|
Vaginal Discharge
Overview · History
· Physical
· Laboratory
· Treatment
· Cervical Ectropion
· Cervicitis
· Chlamydia
· Foreign Body
· Gardnerella
· Gonorrhea
· Infected IUD
· PID: Mild
· PID: Moderate to Severe
· Trichomonas
· Yeast
Overview
The diagnosis of vaginal discharge is based on a History, Physical Exam, and a
few simple diagnostic tests.
History
Ask the patient about itching, odor, color of discharge, painful intercourse, or
spotting after intercourse.
-
Yeast causes intense itching with a cheesy, dry discharge.
-
Gardnerella causes a foul-smelling, thin white discharge.
-
Trichomonas gives irritation and frothy white discharge.
-
Foreign body (lost tampon) causes a foul-smelling black discharge.
-
Cervicitis causes a nondescript discharge with deep dyspareunia
-
Chlamydia may cause a purulent vaginal discharge, post-coital spotting, and deep
dyspareunia.
-
Gonorrhea may cause a purulent vaginal discharge and deep dyspareunia.
-
Cervical ectropion causes a mucous, asymptomatic discharge.
Physical Exam
Inspect carefully for the presence of lesions, foreign bodies and odor. Palpate to
determine cervical tenderness.

-
Yeast has a thick white cottage-cheese discharge and red vulva.
-
Gardnerella has a foul-smelling, thin discharge.
-
Trichomonas has a profuse, bubbly, frothy white discharge.
-
Foreign body is obvious and has a terrible odor.
-
Cervicitis has a mucopurulent cervical discharge and the cervix is tender to touch.
-
Chlamydia causes a friable cervix but often has no other findings.
-
Gonorrhea causes a mucopurulent cervical discharge and the cervix may be tender to
touch.
-
Cervical ectropion looks like a non-tender, fiery-red, friable button of tissue
surrounding the cervical os.
-
Infected/Rejected IUD demonstrates a mucopurulent cervical discharge in the presence of
an IUD. The uterus is mildly tender.
-
Chancroid appears as an ulcer with irregular margins, dirty-gray necrotic base and
tenderness.
Laboratory
Obtain cultures for chlamydia, gonorrhea, and Strept. You may test the vaginal
discharge in any of 4 different ways:
-
Test the pH. If >5.0, this suggests Gardnerella.
-
Mix one drop of KOH with some of the discharge on a microscope slide. The release of a
bad-smelling odor confirms Gardnerella.
-
Examine the KOH preparation under the microscope ("Wet
Mount"). Multiple strands of thread-like hyphae confirm the presence of yeast.
-
Mix one drop of saline with some discharge ("Wet
Mount").
Under the microscope, large (bigger than WBCs), moving micro-organisms with four flagella
are trichomonads. Vaginal epithelial cells studded with coccoid bacteria are "clue
cells" signifying Gardnerella.
Read more about how to perform a wet mount.
Treatment
In addition to specific treatment of any organism identified by culture or other
test...
-
Any patient complaining of an itchy vaginal discharge should probably be treated with an
antifungal agent (Monistat, Lotrimin, etc.) because of the high likelihood that yeast is
present, and
-
Any patient complaining of a bad-smelling vaginal discharge should probably be treated
with Flagyl (or other reasonable substitute) because of the high likelihood that
Gardnerella is present.
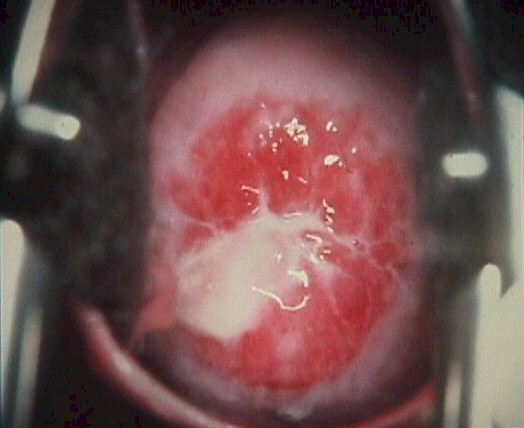
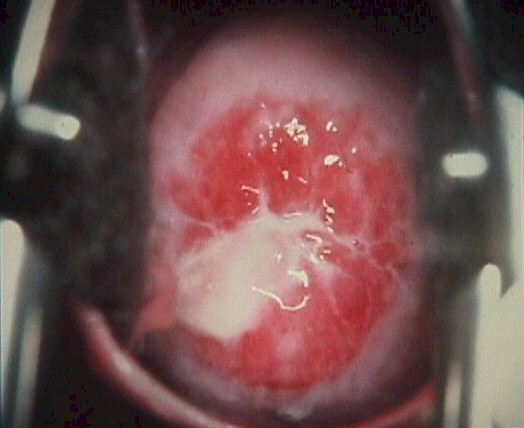
 Ectropion, Erosion or Eversion Ectropion, Erosion or Eversion
This harmless condition is frequently mistaken for cervicitis.
