Endometriosis
Cause · Incidence
· Symptoms
· Physical Findings/Lab
· Diagnosis
· Natural History
· Association with Infertility
· Principles of Management
· Birth Control Pills
· GNRH Antagonists
· Danazol
· Progestins
· Conservative Surgery
· Definitive Surgery
· The
Military Setting
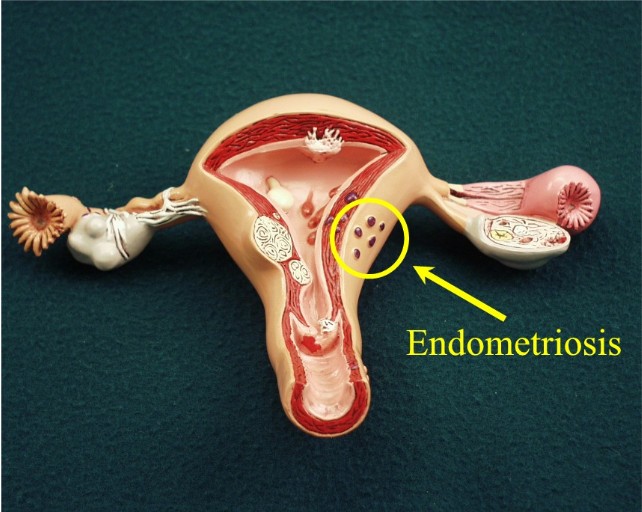
Endometriosis is a common gynecologic problem. It is defined as the
abnormal location of normal endometrial tissue in the body, and is
associated with pain, scar tissue formation, and infertility.
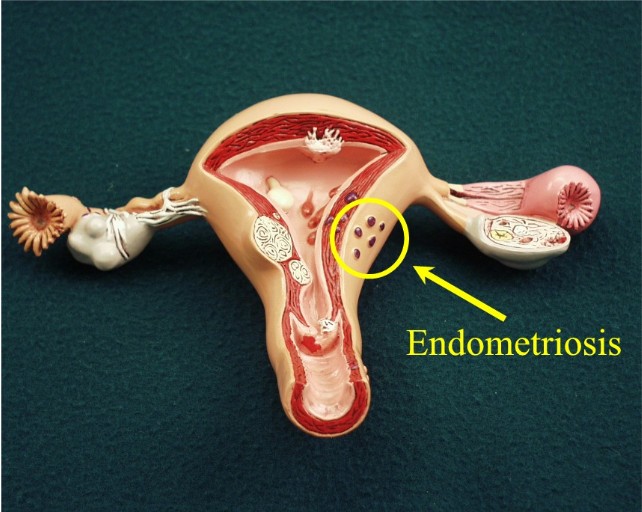 Endometrium is normally located within the uterine cavity, lining the
interior walls of the uterus. In response to the normal cyclic hormonal
events, the lining thickens, then splits off its most superficial layer,
which is shed during the menstrual flow. Endometrium is normally located within the uterine cavity, lining the
interior walls of the uterus. In response to the normal cyclic hormonal
events, the lining thickens, then splits off its most superficial layer,
which is shed during the menstrual flow.
Women with endometriosis have patches of "normal" endometrium located
elsewhere in the body. The most common locations for these implants are
on the:
However, endometriosis can be found virtually anywhere in the body,
including sites quite remote from the pelvis (lung, vertebra, skin).

Cause of Endometriosis
The specific cause is not known, but several theories can, in part,
explain the existence of endometriosis. Two of the more popular theories
are:
-
Implantation Theory: During menses, some
reflux of menstrual products back through the fallopian tubes occurs.
Viable endometrium can land on a favorable site and, if tolerated by
the patient's immune system, can establish enough of a blood supply to
live and respond to the cyclic ovarian hormones.
-
Coelomic Metaplasia Theory: The peritoneal cavity
contains some cells that have retained their undifferentiated nature
and, given the proper stimulus, may grow and differentiate into
endometrial cells.
Incidence
The incidence of endometriosis in the general population is not known.
