|
 The
Menstrual Cycle The
Menstrual Cycle
Among women of childbearing age, there is an expected pattern of the
menstrual cycle. The interplay of hormones, receptor sites, growth
factors, inhibin, and activin with the granulosa and thecal cells in the
ovary is complex. An over-simplified version is:
-
Responding to low levels of
estrogen, the hypothalamus sends a signal to the anterior pituitary gland to
release follicle stimulating hormone (FSH). In addition to stimulating
ovarian follicular growth, FSH also stimulates the granulosa cells of the
follicle to produce gradually increasing amounts of estrogen. This estrogen
has many effects, including stimulation of the endometrium glandular
epithelium to proliferate (reproduce), creating an environment that will
later prove hospitable for implantation of a fertilized ovum.
-
As the estrogen production
accelerates, it begins to inhibit FSH and at the same time stimulates
luteinizing hormone (LH). This leads to a major surge in LH that peaks 12 to
24 hours before ovulation. This surge in LH is accompanied by a parallel
surge in FSH and estrogen.
-
After the peak of LH, FSH and
estradiol, continuing secretion of LH causes the granulosa cells to produce
progesterone. In the absence of pregnancy, the progesterone is produced for
about 10 days. Then it and estrogen production rapidly decline, leading to a
significant withdrawal of hormonal support from the endometrium. This
provokes bleeding as the decidualized endometrium is shed, leaving only the
endometrial basal layer of cells.
-
Responding to the low levels of
estrogen, the hypothalamus again causes release of FSH from the anterior
pituitary, and the cycle begins again.
Normal
Bleeding
-
Occurs approximately once a
month (every 26 to 35 days).
-
Lasts a limited period of
time (3 to 7 days).
-
May be heavy for part of the
period, but usually does not involve passage of clots.
-
Often is preceded by
menstrual cramps, bloating and breast tenderness, although not all
women experience these premenstrual symptoms.
Abnormal Uterine Bleeding
Abnormal bleeding has a number of definitions, the
simplest of which is, "all bleeding that is not normal." Abnormal bleeding
includes:
-
Too frequent periods (more often
than every 26 days).
-
Heavy periods (with passage of
large, egg-sized clots).
-
Any bleeding at the wrong time,
including spotting or pink-tinged vaginal discharge
-
Any bleeding lasting longer than 7
days.
-
Extremely light periods or no
periods at all
Dysfunctional Uterine bleeding
Dysfunctional bleeding is another term with varying
definitions. Some consider bleeding dysfunctional if there is any abnormal
uterine bleeding in the absence of uterine pathology or medical illness. Others
feel that drawing such a fine distinction is pointless as many medical illnesses
(polycystic ovary syndrome, hypothyroidism, hyperthyroidism, adrenal
hyperplasia) can create a pattern of bleeding that is clinically
indistinguishable from the traditional "dysfunctional" uterine bleeding. Many
gynecologists use the term abnormal uterine bleeding (AUB) and dysfunctional
uterine bleeding (DUB) interchangeably.
Overview
Any woman complaining of abnormal vaginal bleeding should be examined.
Occasionally, you will find a laceration of the vagina, a bleeding lesion, or
bleeding from the surface of the cervix due to cervicitis. More commonly, you
will find bleeding from the uterus coming out through the cervical os.
Excluding pregnancy, there are
really only three reasons for abnormal uterine bleeding:
-
Mechanical Problems
-
Hormonal Problems
-
Malignancy
The limited number of
possibilities makes your caring for these patients very simple. If the
bleeding is heavy, obtain a blood count
and assess the rate of blood loss to determine how much margin of safety
you have. Someone with a good blood count (hematocrit)
and minimal rate of blood loss (less than a heavy period), can tolerate
this rate of loss for many days to weeks before the bleeding itself
becomes a threat. Determine whether the bleeding is significant enough
to begin iron replacement therapy.
Pregnancy Problems
A variety of pregnancy problems
can cause vaginal bleeding. These include:
If the bleeding patient has a
positive pregnancy test, a careful search should be made for each of
these problems. However, if the pregnancy test is negative,
pregnancy-related bleeding problems are effectively ruled out.
Read
more about Pregnancy Problems
Read more about Placenta Previa and Placental
Abruption
 Mechanical
Problems Mechanical
Problems
Such problems as uterine
fibroids or polyps are examples of mechanical problems inside the
uterus.
Since mechanical problems have
mechanical solutions, these patients will need surgery of some sort
(Polypectomy, D&C, Hysteroscopy, Hysterectomy, Myomectomy, etc.) to
resolve their problem.
