Duration 9:32
My name is Dr. Jan Eperjesi.
00:02
I’m a resident in obstetrics
00:03
and gynecology
00:04
at Duke University.
00:06
This presentation
00:07
is about nutrition in pregnancy.
00:09
00:12
For this presentation
00:13
on nutrition and pregnancy,
00:15
there are four learning
00:16
objectives.
00:17
Number one is to learn
00:19
the recommendations for weight
00:20
gain in pregnancy.
00:22
Number two is to appreciate
00:23
maternal and fetal risks
00:25
associated
00:25
with excessive or inadequate
00:27
weight gain in pregnancy.
00:29
Number three is to appreciate
00:30
typical weight loss
00:31
after pregnancy.
00:33
Number four is to provide
00:35
information
00:35
about caloric intake, protein
00:37
sources, mercury toxicity
00:39
from certain fish,
00:41
iron requirements, folic acid,
00:44
vitamin A, calcium, caffeine,
00:47
and pica.
00:47
00:50
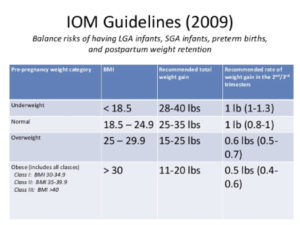
This chart shows the recommended
00:52
weight gain in pregnancy
00:53
for different body mass indexes.
00:56
In 1990, the Institute
00:58
of Medicine recommended a weight
00:59
gain of 25 to 35 pounds or 11.5
01:03
to 16 kilograms
01:04
for women
01:05
with a normal pre-pregnancy body
01:06
mass index.
01:09
The range for twin pregnancy
01:11
is 35 to 45 pounds or 16 to 20
01:14
kilograms.
01:15
Young adolescents that have had
01:17
less than two periods
01:18
after their first menses
01:20
should strive for gains
01:21
at the upper end of this range.
01:23
Shorter women, meaning women
01:25
less than 62 inches
01:27
or 157 centimeters in height,
01:29
should strive for gains
01:31
at the lower end of this range.
01:33
For a body mass index less
01:34
than 19.8, a greater overall
01:37
weight gain is recommended.
01:39
For higher BMIs, the recommended
01:41
weight gain is between 15 to 25
01:43
pounds or seven to 11.5
01:45
kilograms.
01:46
01:50
The current recommendations
01:51
for adequate weight gain
01:52
are from the Institute
01:53
of Medicine in 1990.
01:55
The rationale
01:56
for these recommendations
01:57
aims to prevent pre-term birth
01:59
and fetal growth restriction,
02:01
which are associated
02:02
with inadequate weight gain.
02:04
Interestingly, however,
02:06
the current focus
02:07
is on the obesity epidemic.
02:09
Obesity is associated
02:10
with significantly
02:11
increased risk
02:12
for gestational hypertension,
02:14
preeclampsia,
02:15
gestational diabetes,
02:17
macrosommia, and cesarean
02:18
delivery.
02:20
Studies have shown
02:21
that in obese pregnant women,
02:23
those who gained less than 15
02:24
pounds
02:25
had the lowest rates
02:26
of pre-eclampsia,
02:27
large for gestational age
02:29
infants, and cesarean delivery.
02:31
Other studies have shown
02:33
that women
02:33
with normal pre-pregnancy body
02:35
mass indexes
02:36
who gain less than 25 pounds
02:38
during pregnancy, also
02:40
had a lower risk
02:40
for pre-eclampsia,
02:42
failed induction,
02:43
cephalopelvic disproportion,
02:45
cesarean delivery, and large
02:47
for gestational age infants.
02:48
02:52
Most, but not all, of the weight
02:53
gain during pregnancy
02:55
is lost during and immediately
02:57
after delivery.
02:59
In women whose average weight
03:01
gain is 29 pounds
03:02
during pregnancy, approximately
03:04
12 pounds is lost at delivery.
03:07
In the next two weeks
03:07
after delivery, there
03:09
is an additional nine pounds
03:10
of weight loss.
03:11
A further six pounds is then
03:13
lost between two weeks and six
03:14
months postpartum.
03:16
Overall, the more weight gain
03:18
during pregnancy, the more that
03:20
is lost post-partum.
03:22
Interestingly, however, there
03:23
is no relationship
03:24
between pre-pregnancy body mass
03:26
index or prenatal weight gain
03:29
and weight retention.
03:30
03:33
To the basic protein needs
03:35
of the non-pregnant woman
03:36
are the added demands for growth
03:38
and remodeling of the fetus,
03:40
placenta, uterus, and breasts,
03:42
as well as increased blood
03:43
volume.
