness tingling or weakness in the lower leg.
O: Positive straight leg raise, decreased ROM, with altered strength and deep tendon reflexes (DTR).
A: Herniated Disc
P: Bed rest, Motrin, Flexeril, and referral to Ortho if not improved in 48 to 72 hours, may require surgery
KNEE PROBLEMS
A careful history makes the diagnosis!!!
-
Is there direct trauma or injury? If no go to #2. If so. What was the precise mechanism of injury -what happened?
-
Is it mechanical pain that is related directly to use of the knee? Worse "with bending, walking, climbing stairs, or running"
-
Is there a history of effusion?
-
Does it:
-
lock -fixed in one position ? (Miniscal tear)
-
click - usually normal with deep knee bends.
-
buckle - does knee give out? (ligament instability, miniscal tear, or patellar dislocation)
-
Pseudo buckle - gives out due to pain usually due to patellar - Femoral syndrome. No ligament instability.
-
What factors cause, worsen, or relieve pain?
ANATOMY
-
Bones: Femur with distal medial and lateral epicondyles, Patella, Tibia with medial and lateral condyles, Tibial tubical - attachment of the quads and the Fibula
-
Muscles:
-
Quadriceps (made up of 4 muscles). They form a tendon that envelops the patella. Below the patella it is call the patellar tendon and it inserts into the tibial tubical, anchoring the quads to the tibia. The quadriceps cause knee extension
-
Hamstring muscles Found in the back of the thigh, they cause flexion of the knee.
-
Parts of the Knee Joint:
-
Ligaments: (hold bones together)
Collateral Ligaments - lateral and medial
Cruciate Ligaments - Anterior and posterior
-
Menisci: Distributes weight over the surface of the joint and functions as shock absorbers or cushions.
-
Patella: Our kneecap rides in the groove between the femoral condyles.
-
Bursa: fibrous sacs of fluid that reduce friction between bones, ligaments and tendons.
PHYSICAL EXAMINATION
-
With patient standing: Check - active ROM - The patient uses his own muscles to complete ROM.
Note: Passive ROM involves the examiner moving the patient's limbs through the ROM. This is useful when the patient can not perform active ROM.
-
With patient seated:
-
inspect knee - swelling, tenderness, deformity
-
palpate - check patellar tendon, tibial tubical, and joint line.
-
With patient sitting down:
-
Compare knees - loss of "hollows" swelling superior to the patella is usually caused by an effusion
-
Patella movement, tenderness
-
Check extension (passive ROM)
-
Test medial and lateral collateral ligaments; Valgus (knock knees). Varus (bowed legs)
-
Examine with McMurray or Apley tests to detect a torn meniscus.
COMMON KNEE PROBLEMS
-
Osgood Schlatters Patellar Tendinitis Pain over the tibial tubercle and into the patellar tendon. Actual injury occurs in early teens with the pulling of the patellar tendon out of its attachment at the tibial tubical. This heals with a large calcium deposit below the knee. The tendinitis is a re-inflammation of this old injury. Pain with extension of lower leg.
Treated with rest and anti-inflammatories
-
Patellar - Femoral Syndrome: Pain resulting from overuse of the joint. The mechanical movement of the patella between the femoral condyles on flexion / extension causes inflammation. Affected by weakened quadriceps and abnormal tracking of the patella. There is pain in and around the patella associated with crepitus. Treated with rest and anti-inflammatories.
-
Ligament Strain: Stretching of either anterior or posterior cruciates or medial or lateral collateral ligaments (Remember that combined ligament injury is common). Pain, mild swelling and laxity of the affected ligaments, and weakness. Note: a tear of a ligament will produce a severe effusion or swelling, a strain will not.
Treatment: rest, no weight bearing for 3-5 days, use crutches. Anti-inflammatories, limited duty for 2 to 3 weeks
-
Meniscus Tear: Usually caused by a rotatory mechanism of injury without a direct blow. Sudden onset of localized knee pain may lock, buckle or click. Severe swelling, weakness, and unable to bear weight. On exam severe effusion with tenderness over the joint line. Limited ROM. Positive McMurray’ test.