Ectropion, erosion or eversion (all synonyms) occurs when the normal squamo-columnar
junction is extended outward from the its; normal position at the opening of the cervix.
Grossly, the cervix has a red, friable ring of tissue around the os. Careful inspection
with magnification (6-10x) will reveal that this red tissue is the normal tissue of the
cervical canal, which has grown out onto the surface of the cervix.
Cervical ectropion is very common, particularly in younger women and those taking BCPs.
It usually causes no symptoms and need not be treated. If it is symptomatic, producing a
more or less constant, annoying, mucous discharge, cervical cauterization will usually
eliminate the problem.
When faced with a fiery red button of tissue surrounding the cervical os, chlamydia
culture (in high-risk populations) and Pap smear should be performed. If these are
negative and the patient has no symptoms, this cervical ectropion should be ignored.
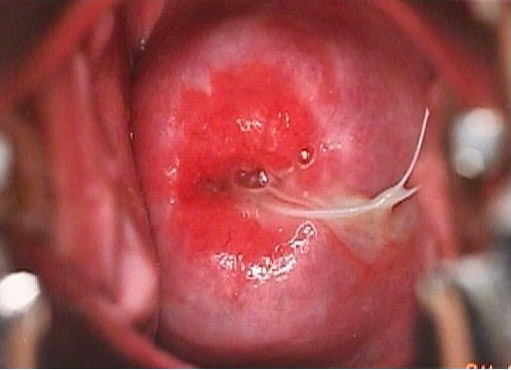
Cervicitis
Inflammation or irritation of the cervix is rarely the cause of significant morbidity.
It is mainly a nuisance to the patient and a possible symptom of underlying disease
(gonorrhea, chlamydia).
Some patients with cervicitis note a purulent vaginal discharge, deep dyspareunia, and
spotting after intercourse, while others may be symptom-free. The cervix is red, slightly
tender, bleeds easily, and a mucopurulent cervical discharge from the os is usually seen.
A Pap smear rules out malignancy. Chlamydia culture and gonorrhea culture (for gram
negative diplococci) are routinely performed.
No treatment is necessary if the patient is asymptomatic, the Pap smear is normal, and
cultures are negative. Antibiotics specific to the organism are temporarily effective and
may be curative. Cervical cautery may be needed to achieve permanent cure.
|
Mucupurulent Cervicitis due to
Chlamydia Infection |
Chlamydia
This sexually-transmitted disease is caused by "Chlamydia trachomatis". It
very commonly locates in the cervical canal although it can spread to the fallopian tubes
where it can cause PID.
Most women harboring chlamydia will have no symptoms, but others complain of purulent
vaginal discharge, deep dyspareunia, and pelvic pain. There may be no significant pelvic
findings, but a friable cervix, mucopurulent cervical discharge, pain on motion of the
cervix, and tenderness in the adnexa are suggestive.
The diagnosis is often made on the basis of clinical suspicion but can be confirmed
with chlamydia culture. Such cultures are frequently performed routinely in high-risk
populations.
Treatment is:
Recommended Regimens
Azithromycin1 g orally in a single dose
OR
Doxycycline100 mg orally twice a day for 7 days.
Alternative Regimens
Erythromycin base500 mg orally four times a day for 7 days,
OR
Erythromycin ethylsuccinate800 mg orally four times a day for 7 days,
OR
Ofloxacin300 mg orally twice a day for 7 days,
OR
Levofloxacin500 mg orally for 7 days.
Read the CDC Treatment Guidelines for
Chlamydia
Foreign Body
Lost and forgotten tampons are the most common foreign body found in the vagina,
although other objects are occasionally found. Women with this problem complain of a
bad-smelling vaginal discharge which is brown or black in color. The foreign body can be
felt on digital exam or visualized with a speculum.
As soon as you suspect or identify a lost tampon or other object in the vagina,
immediately prepare a plastic bag to receive the object. As soon as it is retrieved, place
it in the bag and seal the bag since the anaerobic odor from the object will be extremely
penetrating and long-lasting.