03:44
During the second half
03:45
of pregnancy,
03:46
approximately 1,000 grams
03:48
of protein are deposited
03:49
amounting to five to sic grams
03:51
per day.
03:53
The concentrations of most
03:54
amino acids in maternal plasma
03:56
fall markedly.
03:58
Preferably, most protein should
03:59
be supplied from animal sources
04:01
such as meat, milk, eggs,
04:03
cheese, poultry, and fish
04:05
because they provide amino acids
04:06
in optimal combinations.
04:09
Milk and dairy products have
04:10
long been considered nearly
04:11
ideal sources of nutrients,
04:13
especially protein and calcium,
04:15
for pregnant or lactating women.
04:18
Fish are an excellent source
04:19
of protein,
04:20
are low in saturated fats,
04:22
and contain omega 3 fatty acids.
04:25
Because nearly all fish
04:26
and shellfish contain trace
04:28
amounts of mercury,
04:29
pregnant and lactating women
04:31
are advised to avoid
04:32
specific types of fish
04:33
with potentially high
04:34
methyl mercury levels.
04:36
These include shark, swordfish,
04:38
King mackerel, and tile fish.
04:41
It is further recommended
04:43
that pregnant women ingest
04:44
no more than 12 ounces or two
04:46
servings of canned tuna
04:48
per week.
04:49
And no more than six ounces
04:50
of albacore or white tuna.
04:53
If the mercury content
04:55
of locally caught fish
04:56
is unknown, then overall fish
04:58
consumption should be limited
04:59
to six ounces per week.
05:01
05:04
With respect to folic acid,
05:06
greater than 50%
05:07
of all neural-tube defects
05:08
can be prevented
05:09
with daily intake of 400
05:11
micrograms of folic acid
05:13
throughout the pre-conceptual
05:14
period.
05:15
The Center for Disease Control
05:17
in 2004
05:19
estimated that the number
05:20
of pregnancies effected
05:21
by neural tube defects
05:22
has decreased from 4,000
05:24
pregnancies per year
05:25
to approximately 3,000 per year
05:27
since mandatory fortification
05:29
of cereal products
05:30
with folic acid in 1998.
05:33
By adding 140 micrograms
05:35
to folic acid
05:37
to each 100 grams of grain
05:38
products, the intake
05:40
of folic acid by women
05:42
of childbearing age
05:43
may be increased by 100
05:45
micrograms per day.
05:47
However,
05:48
because nutritional sources
05:49
alone are insufficient,
05:50
folic acid supplementation
05:52
is still recommended.
05:54
For those women
05:55
with a prior child
05:56
with a neural-tube effect,
05:58
the recurrence risk, which
05:59
is approximately 2% to 5%,
06:01
can be reduced by more than 70%
06:03
with daily folic acid
06:05
supplements of four milligrams
06:06
per day
06:07
in the month before conception
06:09
and during the first trimester.
06:11
Note the difference between 400
06:13
micrograms for women
06:15
with no prior history
06:16
of a neural-tube defect
06:17
versus four milligrams
06:18
if there is a history
06:19
of a neural-tube defects.
06:21
06:24
With the exception of iron,
06:25
practically all diets that
06:27
supply sufficient calories
06:28
for appropriate weight gain
06:30
will contain enough materials
06:32
to prevent deficiency
06:33
if iodized foods are ingested.
06:36
300 milligrams of iron
06:38
is transferred to the fetus
06:39
and placenta.
06:40
500 milligrams is incorporated
06:42
into the expanding
06:43
maternal hemoglobin mass.
06:45
Nearly all is used
06:46
after mid-pregnancy.
06:49
The pregnant woman may benefit
06:50
from 60 to 100 milligrams
06:51
of iron per day
06:52
if she is large, has
06:54
twin fetuses,
06:55
begins supplementation late
06:56
in pregnancy,
06:58
takes iron irregularly,
06:59
or has depressed hemoglobin
07:01
levels.
07:02
With respect to calcium,
07:03
most maternal calcium is in bone
07:06
and can be readily mobilized
07:07
for fetal growth.
07:09
There is also increased calcium
07:10
absorption by the intestine
07:13
and progressive retention
07:14
throughout pregnancy.
07:14
07:18
Vitamin A is associated
07:19
with birth defects
07:20
at very high doses in the range
07:22
of 10,000 to 50,000
07:23
international units daily.
07:26
There is no vitamin A toxicity,
07:28
however, with a beta carotene
07:29
precursor of vitamin A that
07:31
is found in fruits
07:32
and vegetables.