Refer to orthopedics, crutches, and anti-inflammatories.
-
Acute Arthritis: (usually infectious)
-
Cellulitis: due to bacterial infection or Gonococcal infection. -
Gout:
uric acid level increases Joint is tender, is hot, and swollen. No history of injury or trauma. Refer to MD or PA. Orthopedic consultation.
III. ANKLE AND FOOT
Anatomy:
There are seven tarsal bones. Two are very important. The CALCANEUS (the heel bone) is the largest and forms the attachment for the muscles of the calf of the leg via the achilles tendon. The TALUS rests on the calcaneus, the top is rounded for articulation with the tibia and forms the ankle joint. The talus bears the weight of the whole body which is transferred to the foot. The remaining bones of the foot are the phalanges, metatarsals, and the tarsal bones.
The ankle joint is made up of the talus, on top of which rests the tibia. At the sides of the talus are the malleoli of the tibia and fibula. They sit astride the talus like the legs of a rider over a saddle. The joint is held together by ligaments. The three important ligaments of the lateral ankle are:
-
Anterior Talofibular Ligament
-
Posterior Talofibular Ligament
-
Calcanofibular Ligament
These are important to know because 85% of ankle sprains involve the lateral ligaments. (Note: The names of the ligaments are made up from the two bones to which they attach)
The ligaments of the medial ankle arc grouped into one broad strong ligament - the deltoid ligament
Physical Examination:
Precise terms are used to describe both the anatomy and the location of injury Know the following
-
Proximal - Toward or nearest the point of attachment, or nearest the center of the body
-
Distal -Away from or furthest from the center of the body or point of attachment.
-
Extension-- A movement which brings the members of a limb into or toward a straight condition (straightening the joint)
-
Flexion - The act of bending upon itself (bending of the elbow is flexion)
-
Plantar - Refers to the bottom surface of the foot
-
Dorsal Refers to the top of the foot
-
Medial Malleolus - The part of the tibia that forms the inner or medial part of the ankle joint
-
Lateral Malleolus - The part of the fibula that covers the talus laterally.
-
Plantar Flexion - Downward flexion of the joint- an action accomplished by the gastronemous muscle via the achilles tendon.
-
Dorsiflexion - An action that brings the foot up.
-
Inversion - the movement of the sole of the foot inward (medially) so that the soles face toward each other.
-
Eversion - the movement of the sole outward (laterally) so that the soles face away from each other.
-
Abduction - the lateral movement of the limbs away from the body
-
Adduction - the movement of the limb toward the body after abduction
Ankle and Foot Examination:
Inspection: Look for swelling, redness, injury, deformity, or flat feet (pes planus).
Palpation: Feel for tenderness, swelling, heat, crepitus, check medial and lateral malleoli.
Range of Motion:
-
Inversion / eversion
-
Dorsiflexion/ plantar flexion
-
Abduction/adduction
-
Flexion/ extension of toes.
Muscles and Tendons:
-
Test strength with resistance of dorsiflexion/ planar flexion
-
Check Achilles tendon with the squeeze test
-
Check gait- walk on heels and toes
-
Check calf muscles by hopping up and down on the ball of foot
If patient lands flat footed their is weakness in the calf muscles
Neurological Testing: Check sensation to foot with pin prick or sharp / dull test with a paper clip.
See Neurology session for details.
Ankle Sprain: Indicates ligament injury. The anterior talofibular ligament is most commonly injured with point tenderness anterior to the lateral malleolus.
S: Painful swollen ankle, may not be able to bear weight
O: Tender over anterior lateral malleolus, swelling, ecchymosis (a blue-black discoloration due to bleeding into tissue). Decreased ROM.
A: Ankle Sprain
P: May need splint, and crutches if severe.
RICE Therapy: Rest, Ice, Compression, Elevation. Motrin
800 mg TID
Hand and Wrist
Precise terms for the hand and wrist:
Palmer (or volar) - the anterior surface of the hand.
Dorsal - the posterior surface of the hand.
Ulnar - toward the ulna or little finger
Note: Radial and ulnar are preferred because of the confusion over medial and lateral.
Pronation - the act of turning the hand so that the palm faces downward or backwards.