Have the patient return in a few days for follow-up examination. Normally, no other
treatment is necessary, but patients who also complain of fever or demonstrate systemic
signs/symptoms of illness should be evaluated for possible toxic shock syndrome, an
extremely rare, but serious, complication of a retained tampon.
Gardnerella (Hemophilus, Bacterial Vaginosis)
The patient with this problem complains of a bad-smelling discharge which gets worse
after sex. Cultures will show the presence of "Gardnerella Vaginalis," the
bacteria associated with this condition. While this problem is commonly called
"Gardnerella," it is probably the associated anaerobic bacteria which actually
cause the bad odor and discharge.
The diagnosis is confirmed by the release of a bad odor when the discharge is mixed
with KOH ("whiff test"), a vaginal pH greater than 5.0, or the presence of
"clue cells" (vaginal epithelial cells studded with bacteria) in the vaginal
secretions.
Treatment is:
Recommended Regimens (CDC 2002)
Metronidazole500 mg orally twice a day for 7 days,
OR
Metronidazole gel0.75%, one full applicator (5 g) intravaginally, once a
day for 5 days,
OR
Clindamycin cream 2%, one full applicator (5 g) intravaginally at bedtime
for 7 days.
Alternative Regimens (CDC 2002)
Metronidazole2 g orally in a single dose,
OR
Clindamycin300 mg orally twice a day for 7 days,
OR
Clindamycin Ovules100 g intravaginally once at bedtime for 3 days.
Read the CDC
Treatment Guidelines for Bacterial Vaginosis
Watch a video showing Clue cells
Gonorrhea
This sexually-transmitted disease is caused by a gram negative diplococcus. The
organism grows easily in the cervical canal, where it can spread to the fallopian tubes,
causing PID. It may also infect the urethra, rectum or pharynx.
Many (perhaps most) women harboring the gonococcus will have no symptoms, but others
complain of purulent vaginal discharge, pelvic pain, and deep dyspareunia. There may be no
significant pelvic findings, but mucopurulent cervical discharge, pain on motion of the
cervix, and tenderness in the adnexa are all classical.
The diagnosis is often made on the basis of clinical suspicion but can be confirmed
with chocolate agar culture or gram stain.
Treatment is:
Recommended Regimens (CDC 2002)
Cefixime400 mg orally in a single dose,
OR
Ceftriaxone125 mg IM in a single dose,
OR
Ciprofloxacin500 mg orally in a single dose,§§
OR
Ofloxacin400 mg orally in a single dose,§§
OR
Levofloxacin250 mg orally in a single dose,§§
PLUS,
IF CHLAMYDIAL INFECTION IS NOT RULED OUT
Azithromycin1 g orally in a single dose
OR
Doxycycline100 mg orally twice a day for 7 days.
Alternative Regimens (CDC 2002)
Spectinomycin 2 g in a single, IM dose. Spectinomycin is expensive
and must be injected; however, it has been effective in published clinical
trials, curing 98.2% of uncomplicated urogenital and anorectal gonococcal
infections. Spectinomycin is useful for treatment of patients who cannot
tolerate cephalosporins and quinolones.
Single-dose cephalosporin regimens (other than ceftriaxone 125 mg IM
and cefixime 400 mg orally) that are safe and highly effective against
uncomplicated urogenital and anorectal gonococcal infections include ceftizoxime (500 mg, administered IM), cefoxitin (2 g, administered IM with probenecid 1 g orally), and cefotaxime (500 mg, administered IM). None of the
injectable cephalosporins offer any advantage over ceftriaxone.
Single-dose quinolone regimens include gatifloxacin 400 mg orally,
norfloxacin 800 mg orally, and lomefloxacin 400 mg orally. These regimens
appear to be safe and effective for the treatment of uncomplicated gonorrhea,
but data regarding their use are limited. None of the regimens appear to offer
any advantage over ciprofloxacin at a dose of 500 mg, ofloxacin at 400 mg, or levofloxacin at 250 mg.
Sexual partners also need to be treated.
Read the CDC Treatment Guidelines for
Gonorrhea
 Infected IUD Infected IUD
Sooner or later, as many as 5% of all intrauterine devices will become infected.
Patients with this problem usually notice mild lower abdominal pain, sometimes have a
vaginal discharge and fever, and may notice deep dyspareunia. The uterus is tender to
touch and one or both adnexa may also be tender.
Treatment consists of removal of the IUD and broad-spectrum antibiotics. If the
symptoms are mild and the fever low-grade, oral antibiotics (amoxicillin, cephalosporins, tetracycline, etc.) are very suitable. If the patient's fever is high, the symptoms
significant or she appears quite ill, IV antibiotics are a better choice (cefoxitin, or metronidazole plus gentamicin, or clindamycin plus gentamicin).