07:34
The American College
07:34
of Obstetricians
07:35
and Gynecologists
07:36
does not recommend
07:37
supplementation of vitamin A
07:38
because intake in the United
07:40
States is adequate.
07:42
However, in developing
07:43
countries, vitamin A deficiency
07:45
is an endemic nutrition problem.
07:48
It causes night blindness
07:49
in pregnant women
07:50
and is associated with increased
07:51
risk of anemia and pre-term
07:53
birth.
07:54
It is estimated six 6 million
07:56
pregnant women suffer from night
07:57
blindness, secondary to vitamin
07:59
A deficiency.
07:59
08:03
The American Dietetic
08:04
Association recommends
08:05
that caffeine intake
08:06
in pregnancy
08:07
be limited to less than 300
08:08
milligrams per day
08:10
or about three five ounce cups
08:12
of coffee.
08:13
However, only extremely high
08:15
levels of caffeine
08:16
equivalent to greater than five
08:18
cups of coffee per day,
08:20
may have possible association
08:21
with spontaneous abortion.
08:24
Adverse outcomes related
08:25
to caffeine are controversial.
08:27
These include possible low birth
08:29
weight, fetal growth
08:30
restriction,
08:31
and pre-term delivery.
08:33
One study showed that if greater
08:35
than 200 milligrams of caffeine
08:37
throughout pregnancy
08:38
was consumed,
08:39
there was an increased odds
08:40
ratio of 1.4 for fetal growth
08:43
restriction.
08:43
08:47
Pica is defined as craving
08:49
of pregnant women
08:50
for strange foods,
08:51
such as starch and sourdough
08:54
or non-food items,
08:55
for example, ice, starch,
08:57
or clay.
08:58
There is a 4% prevalence of pica
09:00
in the second trimester.
09:03
Pica may be triggered
09:04
by severe iron deficiency,
09:06
but the corollary statement
09:07
is not necessarily true.
09:10
All women with pica
09:11
are not necessarily iron
09:12
deficient.
09:14
Interestingly, pre-term delivery
09:16
at less than 35 weeks
09:18
is twice as high in women
09:19
with pica.
Duration 18:47
00:07
hello everyone this is Chris miranski
00:09
and this video will cover screening
00:11
during pregnancy I’d like to thank dr.
00:13
Deborah Feldman for her contributions to
00:15
this video the goals of this video are
00:18
as follows we will review some of the
00:21
foundational principles related to
00:22
screening tests we will then discuss the
00:25
more common end employees in neural tube
00:27
defects that can be identified through
00:28
early pregnancy screening we will
00:31
introduce serum and ultrasound screening
00:33
through the use of alpha-fetoprotein to
00:35
detect open neural tube defects we will
00:38
understand the strengths and limitations
00:39
of first and second trimester serum and
00:41
ultrasound screening then finally we
00:43
will describe cell-free DNA and its role
00:45
in pregnancy screening so first a review
00:48
of the important concepts around
00:50
screening tests screening tests are not
00:52
designed to be diagnostic people is
00:54
suspicious or positive findings must be
00:57
referred for a diagnosis and treatment
00:59
diagnostic tests tend to be more complex
01:01
time-consuming and costly and diagnostic
01:05
tests should be reserved when signs
01:07
symptoms or positive screening tests
01:09
warrant further investigation a good
01:13
screening test has high sensitivity a
01:15
low false positive rate detection is
01:17
best if it can be in the pre-symptomatic
01:20
period screening tests should have an
01:23
intervention that improves with earlier
01:25
detection and there needs to be cost
01:27
effective important terms to understand
01:30
when it comes to describing and talking
01:32
about screening tests include
01:33
sensitivity specificity positive and
01:36
negative predictive value and the false
01:37
positive rate and I’m going to go over
01:39
those individually sensitivity is the
01:42
probability that a person with a disease
01:44
will be correctly identified by a
01:45
screening test as having the disease
01:47
this is also known as the detection ring
01:50
specificity is the probability that a
01:52
person without a disease will be
01:54
correctly identified by a screening test
01:55
as not having the disease the positive
01:59
predictive value is the probability that
02:00
a person with a positive screening test
02:02
actually has the disease and the
02:04
negative predictive value is the
02:06
probability that a person with a
02:07
negative screening test does not have
02:09
disease
02:09
finally the false positive rate is the
02:12
number of people in the population with
02:14
a pause
02:14
test who do not have the disease and
02:16
when the incidence of disease in
02:18
question is small the false positive
02:21
rate approaches the screen positive rate
