|
 Endometrial cancer is the single most common genital tract malignancy in
women. A woman's lifetime risk of ever developing endometrial cancer is
about 2%. Peak incidence is between age 50 and 65. Endometrial cancer is the single most common genital tract malignancy in
women. A woman's lifetime risk of ever developing endometrial cancer is
about 2%. Peak incidence is between age 50 and 65.
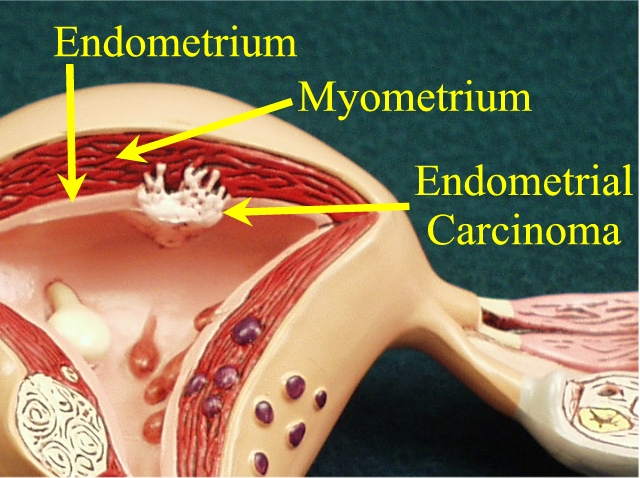
Endometrial cancer arises from the glandular cells of the uterine
lining. The most common form of this occurs among women exposed to
chronic, unopposed estrogen.
- Estrogen stimulates the uterine lining to proliferate, becoming
lush and thick. Normally, estrogen is episodically opposed by
progesterone (produced with ovulation). Progesterone inhibits the
proliferative growth effects of estrogen, and provide structural
support to the soft, otherwise friable endometrium. With the
withdrawal of progesterone at the end of the menstrual cycle, the
structural support to this thickened endometrium is weakened, and
shedding of the uterine lining occurs.
- Without this cyclic progesterone exposure and episodic shedding,
the uterine lining becomes too thick and the endometrial glands too
crowded. This is called endometrial hyperplasia. Should the
hyperplasia go unchecked, some degree of cellular atypia often
develops. Ultimately, the glandular cells look and behave so atypical
that they begin to invade through the basement membrane...cancer of
the endometrium.
Thus, most cases of endometrial cancer arise from endometrial
hyperplasia because of chronic, unopposed estrogen stimulation.
Clinically, this situation might arise in a chronically anovulatory
patient, or an obese patient, whose body fat cells are converting
androstenedione to estrone. Endometrial carcinoma has been associated
with a number of clinical conditions, but the apparent common final
pathway to cancer is chronic, unopposed estrogen.
Not all cases of endometrial cancer arise in this fashion. There is a
subgroup whose cancer does not appear to be estrogen dependent. These
cancers usually arise in older women, tend not to be associated with
endometrial hyperplasia, and tend to be unusually aggressive and less
responsive to usual treatment.
Abnormal bleeding is the classical symptom of endometrial cancer.
Because abnormal bleeding is widely viewed as a danger sign, and because
of the availability with simple endometrial biopsies, many cases of
endometrial cancer never occur. During the hyperplasia stage, abnormal
bleeding develops which is evaluated by sampling of the endometrium. The
hyperplasia is treated with progestins, and a subsequent cancer avoided.
Thus, a common approach to a woman at risk for endometrial cancer
(post-menopausal, for example), is to sample the endometrium whenever
abnormal bleeding is encountered. There may be exceptions to this
general approach, but sampling may involve endometrial biopsy, D&C,
and/or hysteroscopy. Recent advances in ultrasound technology have led
to increased use of this technique, particularly when combined with
intracavitary infusion of saline to outline the endometrial structures
more clearly.
|
In those cases in which the cancer is not avoided, treatment varies,
depending on the extent of the cancer. One factor influencing choice of
treatment is the staging of the disease:
|
Stage |
Extent of Disease |
|
I |
Cancer limited to the uterine
body (corpus) |
|
II |
Cancer extends into the cervix,
but not beyond the uterus. |
|
III |
Cancer extends beyond the
uterus, but only so far as the peritoneum, adnexa or vagina |
|
IV |
Cancer extends into the bladder,
bowel, or to distant sites |
Within each stage are subgroups (eg, Stage IA, IB, IC) that distinguish
the extent of disease within each stage.
Other factors influencing the choice of treatment include tumor grade,
histologic subtype, age, race, depth of endometrial penetration through
the uterine wall, and presence or absence of positive peritoneal
cytology and distant metastases. Among the choices for treatment are
simple TAH/BSO, pelvic/periaortic lymphadenectomy, radiation therapy and
chemotherapy. Prognosis for the lower stage, better differentiated
tumors is excellent. For more advanced cancers, the prognosis is not as
good.
Typical management of these patients consists of:
-
Identifying the patient with endometrial cancer.
-
Staging the cancer to enable selection of the best therapy.
-
TAH/BSO for Stage I and possibly some Stage II patients
-
Whole pelvis irradiation for more advanced cases, either as an
adjunct to surgery or instead of surgery.
-
Additional irradiation to periaortic areas if metastases are
present
-
Possible chemotherapy for very advanced cancers.
-
Surveillance for recurrence.
|