Supination - to turn the forearm or hand so that the palm faces upward
Numbering of the fingers: 1 = thumb, 2 = index finger, 3= long finger, 4 = ring finger, 5 = small finger
Bones of the hand:
Phalanges - distal, middle and proximal phalanges.
The joints in between the phalanges are named:
DIP - Distal interphalangeal joint
PIP - Proximal interphalangeal joint
MCP or MC - Metacarpophalangeal joint, where the metacarpals meet the phalanges
Nerves: The hand is supplied by three nerves - the median, the ulnar, and the radial nerves.
With no more than a paperclip an accurate test for sensation can be carried out. An injured nerve makes its presence known in three ways
-
Loss of sensation
-
Loss of motor function
-
Loss of sweating- if a nerve is lacerated the skin immediately becomes dry, so feel the skin.
Sensation is tested using the two - point discrimination test. Use a paper clip with the points 5mm apart. Press lightly against the skin, just enough to dent the skin along the sides of the fingers never across the finger.
Hand Examination:
Inspection: swelling, redness, injury, deformity.
Palpation: Tenderness, swelling, heat, crepitus.
Active ROM: Make a fist, flex the wrist, open the hand and extend the wrist, spread fingers apart and bring back together. Thumb has 4 movements - up, down, and side to side.
Test Muscle Strength:
-
Grip strength - patient squeezes your two fingers in his hand.
-
Pinch mechanism - the patient's thumb and index finger are pinched together to make a ring, insert your index finger and pull
-
Test Tendons of the hands (common to injure with laceration):
-
Check ability to flex DIPS
-
Check ability to flex PIPS
-
Check ability to flex MCPs
-
Check thumb for abduction (moving thumb away from the palm)
-
Check thumb for adduction (moving thumb toward the palm)
Neuro Exam: Sensory - two point discrimination
Ulnar C-8: test 5th finger
Radial C-6: test back of hand (radial side, dorsum)
Medial C-7: test the index finger on the palmar (volar) surface.
Motor:
C-6: Radial - Extension of wrist
C-7: Medial - Wrist flexion
C-8: Ulnar - Thumb adduction
Common Hand Problems:
1. Fracture of the Navicular (scaphoid): The most common of carpal fractures. Treatment is complicated if not found early however, it may not be initially seen on X-ray. Therefore if the patient has selling and tenderness localized in the anatomical snuff box after injury, it is treated as a fracture. Splint with a thumb spica cast and repeat X-rays in 2 weeks with the cast off looking for avisible fracture line. If fractured refer to orthopedics.
2. Boxer’s Fracture: Fracture of the fifth metacarpal causes the distal head of the MC to angulate toward the palm, usually the result of hitting something with the fist. Treated with an ulnar gutter splint with the hand and wrist in a functional position for three weeks.
3. SubunguaI Hematoma (under the nail): Common after hitting the distal finger or as a result of a crush type injury and may be associated with fracture of the distal phalanx. Decompression - relieving the pressure caused by bleeding under the nail - will relieve much of the pain. A hot paperclip held by a hemostat is pushed through the nail allowing drainage. This may convert a closed fracture into an open one therefore two days of antibiotic coverage is necessary.
Dicloxacillin or Erythromycin 250mg qid.
4. Paronychia: This is an abscess of the skin around the base of the nail and may extend under the nail. This is only drained by incision if pus is visible. If pus is not seen and only erythema, swelling and tenderness are present, treat with warm, moist compresses, elevation, and antibiotics
(Dicloxacillin or Erythromycin
250 mg QID).