02:23
so talking about screening tests they
02:27
are best when there is a large
02:29
difference in normal versus abnormal
02:31
values and this would give a high
02:33
detection rate with the low false
02:34
positive rate it’s also important to
02:37
talk about where you put your cutoff for
02:38
screening tests for example here in the
02:41
unaffected population they seem to
02:43
mostly cluster around one in the
02:46
affected population clusters around
02:48
eight using a cut-off of four what you
02:53
would find is that there is a 100%
02:55
detection rate with a zero false
02:58
positive rate this is largely because
02:59
these two groups do not overlap when
03:02
groups do overlap such as these two
03:04
groups with one group clustered around
03:06
one and one group clustered around five
03:08
where you place your cutoff for your
03:10
screening test will drive your detection
03:13
rate as well as your false positive rate
03:15
what you can see here with the cutoff of
03:17
four is that the detection rate is 80%
03:20
and the false positive rate is 0%
03:23
because really were way above the curve
03:25
of the unaffected population however
03:28
we’re not picking up 20% of the
03:30
population that is affected using a
03:34
cut-off of two what you see here is that
03:37
there is a 100% detection rate because
03:40
the affected curve is completely above
03:42
the cutoff of two but there is also now
03:45
a false positive rate of 15% changing
03:49
the cutoff to three is probably the most
03:51
ideal for this situation here the
03:54
detection rate is 95% while at the same
03:57
time the false positive rate is 2% this
04:00
would be the best cutoff for a screening
04:02
test in these two populations now let’s
04:06
use neural tube defects and
04:07
alpha-fetoprotein to apply some of these
04:09
principles of screening and then we will
04:11
move on to screening test done in early
04:13
pregnancy neural tube defects are the
04:15
second most frequent major congenital
04:17
anomaly in pregnancy forty five percent
04:19
of these will be in encephalo where
04:22
there’s a lot of the top portion of the
04:24
brain as can be seen the bottom-left
04:26
pictures the other forty five
04:28
as spina bifida where there’s a weakness
04:30
in the spine and the final 10% is a
04:32
condition called encephalocele
04:34
as you can see in the picture of the
04:36
baby with the large opening in the back
04:38
of its head the overall incidence of
04:41
open neural tube defects in the u.s.
04:42
population is approximately 1 to 2 per
04:44
1,000 births a previously affected child
04:47
increases the risk more than tenfold
04:49
however 90% of open neural tube defects
04:51
have no known risk factor and this means
04:53
that there is a need for screening for
04:55
the lowest population looking at the
04:58
incidence based on risk factors again
05:00
the general population has an incidence
05:01
of 1.5 per 1,000 births for a diabetic
05:04
mother it’s 20 per 1,000 births valproic
05:07
acid use is 10 per 1,000 births one
05:10
prior sip lling with an open roll tube
05:12
defect gives an incidence of 15 to 30
05:14
per 1,000 births to prior siblings with
05:17
oprah neural tube defect gives an
05:18
incidence of 57 per 1,000 births and
05:20
having a parent with an open neural tube
05:22
defect does increase your risk to 11 per
05:25
1000 births alpha-fetoprotein is a
05:28
protein produced by the fetal liver
05:30
fetal levels peak at about 12 weeks
05:32
gestational age this then moves into the
05:34
amniotic fluid and the amniotic fluid
05:36
levels peak at about 15 weeks and the
05:38
maternal serum levels rise steadily
05:40
until about 32 weeks there is a linear
05:42
rise from 15 to 20 weeks and this is
05:45
helpful in terms of screening here’s a
05:47
picture of the rise and
05:49
alpha-fetoprotein from 15 to 20 weeks
05:52
looking at the distribution of maternal
05:54
serum alpha-fetoprotein the unaffected
05:57
population does over lie patients with
05:59
open spina bifida and those within and
06:02
separately but what you can see is that
06:04
with spina bifida and anencephaly the
06:06
average and the distribution of AFP
06:09
levels are higher and higher focus on
06:11
this picture on the maternal serum AFP
06:13
level cutoff of 2.5 multiples of the
06:16
median and how this is at the far right
06:19
end of the unaffected and begins to
06:21
enter into the areas of open spina
06:23
bifida and anencephaly so you can see
06:26
that open neural tube defects can be
06:28
screened with maternal serum
06:29
alpha-fetoprotein and using a 2.5
06:32
multiples of the median cutoff ninety
06:35
percent of an assembly will be detected
06:36
eighty percent of spina bifida will be