If an IUD is present and the patient is complaining of any type of pelvic symptom, it
is wisest to remove the IUD, give antibiotics, and then worry about other possible causes
for the patient's symptoms.
IUDs can also be rejected without infection. Such patients
complain of pelvic pain and possibly bleeding. On pelvic exam, the IUD is seen protruding
from the cervix. It should be grasped with an instrument and gently removed. It cannot be
saved and should not be pushed back inside.
Read more about IUDs
PID: Mild
Gradual onset of mild bilateral pelvic pain with purulent vaginal
discharge is the typical complaint. Fever <100.4 and deep dyspareunia are common.
Moderate pain on motion of the cervix and uterus with purulent or
mucopurulent cervical discharge is found on examination. Gram-negative diplococci or
positive chlamydia culture may or may not be present. WBC may be minimally elevated or
normal.
Treatment consists of:
Regimen A (CDC
2002)
Ofloxacin400 mg orally twice a day for 14 days
OR
Levofloxacin500 mg orally once daily for 14 days
WITH or WITHOUT
Metronidazole500 mg orally twice a day for 14 days.
Regimen B (CDC 2002)
Ceftriaxone250 mg IM in a single dose
OR
Cefoxitin2 g IM in a single dose and Probenecid, 1 g orally administered concurrently in a single dose
OR
Other parenteral third-generation cephalosporin(e.g., ceftizoximeor cefotaxime)
PLUS
Doxycycline100 mg orally twice a day for 14 days
WITH or WITHOUT
Metronidazole500 mg orally twice a day for 14 days.
For further information, read the CDC Treatment Guidelines for PID
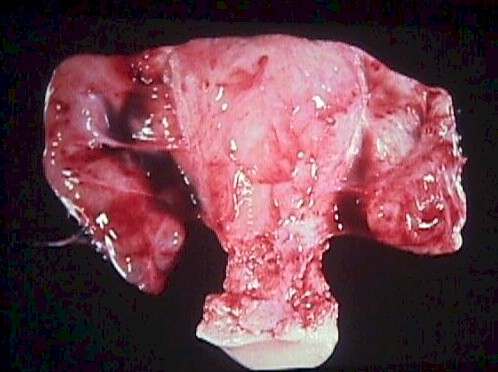
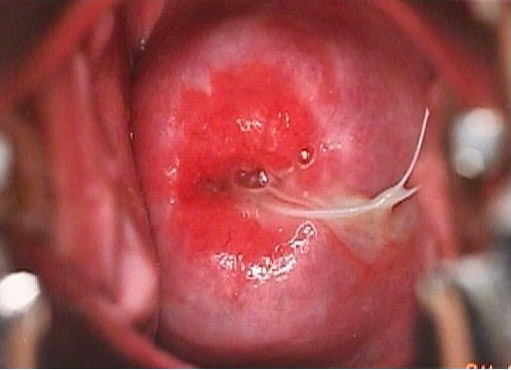
|
Severe PID, required a
hysterectomy to cure. |
PID: Moderate to Severe
With moderate to severe PID, there is a gradual onset of moderate to
severe bilateral pelvic pain with purulent vaginal discharge, fever >100.4 (38.0),
lassitude, and headache. Symptoms more often occur shortly after the onset or completion
of menses.
Excruciating pain on movement of the cervix and uterus is characteristic
of this condition. Hypoactive bowel sounds, purulent cervical discharge, and abdominal
dissension are often present. Pelvic and abdominal tenderness is always bilateral except
in the presence of an IUD.
Gram-negative diplococci in cervical discharge or positive chlamydia
culture may or may not be present. WBC and ESR are elevated.
Treatment consists of bedrest, IV fluids, IV antibiotics, and NG suction
if ileus is present. Since surgery may be required, transfer to a definitive surgical
facility should be considered.
Parenteral Regimen A (CDC 2002)
Cefotetan2 g IV every 12 hours
OR
Cefoxitin2 g IV every 6 hours
PLUS
Doxycycline100 mg orally or IV every 12 hours.
Parenteral Regimen B (CDC 2002)
Clindamycin900 mg IV every 8 hours
PLUS
Gentamicinloading dose IV or IM (2 mg/kg of body
weight) followed by a maintenance dose (1.5 mg/kg) every 8 hours.
Single daily dosing may be substituted.