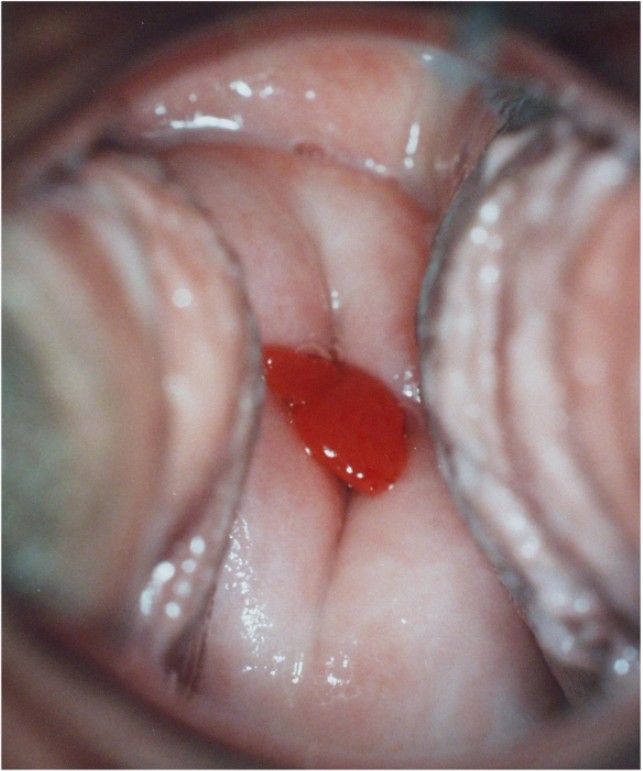
-
Polyps visible protruding from the
cervix are usually coming from the cervix and can be easily twisted off.
-
A simple ultrasound scan can reveal
the presence of fibroids and their location. Those fibroids that are impinging
on the endometrial cavity are the most likely to be responsible for abnormal
bleeding.
-
Endometrial polyps can be identified
with a fluid-enhanced ultrasound (sonohysterography), a simple office
procedure. They can also be identified during hysteroscopy.
-
An endometrial biopsy can be useful
in ruling out malignancy or premalignant changes among women over age 40. It
can also be useful in younger women in identifying the hormonally confused
endometrium of anovulatory bleeding, and will sometimes pick up a small piece
of endometrial polyp.
-
Another form of mechanical problem is
an IUD causing abnormal bleeding. These should always be removed.
Hormonal Problems
Hormonal causes for abnormal bleeding include anovulation leading to an
unstable uterine lining, breakthrough bleeding associated with birth control
pills, and spotting at midcycle associated with ovulation. Some of these cases
will be related to an underlying medical abnormality, such as polycystic ovary
syndrome, hyper or hypothyroidism, adrenal hyperplasia, and pituitary adenoma.
Rarely, this may be due to a hormone secreting neoplasm of the ovary.
The solution to all of these problems
is to find and treat those underlying medical abnormalities that exist, and/or
take control of the patient hormonally and insist (through the use of BCPs) that
she have normal, regular periods.
-
Thyroid disease can be ruled out
clinically or through laboratory testing (TSH)
-
Adrenal hyperplasia can be ruled out
clinically or through laboratory testing (DHEAS, 17 hydroxyprogesterone, ACTH
stimulation test)
-
Prolactin-secreting pituitary adenoma
can be ruled out clinically or through laboratory testing (serum
prolactin)
-
Hormone-secreting ovarian neoplasms
can be ruled out clinically or through laboratory testing (ultrasound,
estradiol, testosterone)
-
Anovulation can be confirmed through
the use of endometrial biopsy, although for women under age 40, biopsy is only
infrequently utilized.
If the abnormal bleeding is
light and the patient's blood count good, starting low-dose BCPs at the
next convenient time will usually result in effective control within a
month or two.
If the bleeding is quite heavy
or her blood low, then it is best to have the patient lie still while
you treat her with birth control pills. Some gynecologists have used 4
BCPs per day initially to stop the bleeding, and then taper down after
several days to three a day, then two a day and then one a day. If you
abruptly drop the dosage, you may provoke a menstrual flow, the very
thing you didn't want.
Alternatively, particularly for
those with intractable anovulatory bleeding, plain estrogen in doses of
2.5 up to 25 mg a day can be effective in promoting endometrial
proliferation, stopping the bleeding. After the bleeding is initially
controlled with estrogen, progesterone is added to stabilize the
endometrium, leading up to a hormonal withdrawal flow a week or two
later. Two drawbacks to this approach are the nausea that frequently
accompanies such large doses of estrogen, and the theoretical risk of
thromboembolism among women exposed to large amounts of estrogen while
on bed rest.