06:38
detected and there is only a three
06:41
percent false
06:41
positive rate elevated maternal serum
06:44
AFP can also be seen with these defects
06:47
here this includes ventral wall defects
06:49
triploid e aneuploidy amniotic band
06:52
sequence de pentalogy of Cantrell renal
06:54
agenesis multiple gestation x’
06:56
congenital necrosis sacrococcygeal
06:59
teratoma dermatological conditions in
07:02
Cory ng ona ultrasound can also be used
07:05
in the screening of spina bifida using
07:08
an ultrasound to detect open neural tube
07:10
defects it’s important to first
07:11
recognize what normal parts of the fetus
07:13
look like this image shows normal
07:15
cervical and thoracic spine views with
07:17
the small white dots that are continuous
07:19
like a train track below
07:20
this image shows normal lumbar and
07:22
sacral spine use in this picture this is
07:26
a normal closed vertebral body and in
07:29
this image you see normal cranial views
07:31
of the fetal head moving on to what
07:34
you’ll see with spina bifida the orange
07:36
arrow is pointing to an opening in the
07:38
fetal spine this is a spine in the
07:39
longitudinal view here as well you can
07:42
see a splaying of the fetal spine with
07:45
spina bifida as this is an open oral
07:46
tube defect in this view looking at the
07:49
spinal processes as identified by the
07:51
red arrow you can see that it is open
07:53
and the orange arrow is pointing to the
07:55
meningocele
07:56
that is protruding from the back of the
07:58
baby in this transverse view you can
08:01
again see the meningocele protruding
08:03
from the back of the baby right where
08:05
the orange arrow is pointing when a
08:07
spina bifida is president there’s also
08:09
changes in the fetal cranium
08:10
here you see eleven sign with a red
08:12
arrow as indentations in one part of the
08:15
cranium the orange arrow points to an
08:17
enlarged lateral ventricle moving on to
08:21
discuss chromosomal abnormalities
08:23
there are several chromosomal
08:24
abnormalities that can be detected with
08:26
early pregnancy screening these include
08:28
the aneuploidies such as trisomy 21 18
08:31
and 13 as well as sex chromosome
08:33
abnormalities such as 45 X or Turner
08:36
syndrome also triploid II which is a
08:38
complete triple copy of the chromosomal
08:40
set these can be translocations as well
08:42
as deletions duplications and inversions
08:44
trisomy 21 is known as Down syndrome
08:47
this occurs in approximately one out of
08:48
a thousand births the typical phenotype
08:50
is short stature classic facies
08:53
developmental delay and mental
08:54
retardation the
08:55
associated anomalies such as cardiac
08:57
defects Doisneau stenosis or atresia and
09:00
short limbs the average life expectancy
09:01
is 50 to 60 years of age trust me 18 is
09:05
known as Edwards syndrome this occurs in
09:07
one out of five thousand live births
09:09
the typical phenotype includes short
09:11
stature clenched fists overlapping
09:13
digits and rocker-bottom feet The
09:15
Associated physical anomalies include
09:17
tetralogy of flow omphalocele congenital
09:19
diaphragmatic hernia neural tube defects
09:22
and choroid plexus cysts only five to 25
09:24
percent of patients with trisomy 18 live
09:27
past two years of life last is trisomy
09:30
13 also known as potato syndrome this
09:32
occurs in one out of 10,000 to 20,000
09:35
live births and there are many
09:37
associated anomalies including hole
09:38
approximately cleft lip and palate
09:40
cystic hygroma single nostril or absent
09:42
nose
09:43
um fallacy on cardiac anomalies
09:45
including hypoplastic left heart
09:46
clubfoot or club hand polydactyly and
09:49
overlapping fingers 85% of these
09:51
patients will not live past the first
09:53
year of life in terms of the various
09:56
pregnancy screening options it’s
09:57
important to keep in mind that the
09:59
diagnostic interventions are chorionic
10:01
villus sampling and amniocentesis these
10:03
require a small needle to be placed in
10:05
the pregnancy which can disrupt the
10:07
pregnancy and cause miscarriage or
10:08
pregnancy loss
10:09
this occurs in 23 out of 1,000
10:11
pregnancies that undergo CVS and 7 and
10:14
1,000 pregnancies that undergo
10:16
amniocentesis the screening options
10:18
include age based screening and then
10:20
moving on to the more modern screening
10:22
tests of second trimester analytes which
10:24
our hormones and proteins made by the
10:26
pregnancy first trimester analytes both
10:29
of these have some incorporation of
10:30
ultrasound and finally the newest
10:32
technology is cell free field DNA in
10:36
terms of age based screening prior to
10:38
the advent of ultrasound and serum