For women undergoing gynecologic surgery, the incidence varies,
undoubtedly depending on the population, type of surgical procedure, and
the skill and diligence with which endometriosis is sought. The
frequency with which endometriosis is found varies from:
-
6% to 43% of women undergoing sterilization
-
12% to 32% of women undergoing laparoscopy for pelvic pain
-
21% to 48% of women undergoing laparoscopy for infertility
-
50% of teenagers undergoing laparoscopy for chronic pelvic pain or
dysmenorrhea
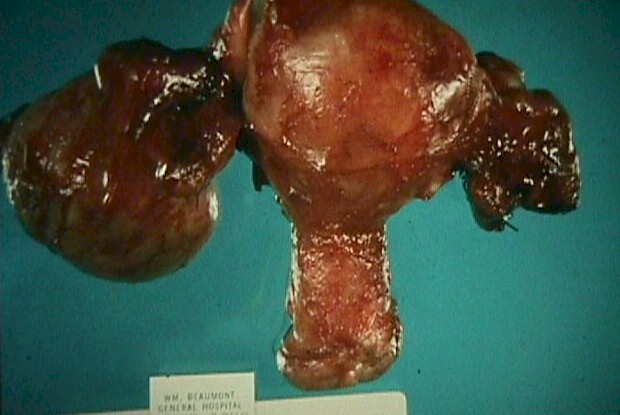 |
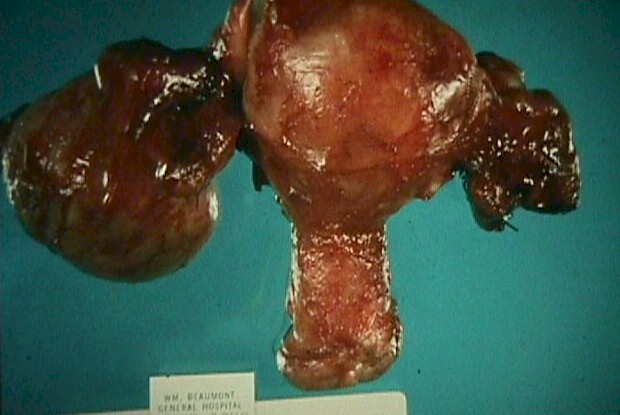
Endometrioma of Right Ovary |
Symptoms
Classically, women with symptomatic endometriosis present with a chronic
(more than 6 month) history of steadily worsening pelvic pain. It is
worse with menses and sometimes worse with ovulation. It may be focal or
diffuse, but its location is usually constant. The pain may be aching,
cramping, or both at different times.
A second classical symptom is
painful intercourse on deep penetration. The patient will tell you she
feels him hitting something deep inside that is very tender. If she
re-directs the angle of his thrusting or limits the depth of his
penetration, she may be able to avoid the pain.
Less common is painful bowel movements. If implants are located on
the rectosigmoid or close to it (uterosacral ligaments), then she may
experience pain while actually passing her stool.
About half of the women who are demonstrated to have endometriosis
have no symptoms at all.
Physical Findings and Lab
Classical physical findings include:
-
Unusual tenderness and thickness (a dough-like consistency) in the
adnexal areas.
-
Tender nodules along the uterosacral ligament, usually appreciated
best on combined recto-vaginal bimanual exam.
-
Tender nodules at the junction of the bladder and the uterus.
-
Tender nodules over the uterine corpus.
Many women (particularly those with asymptomatic endometriosis) have
no positive physical findings.
There are no laboratory tests that are specific for endometriosis.
However:
-
Some women with endometrioisis have a persistent complex or solid
adnexal mass on ultrasound, CT or MRI. These endometriomas can assume
a passable resemblance to almost any adnexal neoplasm. This means that
the differential diagnosis for virtually any adnexal mass would
include endometriosis.
-
Most women with endometriosis will have an elevated serum CA-125.
This chemical is released any time there is peritoneal irritation from
any source.
Diagnosis
The diagnosis can be established clinically, surgically, and/or
histologically.
-
Clinical Diagnosis is established by a convincing history that is
reasonably close to the classical description, accompanied by physical
findings that are very suggestive of endometriosis. Making a clinical
diagnosis has the advantage of avoiding surgery, but the disadvantage
of being wrong from time to time.