Giving iron supplements is a
good idea (FeSO4 325 mg TID PO or its' equivalent) for anyone who is
bleeding heavily.
Malignancy
Abnormal bleeding can also be a symptom of malignancy, from the vagina,
cervix or uterus.
Cancer of the vagina is
extraordinarily rare and will present with a palpable, visible, bleeding
lesion on the vaginal wall. Cancer of the cervix is more common but a
normal Pap smear and normal exam will effectively rule that out. Should
you find a bleeding lesion in either the vagina or on the cervix, these
should be biopsied.
Factors that increase the risk
for endometrial carcinoma include:
-
Increased estrogen exposure
(exogenous or endogenous)
-
Diabetes
-
Overweight (through increased
conversion of androstenedione to estrone by body fat cells)
-
Chronic, untreated anovulation (many
years)
Cancer of the uterus
(endometrial carcinoma) occurs most often in the older population
(post-menopausal) and is virtually unknown in patients under age 35. For
those women with abnormal bleeding over age 40, an endometrial biopsy is
a wise precaution during the evaluation and treatment of abnormal
bleeding.
Read more about Cancer of the Uterus
Diagnostic and Therapeutic Options
- Pregnancy test
- Examine the patient
- Pap smear
- Biopsy any visible lesions of the
cervix or vagina
- Endometrial biopsy for women over
age 40
- Pelvic ultrasound scan to look for
submucous fibroids
- Sonohysterography if D&C is not
planned and abnormal bleeding persists
- Blood count (if bleeding has been
heavy and prolonged)
- Correct any underlying medical
problems
- Begin OCPs to control abnormal
bleeding due to hormonal causes
- Continuous OCPs to suppress
menstruation completely
- Depo Provera to suppress ovulation
and menstruation
- D&C (with or without hysteroscopy)
to remove endometrial polyps
- If bleeding is intractable and the
patient desires to preserve childbearing, consider myomectomy if submucous
fibroids are contributing to the bleeding.
- If bleeding is intractable and the
patient has completed childbearing, consider balloon or roller-ball ablation
of the endometrium, or hysterectomy.
|
Heavy Periods
Heavy periods ("menorrhagia," "hypermenorrhea") and lengthy periods may reflect
an underlying mechanical abnormality inside the uterus (fibroids, polyps), may
be a cause of iron-deficiency anemia, may contribute to uncomfortable menstrual
cramps. If the examination, Pap smear, and pregnancy test are normal, then the
chance of malignancy is very low and need not be further considered in those
under age 40 unless symptoms persist. Those over 40 should have an endometrial
biopsy.
One good approach is to give
birth control pills to women with these heavy periods. The effect of the
BCPs is to reduce the heaviness and duration of flow. If they are
anemic, oral iron preparations will usually return their iron stores to
normal. If the BCPs (standard, low dose, monophasic pill such as Ortho
Novum 1+35, LoOvral or LoEstrin 1.5/30) fail to reduce the flow
appreciably, they can be taken continuously, without the usual "week
off." This will postpone their menstrual period for as long as several
months. Even though their period may still be heavy or lengthy, the fact
that they only have it every few months rather than every 4 weeks will
have a major impact on their quality of life and anemia, if present.
Alternatively, you could start
the patient on DMPA (depot medroxyprogesterone acetate) 150 mg IM Q 3
months. This will usually disrupt the normal period and she probably
won't continue to have heavy periods. There are some significant
drawbacks to this approach, however. Light spotting or bleeding are
common among women taking DMPA, so you will be substituting one nuisance
for another nuisance.
If sonohysterography
demonstrates an endometrial polyp, removal of the polyp will often
restore a normal menstrual flow. OCPs will sometimes reduce the flow due
to fibroids enough to allow the patient to tolerate these flows for
extended lengths of time.
Light Periods
Extremely light periods, so long as they occur at the right time, are not
dangerous and really are not a medical problem.
This condition is most often
seen among women taking low dose birth control pills. The birth control
pills usually act by blocking the normal ovarian function (production of
various hormones and ovulation), and then substituting the hormones
(estrogen and progestin) found in the BCPs. Usually, the result of this
exchange is that the circulating estrogen levels are about the same as
if the woman were not taking BCPs. In some women, however, the estrogen
levels are significantly lower than before they started taking the BCPs.
In this case, they will notice their menstrual periods getting lighter
and lighter (over 3 to 6 months), and possibly even disappearing
altogether.