10:40
analytes physicians would screen women
10:42
based on maternal age to select women at
10:44
highest risk for amniocentesis the age
10:46
cutoff was somewhere between 35 to 37
10:49
years old and this was when the risk of
10:51
miscarriage after amniocentesis
10:53
approximated the risk of Down syndrome
10:55
based on the woman’s age for this reason
10:58
advanced maternal age was set at 35
11:00
years old age based screening generally
11:02
identified 30% of cases with Down
11:04
syndrome by offering amniocentesis to
11:06
the oldest 5% of the population
11:09
what we’ve seen is that the age of the
11:10
pregnant population is increasing and
11:12
there are more and more women having
11:13
pregnancies later in life with the
11:16
availability of the alpha-fetoprotein
11:18
tests identified early on as a marker
11:20
for open neural tube defects in 1984
11:23
armored cats at all found that there was
11:25
an association of aneuploidy with low
11:27
values of maternal serum alpha-theta
11:29
protein his group and another group went
11:32
back and looked at banks stored serum
11:34
and linked these with Down syndrome and
11:36
analyzed them and what was found was
11:38
that between 14 to 22 weeks that the
11:41
median AFP was approximately 25 percent
11:43
lower in pregnancies associated with
11:45
Down syndrome after that time new second
11:49
trimester hormones and proteins were
11:51
found which were also markers for
11:53
aneuploidy the triple screen includes
11:54
alpha-fetoprotein made by the fetal
11:57
liver estriol made by the placenta and
11:59
the fetus in beta HCG made by the
12:01
placenta these three values have an
12:03
overall 70 percent sensitivity with a
12:05
five percent false positive rate and a
12:07
thirty five year old woman to detect
12:09
Down syndrome the quadruple screen
12:11
includes alpha-fetoprotein made by the
12:13
fetal liver estrella made by the fetus
12:15
and the placenta beta HCG made by the
12:17
placenta and inhibin a made by the
12:19
placenta as well as the ovary these four
12:21
values have an overall 81 percent
12:23
sensitivity with a five percent false
12:25
positive rate for a woman who is 35
12:27
years old to detect Down syndrome what
12:30
was found over time also was that moving
12:32
from age based screening to the triple
12:34
screen and onto the quad screen overall
12:36
decreased the annual synthesis rate
12:38
looking at the number of amniocentesis
12:39
needed to be performed to diagnose one
12:42
Down syndrome case using age required
12:44
125 the triple screened 54 and the quad
12:47
screen 43 this overall resulted in less
12:50
pregnancy losses with 2500 happening
12:53
using age based screening 1500 with the
12:55
triple screen and 1300 with the quad
12:57
screen there is an increase in
12:59
sensitivity with a decrease in the false
13:01
positive rate looking specifically at
13:03
quad screen values at 16 weeks for
13:05
pregnancies with trisomy 21 there is low
13:07
alpha-fetoprotein low estriol and
13:09
elevated levels of HCG and inhibit which
13:12
tries to me 18 there are low values for
13:14
all of the four analytes in the quad
13:16
screen trisomy 13 really particularly
13:18
depends on the abnormalities that are
13:20
present in the fetus and as men
13:22
early on with okra no treat defects
13:24
there’s an increase in alpha-fetoprotein
13:27
incorporating ultrasound into the serum
13:29
analytes also adds to knowledge about
13:31
the pregnancy it is known that with a
13:33
genetic sonogram there are phenotypic
13:35
features of the fetus that can be used
13:37
to adjust the likelihood ratios based on
13:39
the serum screening alone especially for
13:41
Down syndrome this really needs to be
13:43
based on population and this can be used
13:45
over all really just to reduce the risk
13:47
of aneuploidies if none of these
13:49
features are present the main features
13:52
that are looked at are as follows nuchal
13:54
thickening Harper called bowel short
13:56
humorous short femur and echogenic focus
13:58
and pile ethicists before looking at how
14:01
these change the likelihood ratio let’s
14:03
see what some of these look like on
14:04
ultrasound in this picture you can see a
14:07
thickening of the back of the baby’s
14:09
neck called nuchal fold thickening that
14:11
is where the arrow and the ultrasound
14:13
picture and the two arrows on the back
14:15
of the fetuses head and the picture
14:18
Micha genic bowel is whitening of the
14:21
fetal bowel and this can be seen as the
14:23
white in the area of the arrow which is
14:25
also in the area of the fetal abdomen
14:28
the humerus and femur are long bones
14:31
which pretty much show up as straight
14:33
white lines on ultrasound what you can