-
Surgical Diagnosis is obtained by visualizing typical
endometriosis implants in the typical places endometriosis tends to
grow in. The visual indicators of endometriosis include deep red,
slightly hemorrhagic sites, white puckering of the peritoneum, brown
"powder burns," translucent blebs, defects in the peritoneum, polypoid
growths, and dense scarring of the ovaries, tubes and cul-de-sacs.
This may be done through laparoscopy or laparotomy. A surgical
diagnosis is more reliable than a clinical diagnosis, but not always
consistent with a histologic diagnosis.
-
Histologic diagnosis depends on the microscopic confirmation of
endometrial glandular and stromal cells in an ectopic location. This
is highly specific, but requires surgical risk to obtain the specimen.
At times, the endometrial cells can be elusive, particularly if the
patient has been treated with medications to suppress endometriosis.
It is not uncommon for there to be obvious endometriosis at the time
of surgery, yet the biopsies will be negative.
Some gynecologists feel that before initiating therapy, all patients
in whom the diagnosis of endometriosis is entertained should undergo
laparoscopy. Others feel that this is an unnecessary and dangerous
over-reaction and reserve laparoscopy for those in whom conservative
management has failed or for whom there are other indications for
laparoscopy, such as infertility.
Natural History
Untreated, endometriosis can worsen, regress or stay the same, but more
often is progressive. Some life events have a favorable influence on
endometriosis. Pregnancy and breast-feeding favorably influence
endometriosis. Birth control pills, even if taken cyclically, usually
make endometriosis better (particularly minimal, mild or moderate).
At
menopause, deprived of its hormonal support, endometriosis usually
regresses, regardless of whether or not estrogen replacement therapy is
used.
Endometriosis has no malignant potential. It is a problem only
because of its potential for causing pain and scarring, and its
association with infertility.
Association with Infertility
Generations of gynecologists have recognized that among infertile women,
endometriosis is relatively common. Probably between 25% and 50% of
infertile women will have at least some degree of endometriosis present.
It is easy to understand how someone with severe endometriosis,
including dense pelvic adhesions, might experience difficulty achieving
a pregnancy. More difficult to understand is why someone with one tiny
endomtriosis implant on the sigmoid colon would also experience
infertility. The answer may lie in the complexity of endometriosis.
Rather than blaming endometriosis for the infertility, it is
certainly possible that there is some other, yet unexplained factor,
that predisposes the woman towards developing endometriosis and also
predisposes her toward infertility. Severe cervical stenosis, for
example could promote a large amount of retrograde menstruation (setting
her up for endometriosis) and also interfere with normal sperm transport
through the cervix (decreasing her chance of fertility).
Principles of Management
There is no single best management for all women with endometriosis.
Treatment must be individualized. The primary factors that we consider,
however are:
-
The need for preserving childbearing capacity
-
The severity of her symptoms
-
Presence or absence of infertility as a clinical concern for her.
-
Age
A 35 year old woman with severe symptoms and no desire for any
further childbearing might be best served by a hysterectomy. The same
woman at age 50 might prefer to go with medical therapy until menopause,
when the symptoms will go away. The same woman at age 40, but with mild
symptoms might do well on birth control pills.
Birth Control Pills
Birth control pills exert a number of beneficial effects, particularly
on mild or moderate endometriosis. They generally:
-
Reduce the heaviness of the menstrual and its duration, reducing
the amount of retrograde menstrual products.
-
Provide a powerful decidualizing effect on the implants by virtue
of their strong progestin. This discourages further growth of
pre-existing implants.
-
Reduce the levels of circulating estrogens, particularly estradiol.
By inhibiting ovarian function and providing "add-back" estrogen, the
s. estradiol levels in the blood are usually a little lower than
before the BCP was taken. Lower estrogen levels ease some of the
hormonal stimulatioin of the implants.
-
When taken continuously, stop the episodic hormonal withdrawal
bleed that occurs both with normal endometrium and with endometrial
implants.
For severe endometriosis, other more powerful medications or surgery
are often needed to be effective.
It usually takes 3-6 months of continuous OCPs for the patient to
notice a significant benefit and up to 12 months to achieve maximum
benefit.