This is not dangerous, has no
impact on future fertility, and will resolve spontaneously if the BCPs
are stopped. Stopping the BCPs is not necessary, however, because there
are other safe alternatives. If the periods are simply very light (1-2
days), you can ignore the problem because this situation poses no threat
to the patient.
If periods have totally
stopped:
-
Rule out pregnancy.
-
You may change to a different
BCP with different hormone in it. This will often lead to recognizable
periods because the different hormone is metabolized differently.
-
You may add estrogen
(Premarin .625 mg or Esterase 1 mg) to each BCP to increase the
estrogen stimulation of the uterine lining, increasing its' thickness
and leading to heavier periods. After the desired effect has been
achieved (recognizable periods), the extra estrogen can be stopped.
-
You may safely reassure the
patient and allow her to not have periods while taking the BCPs. As
long as she otherwise feels well, the absence of periods while taking
BCPs is not known to have any adverse effects and some women prefer to
avoid monthly flows.
Late
for a Period
Pregnancy should be ruled out with a pregnancy test.
If the pregnancy test is
negative and the patient is not taking hormonal contraception, then
simple observation for a single missed period is the usually the wisest
course. Delay of periods in operational settings is common. In Boot
Camp, among women not on BCPs, about 1/3 of women will skip periods for
up to three months. The same observation is found among college freshman
women. Presumably, this is a stress response.
If the patient remains without
a period for an extended length of time (3 months or more), then the
following are often done:
-
Normal menstrual flows are
re-established with either BCPs, or Provera (10 mg a day x 5 days,
followed 3 days later by a period). Provera works well if ovarian
function is not deeply depressed, but will not work for some women.
BCPs will usually work regardless of the degree of ovarian
suppression.
-
The patient is tested for
thyroid malfunction. (TSH or Thyroid Stimulating Hormone test).
-
The patient is tested for
prolactin disorders. (prolactinoma, often associated with
inappropriate milk secretion from the nipples)
-
The patient is tested for
premature ovarian failure. (FSH/follicle stimulating hormone and LH/luteinizing
hormone)
If any of these tests are
abnormal or neither Provera nor BCPs are effective in restarting normal
periods, gynecologic consultation upon return to garrison is indicated.
Irregular Periods
This means menstrual periods coming at unpredictable intervals, rather than the
normal once-a-month cycles.
If the flows, whenever they come, are
normal in character and length, this is not a dangerous condition and no
treatment or evaluation is required. If the patient finds the irregular
character of her periods to be troublesome, then starting low dose BCPs will
be very effective in giving her quite normal, once-a-month menstrual flows.
If the flows, whenever they come, are
not consistent; are sometimes heavy, are sometimes light, are sometimes only
spotting, then they are likely not true menstrual cycles, but are anovulatory
bleeding (uterine bleeding occurring in the absence of ovulation). This
condition should be treated with re-establishment of normal, regular periods,
usually with BCPs. Unresolved anovulatory bleeding may, over many months to
years, lead to cosmetic problems (unwanted hair growth due to relative excess
of male hormones) and uterine lining problems (endometrial hyperplasia due to
a lack of the protective hormone progesterone).
Patients with infrequent periods,
particularly if associated with overweight status, acne, and multiple
follicles on the ovary when visualized with ultrasound, usually have
"polycystic ovary syndrome." This condition may be effectively treated with
OCPs, but also responds well to the use of Metformin.
Patients with hypothyroidism may also
have this type of menstrual cycle, and screening for thyroid disease with a
TSH is helpful.
Too Frequent Periods
Periods that are too frequent (more
often than every 26 days, "metrorrhagia") can be related to several
predisposing factors:
-
If the periods are otherwise
normal, then a short "luteal phase" or insufficient ovarian production
of progesterone may be responsible.
-
If the periods are
inconsistent, then failure to ovulate and the resulting anovulatory
bleeding may be responsible.
-
If the periods are actually
normal and once a month, but there are episodes of bleeding in between
the periods, then mechanical factors such as fibroids or polyps may be
responsible.
Women with hyperthyroidism are
classically described as experiencing frequent, heavy periods. They, in
reality, rarely show that pattern, but we usually
screen these patients for thyroid disease anyway.
Constant Bleeding
Women who experience significant daily bleeding for a very long time
(weeks) sometimes develop another kind of problem unique to this
circumstance, denuding of the uterine lining.
Normally, small breaks or tears in
the uterine lining are promptly repaired. For women who have been bleeding for
weeks, with the accompanying uterine cramping, the uterine lining becomes very
nearly completely lost. There is so little endometrium left that the woman
will have difficulty achieving repair and restoration of the normal lining
without external assistance. A common example of this situation would be a
teenager who has been bleeding for many weeks but who, through embarrassment,
has not sought medical attention. On arrival, she continues to bleed small
amounts of bright red blood. She is profoundly anemic, with a hemoglobin of
7.0.