14:34
see in this ultrasound picture is that
14:36
the average gestational age of this
14:38
fetus is supposed to be 23 weeks in one
14:40
day and this femur is measuring 20 weeks
14:42
in two days an inch our cardiac academic
14:46
focus as a small white dot that is
14:48
present in the fetal heart as can be
14:50
seen by the arrow in this picture
14:52
and pie electus is is an increase of
14:55
fluid seen in the kidney as can be seen
14:57
by this small black circle with the two
15:00
arrows pointing to it these ultrasound
15:03
findings can change the likelihood ratio
15:04
for isolated markers of Down syndrome
15:06
the likelihood ratio is most increased
15:09
by seeing an increase in nuchal
15:11
thickness hyper acog bowel also
15:13
increases the likelihood of Down
15:15
syndrome also a short humerus is more
15:18
likely than a short femur and echogenic
15:20
focus and pilot assists are not nearly
15:22
as strongly associated as the other
15:24
findings this eventually led to what is
15:27
known as the first trimester combined
15:29
screen the nuchal translucency thickness
15:31
is able to measure in the first
15:33
trimester this picture right here shows
15:35
an increased nickel
15:36
thickness in a first trimester fetus
15:38
when combined with pregnancy associated
15:40
plasma protein a and free beta HCG this
15:44
is known as the combined first trimester
15:46
screen and is very helpful and reliable
15:49
similar to the second trimester
15:50
screening looking specifically at the
15:53
nuchal thickness the more thick the new
15:55
Col thickness becomes the more likely
15:57
this is associated with aneuploidy at 2
15:59
millimeters or less the risk of
16:01
aneuploidy whether it’s trisomy 21 18 or
16:03
13 is approximately 1% as the nuchal
16:06
thickness increases to 3 millimeters
16:07
this overall aneuploidy risk increases
16:10
to 17% and greater than 3 millimeters
16:12
nuchal thickness is associated with a
16:14
67% risk of aneuploidy there are many
16:18
advantages of first trimester or serum
16:20
screening these include early detection
16:21
a similar sensitivity in false positive
16:24
rate to second trimester screening these
16:26
can be followed up with an early
16:27
diagnostic test and allowed the family
16:29
to make decisions about pregnancy
16:30
termination which is safer when done in
16:33
the first trimester the disadvantages
16:35
include that the first trimester serum
16:37
screen may over detect cases destined to
16:40
spontaneously abort also it does not
16:41
screen for open neural tube defects and
16:43
the diagnostic tests which at this point
16:46
would be chorionic villus sampling
16:47
compared to meö synthesis has more risk
16:49
also there’s a very small testing window
16:51
and the first trimester serum screening
16:53
needs to be performed at 11 to 13 weeks
16:57
finally I’d like to mention briefly cell
17:00
free fetal DNA it has been known for a
17:02
long time that fetal cells and field DNA
17:04
end up in the maternal circulation it is
17:06
possible to obtain this genetic material
17:08
through a simple maternal blood draw
17:09
amplification of small amounts of the
17:11
fetal DNA from the maternal circulation
17:13
can be performed using massive parallel
17:16
sequencing what ends up happening is
17:17
that these tests evaluate the relative
17:19
ratio of fetal chromosome DNA for
17:22
trisomy 21 13 and 18 and compare those
17:25
to the maternal DNA present for those
17:27
chromosomes these tests end up being 98
17:29
to 99 percent accurate was no rest the
17:31
fetus the advantages of cell-free fetal
17:35
DNA include detection as early as eight
17:38
to ten weeks a sensitivity greater than
17:40
98% and a false positive rate of
17:42
approximately 0.2% it is minimally
17:44
invasive and is not dependent on
17:45
ultrasound the disadvantages is that up
17:47
until recently this could not be used
17:49
for twins but the
17:50
is changing it is not useful in the
17:52
setting of placental mosaicism which is
17:54
extremely rare cell-free fetal DNA only
17:56
screens for common employees and for
17:59
certain women if there’s a low fetal
18:01
fraction this cannot be performed and
18:04
approximately 2 to 6% of pregnancies and
18:06
this is particularly true for the obese
18:08
mother well that’s about it everybody I
18:10
think that we’re able to review some of
18:12
the foundational principles related to
18:13
screening tests discuss the more common
18:15
and employees on neural tube defects
18:16
that can be identified through early
18:18
pregnancy screening we introduced serum
18:19
and ultrasound screening through the use
18:21
of alpha-fetoprotein to detect over
18:23
neural tube defects we understood the