SHOULDER
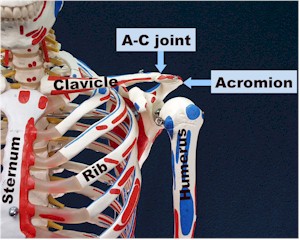
The shoulder is a complex arrangement of 3 bones held together by muscles, tendons, and ligaments. The clavicle attaches the shoulder to the sternum and holds the shoulder out from the trunk forming the sternoclavicular joint. From behind the shoulder joint the scapula forms two projections, the acromion and the coracoid which together with the clavicle form the glenoid fossa, a socket into which the ball like head of the humerus is cradled. This combination forms the shoulder or glenohumeral joint. A third joint is formed where the acromian process from the scapula meets the distal clavicle, the acromioclavicular (A-C) joint. The rotator cuff stabilizes the glenohumeral joint and is made up of a group of muscles: The suprapinatus, infraspinatus, teres minor, and subscapulris. The biceps tendon is held in a groove in the humerus and attaches under the rotator cuff. Bicep tendinitis with pain to the area of the biceptal groove is a common problem. Injuries may include a roptator cuff tendinitis or tear, A-C joint separation from a fall on the shoulder, and dislocation or glenohumeral instability.
Physical Examination:
Inspection: Swelling, deformity, redness, asymmetry.
Palpation: Feel for deformity, tenderness, effusion or swelling, or crepitus
Identify the clavicle, A-C joint, bicepital groove, sternoclavicular joint
Range of Motion:
Active: Ask patient to
-
Raise both arms to a vertical position at the sides of the head - both with abduction and forward flexion.
-
Scratch his back - first reaching behind the neck and then reaching behind to the small of the back.
Passive: Test for shoulder flexion, extension, abduction, adducion, external and internal rotation
Muscle Strength:
-
Check shoulder abductors with arm extended straight out from the side push downward while patient resists.
Neurological Examination: Check sensation with pin prick. Do an entire neurological examination of the hand as presented in the neurology lesson.
Common Causes of Shoulder Pain:
Rotator Cuff Tendinitis: The most common cause of shoulder pain. Caused by the rotator cuff getting pinched under the acromian process. Patients are usually after 40 years of age and are athletical1y active.
Rotator Cuff Tear: Usually after 40 years of age, caused by an injury. Abduction is severely impaired. As the patient tries to abduct the arm, a characteristic shoulder shrug is produced.
Bicipital Tendinitis: Inflammation of the biceps tendon producing pain in the bicipital groove.
Dislocation: Tends to occur after falling on an outstretched arm. 95% are anterior dislocation and the humeral head is palpable anteriorly. Reduce as soon as possible. Refer to MD/PA.
FRACTURES
Any break in the continuity of a bone as a result of trauma.
S: Recent trauma, or repeated vigorous physical activity. Pain over affected area. May have swelling, bruising (ecchymosis), deformity, and restricted movement.
O: tenderness at the site, may have edema/swelling, crepitus, deformity, loss of motion, and restricted use of involved area. Check pulses and neurological status. Stress fractures may have no other findings except for worse pain with activity and relieved by rest.
A: Fracture
P: X-rays usually required to confirm diagnosis. Stress fractures may require a bone scan. Minor, non-displaced fractures: Immobilization, no weight bearing, pain medication and Orthopedic referral. Major fracture: Immediate orthopedic referral.
|
|
Approved for public release;
Distribution is unlimited.
The listing of any non-Federal product in this CD is not an endorsement of the
product itself, but simply an acknowledgement of the source.
Bureau of Medicine and Surgery
Department of the Navy
2300 E Street NW
Washington, D.C
20372-5300 |
Operational Medicine
Health Care in Military Settings
CAPT Michael John Hughey, MC, USNR
NAVMED P-5139
January 1, 2001 |
United States Special Operations
Command
7701 Tampa Point Blvd.
MacDill AFB, Florida
33621-5323 |
*This web version is provided by
The Brookside Associates Medical Education Division. It contains
original contents from the official US Navy NAVMED P-5139, but has been
reformatted for web access and includes advertising and links that were not
present in the original version. This web version has not been approved by the
Department of the Navy or the Department of Defense. The presence of any
advertising on these pages does not constitute an endorsement of that product or
service by either the US Department of Defense or the Brookside Associates. The
Brookside Associates is a private organization, not affiliated with the United
States Department of Defense.
Contact Us · Other
Brookside Products
|
|
Operational Medicine 2001
Contents
|

|
 |
|
FMST Student Manual Multimedia CD
30 Operational Medicine Textbooks/Manuals
30 Operational Medicine Videos
"Just in Time" Initial and Refresher Training
Durable Field-Deployable Storage Case |
|