Alternative Parenteral Regimens (CDC 2002)
Ofloxacin400 mg IV every 12 hours
OR
Levofloxacin500 mg IV once daily
WITH or WITHOUT
Metronidazole500 mg IV every 8 hours
OR
Ampicillin/Sulbactam3 g IV every 6 hours
PLUS
Doxycycline100 mg orally or IV every 12 hours.
For further information, read the CDC Treatment Guidelines for PID
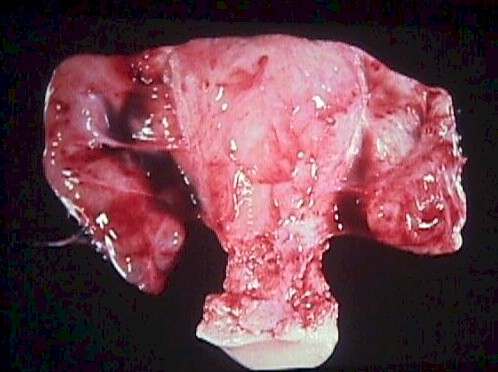
|

Trichomonas vaginal infection |
Trichomonas
This microorganism, with its four flagella to propel it, is not a normal inhabitant of
the vagina. When present, it causes a profuse, frothy white or greenish vaginal discharge.
When the discharge is suspended in normal saline and examined under the microscope, the
typical movement of these large organisms (larger than white blood cells) is obvious.
Itching may be present, but this is inconsistent. Trichomonas is transmitted sexually and
you may wish to treat the sexual partner, particularly if this is a recurrent trichomonad
infection.
Recommended Regimen (CDC 2002)
Metronidazole2 g orally in a single dose.
Alternative Regimen (CDC 2002)
Metronidazole500 mg twice a day for 7 days.
Read the CDC
Treatment Guidelines for Trichomonas
Watch a video showing
trichomonads under the microscope
|

Thick white, cottage cheese discharge
often accompanies yeast infections.
|
Yeast (Monilia, Thrush)
Vaginal yeast infections are common, monilial overgrowths in the vagina and vulvar
areas, characterized by itching,dryness, and a thick, cottage-cheese appearing vaginal
discharge. The vulva may be reddened and irritated to the point of tenderness.
Yeast thrives in damp, hot environments and women in such
circumstances are predisposed toward these infections. Women who take broad-spectrum
antibiotics are also predisposed towards these infections because of loss of the normal
vaginal bacterial flora.
Yeast organisms are normally present in most vaginas, but in small numbers. A yeast
infection, then, is not merely the presence of yeast, but the concentration of yeast in
such large numbers as to cause the typical symptoms of itching, burning and discharge.
Likewise, a "cure" doesn't mean eradication of all yeast organisms from the
vagina. Even if eradicated, they would soon be back because that is where they normally
live. A cure means that the concentration of yeast has been restored to normal and
symptoms have resolved.
The diagnosis is often made by history alone, and enhanced by the classical appearance
of a dry, cheesy vaginal discharge. It can be confirmed by microscopic visualization of
clusters of thread-like, branching Monilia organisms when the discharge is mixed with KOH.
Recommended Regimens (CDC 2002)
Intravaginal Agents:
Butoconazole2% cream 5 g intravaginally for 3 days,
OR
Butoconazole2% cream 5 g (Butaconazole1-sustained release), single
intravaginal application,
OR
Clotrimazole1% cream 5 g intravaginally for 7--14 days,
OR
Clotrimazole100 mg vaginal tablet for 7 days,
OR
Clotrimazole 100 mg vaginal tablet, two tablets for 3 days,
OR
Clotrimazole 500 mg vaginal tablet, one tablet in a single application,
OR
Miconazole2% cream 5 g intravaginally for 7 days,
OR
Miconazole100 mg vaginal suppository, one suppository for 7 days,
OR
Miconazole200 mg vaginal suppository, one suppository for 3 days,
OR
Nystatin100,000-unit vaginal tablet, one tablet for 14 days,
OR
Tioconazole6.5% ointment 5 g intravaginally in a single application,
OR
Terconazole0.4% cream 5 g intravaginally for 7 days,
OR
Terconazole0.8% cream 5 g intravaginally for 3 days,
OR
Terconazole80 mg vaginal suppository, one suppository for 3 days.
Oral Agent:
Fluconazole150 mg oral tablet, one tablet in single dose.
Reoccurrences are common and can be treated the same as for initial infections. For
chronic recurrences, many patients find the use of a single applicator of Monistat 7 at
the onset of itching will abort the attack completely. Sexual partners need not be treated
unless they are symptomatic.
Read the CDC Treatment Guidelines for
Yeast
Watch a video of yeast under the
microscope
|