These patients do not respond to
simple BCP treatment because the BCPs are so weak in estrogen and so strong in
progestin that the uterine lining barely has a chance to grow and cover up the
denuded, bleeding areas inside the uterus.
These patients need strong doses of
plain estrogen, to effectively stimulate the remaining uterine lining (causing
it to proliferate). Premarin, 2.5 to 5 mg PO per day, or IV (25 mg slowly over
a few hours) will provide this strong stimulus to the uterine lining and if
combined with bedrest, will usually slow or stop the bleeding significantly
within 24 hours. The estrogen is stimulating the uterine lining to grow lush
and thick. The estrogen is continued for several days, but at lower dosages
(1.25 to 2.5 mg per day) until the bleeding completely stops. Then,
progesterone is added (Provera 5-10 mg PO per day) for 5-10 days. Progesterone
is necessary at this point because the lush, thick uterine lining is also very
fragile and easily broken. Progesterone provides a structural strength to the
uterine lining, making it less likely to tear or break.
Once a normal, thick, well-supported
lining has been re-established, first with estrogen, then with the addition of
progesterone, it will need to be shed, just like a normal lining is shed once
a month. Stopping all medication will trigger a normal menstrual flow about 3
days later. The lining will have been restored and the vicious cycle of
bleeding leading to more endometrial loss leading to more bleeding will be
broken. Future periods may then be normal, although many physicians will start
BCPs at that point to prevent recurrence of the constant bleeding episode.
Hemorrhage
Hemorrhage is defined
differently by different texts, but three good general guidelines are
these:
-
If the bleeding is heavier
than the heaviest menstrual period the patient has ever
experienced...that is hemorrhage.
-
If, when standing, blood is
running down her leg and dripping into her shoes...that is hemorrhage.
-
If, because of heavy vaginal
bleeding, the patient cannot stand upright without feeling
light-headed or dizzy...that is hemorrhage.
Vaginal hemorrhage is more
often associated with pregnancy complications such as miscarriage or
placental abruption, but certainly can occur in the absence of
pregnancy.
This is a true medical
emergency and a number of precautionary steps should be taken:
-
IV access should be
established to facilitate fluid resuscitation
-
Blood transfusion should be
made readily available, if it proves necessary.
-
Pregnancy must be
excluded as it's presence may profoundly effect the treatment.
-
Bedrest will lead most cases
of hemorrhage to slow, regardless of the cause.
-
Medical evacuation should be
planned as the definitive treatment of uterine hemorrhage not
responsive to conservative measures is surgical.
Helpful tips:
-
Blood counts (hgb or hct)
performed during an acute hemorrhage may be falsely reassuring as the
hemoconcentration accompanying hemorrhage may take several hours to
re-equilibrate in response to your IV fluids.
-
Elevation of the legs to
about 45 degrees will add as much as one unit of fresh, whole blood to
the patient's circulation by eliminating pooling in the lower
extremities.
In severe cases of hemorrhage
when surgical intervention is not immediately available, vaginal packing
can slow and sometimes stop bleeding due to vaginal lacerations or uterine
bleeding from many causes.
- After a Foley catheter is inserted in the
bladder, a vaginal speculum holds the vaginal walls apart.
- Tail sponges,
long rolls of gauze, 4 X 4's or any other sterile, gauzelike substance can
be packed into the vagina.
- The upper vagina is packed first, with moderate
pressure being exerted to insure a tight fit.
- Then, progressively more
packing material is stuffed into the lower vagina, distending the walls.
- Ultimately, the equivalent of a 12-inch or 16-inch softball sized mass of
gauze will be packed into the vagina.
This has several effects:
- Any
bleeding from the cervix or vagina will have direct compression applied,
slowing or stopping the bleeding.
- The uterus is elevated out of the
pelvis by the presence of the vaginal pack, placing the uterine vessels on
stretch, slowing blood flow to the uterus and thus slowing or stopping any
intrauterine bleeding.
- By disallowing the egress of blood from the
uterus, intrauterine pressure rises to some extent, exerting a tamponade
effect on any continuing bleeding within the uterus.
Vaginal packing can
be left for 1-3 days, and then carefully removed after the bleeding has
stopped or stabilized. Sometimes, only half the packing is removed,
followed by the other half the following day. The Foley catheter is very
important, both to monitor kidney function and to allow the patient to
urinate (usually impossible without a Foley with the vaginal packing in
place). |