OCPs are relatively inexpensive, making this treatment choice very
affordable for most patients.
 GnRH Agonists GnRH Agonists
Luprolide induces a temporary and artificial menopause, with inhibition
of ovarian function. The bad part of that are the side-effects,
including hot flashes, night sweats, vaginal dryness and other menopause
symptoms. The good part is that deprived of their estrogen support,
endometriosis implants regress and may disappear.
Many physicians will
provide add-back estrogen to their endometriosis patients who experience
significant menopausal symptoms. This add-back estrogen is a very small
dose and does not apparently reduce the beneficial impact of Luprolide,
but does provide significant relief of their annoying symptoms.
Most patients taking this medication will notice a significant
improvement of their symptoms in 3 months and by 6 months feel very
good. After 6 months, the medication needs to be stopped, although
another course can be taken later, if needed.
Luprolide is moderately expensive, a potentially limiting factor for
some patients.
Danazol
This is a cousin of testosterone and has both direct and indirect
effects on endometriosis. It:
-
Directly inhibits endometriotic implant growth through its
powerful decidualization properties.
-
Suppresses the secretion of pituitary gonadotropins, resulting in
inhibition of ovarian function and lower estrogen levels.
-
Blocks steroidogenic enzymes.
The two main problems with Danazol when used for treatment of
endometriosis are its high cost and significant side-effects (weight
gain, masculinizing side-effects and depression). However, it is very
effective in treating endometriosis and few patients stop it, even if
they experience side-effects. It is normally taken for about a year
before stopping it.
Progestins
Progestins can inhibit pituitary release of gonadotropins, blocking
ovarian function, and have a strong decidualizing effect on endometrial
implants, limiting their growth. Both properties are valuable when
treating endometriosis.
Progestins seem to be about as effective in
treating endometriosis as OCPs, but are somewhat less well tolerated.
Weight gain and breakthrough bleeding are the biggest problems. It is
not particularly expensive, and is a reasonable choice for someone
wishing to avoid surgery and OCPs, but intolerant of Danazol or Luprolide.
Conservative Surgery
Conservative surgery means surgically removing as much endometriosis as
possible, but within the limitations of preserving childbearing capacity
as much as possible. This means leaving the uterus, tubes and ovaries
largely intact, but removing all endometriosis implants that can safely
be removed.
Conservative surgery is the best choice for most
infertility patients as none of the non-surgical treatments has been
found to improve the patient's fertility at all. In contrast,
conservative surgery will achieve 40% to 60% post-surgical pregnancy
rates, depending on the severity of the disease.
Definitive Surgery
Definitive surgery involves a hysterectomy, with or without removal of
the tubes, ovaries, and other sites of endometriosis. Definitive gives
the greatest chance of permanently curing the pain of endometriosis, but
necessarily involves giving up any chance for future childbearing.
Controversial is the role of removal of the ovaries. If you remove them,
you will achieve a slightly higher cure rate than if you leave them
alone. However, you will surgically create menopause and without
treatment, create menopausal symptoms. For this reason, many
gynecologists prefer to leave the ovaries in.
Other gynecologists prefer to remove the ovaries, with the intention
of starting estrogen replacement therapy immediately after surgery. The
addition of these small amounts of estrogen are apparently not enough to
further feed the endometriosis.
The
Military Setting
Patients presenting in an advance military setting will generally complain of
chronic pelvic pain, of at least 6 months duration, that is significantly worse
during their menstrual flow. They may have painful intercourse on deep
penetration and may experience painful bowel movements. Sometimes, the only
symptom is progressively worse dysmenorrhea. Usually, there will be at least
focal tenderness in the adnexal areas, and sometimes generalized tenderness.
These patients will benefit from a course of antibiotic (doxycycline, ciprofloxacin, zithromax, or comparable drugs
capable of clearing chronic PID), and OCPs.
The antibiotic will insure that chronic PID is not a
source of their pain, and the OCPs will be effective at limiting their symptoms and treating the endometrioisis.
Most effective in this setting will be continuous OCPs, to totally
suppress the menstrual cycle. |