18:24
strengths and limitations of first and
18:26
second trimester serum and ultrasound
18:27
screening and finally we described the
18:29
cell-free fetal DNA and its role in
18:31
pregnancy screening thanks so much for
18:33
watching the video we hope you find it
18:34
helpful good luck with everything and
18:36
we’ll see you in class
18:36
take care
18:37
[Music]
18:42
you
Duration 17:57
all right we now move to chapter three
00:08
obstetric all procedures and the first
00:11
one that we will talk about is obstetric
00:14
ultrasound obstetrical ultrasound has
00:16
totally revolutionized pregnancy care
00:19
when I started my residency in the 1970s
00:25
it was just beginning and the changes
00:28
that we’ve seen in obstetric ultrasound
00:31
are just amazing I don’t think it is
00:34
possible for a patient to get through
00:37
pregnancy in the United States with
00:39
regular prenatal care without getting at
00:42
least one ultrasound ultrasound is an
00:45
imaging modality with low energy high
00:49
frequency sound waves it has probably
00:52
been studied more than any other imaging
00:55
method to see if there are any
00:58
abnormalities and effects on the fetus
01:00
and at the low energy high frequency
01:03
waves that we use today no one has shown
01:06
any adverse effects on the embryo and
01:09
fetus but it always could be that we
01:12
haven’t looked long enough yet so we
01:14
always need to be concerned with that
01:15
the early ultrasounds were trans
01:18
abdominal trans abdominal can be used
01:22
any time during the pregnancy but the
01:24
image quality may not be as good it
01:28
depends on the body mass index of the
01:30
patient it depends on the presence of
01:34
scars in the skin the trans abdominal is
01:38
not very helpful if you have a three or
01:40
four hundred pound patient the benefit
01:42
of a transvaginal is it can be used in
01:46
any patient whether she’s a hundred
01:48
pounds or whether she is four hundred
01:49
pounds because you get the transducer in
01:53
the vagina close to the pelvic organs
01:55
you have very high resolution images the
02:00
dating accuracy of a first trimester
02:01
ultrasound is plus or minus five days
02:05
which is pretty good
02:07
the Doppler ultrasound we can use to
02:11
assess blood flow and as we will talk
02:13
about
02:14
with fetal antepartum testing we can
02:17
look at umbilical artery blood flow and
02:20
look at diastolic and systolic flow and
02:22
when we’re assessing for fetal anemia
02:25
with a low immunization we can do
02:28
fetal middle cerebral artery blood flow
02:30
and we look at the peak systolic
02:32
measurements in those situations this is
02:36
a wonderful image it is 12 weeks and 3
02:40
days and it shows the fetus in a
02:42
sagittal plane you can see that the
02:45
skull is intact you can see that there
02:48
is normal-appearing spine
02:50
there is no spina bifida you can see the
02:53
abdominal wall is intact
02:55
there’s no omphalocele or gastroschisis
02:58
we can see the mandible the maxilla we
03:01
can see the nasal bone this is a
03:05
beautiful appearing normal first
03:08
trimester ultrasound and the accuracy in
03:10
terms of dating is plus or minus five
03:13
days the indications for obstetric
03:16
ultrasound are many in fact you could
03:19
almost say that there is an indication
03:22
for every pregnancy in terms of ectopic
03:25
pregnancy to identify is it in the
03:28
uterus that’s something we talked about
03:30
viability to see is there cardiac motion
03:33
we talked about that when we’re looking
03:36
at first an early pregnancy bleeding
03:38
gestational age dating is very important
03:42
and the earlier in pregnancy the
03:44
ultrasound dating is performed the more
03:47
accurate is if there are subsequent
03:50
ultrasounds we do not change the due
03:53
date we just look to see is there
03:55
appropriate or inappropriate growth
03:58
multiple gestation twins and triplets
04:01
and quadruplets the only way to
04:03
definitively diagnose that is by
04:05
obstetrical ultrasound amniotic fluid
04:08
volume is part of our modified
04:11
biophysical profile which we’ll talk
04:13
about later on if the uterus is smaller
04:15
than dates all ago Hydra Menace may be a
04:19
cause for that we can assess serial
04:21
measurements for fetal growth that’s
04:23
going to be important in patients who
04:25
have chronic hypertension
04:27
we have diabetes they may be the fetuses
04:30
is too small or the fetus isn’t growing
04:32
adequately we can evaluate fetal
04:35
well-being with ultrasound specifically
04:37
with a biophysical profile where we look
04:40
at gross body movements we look at
04:42
extension and flexion of extremities we
04:44
look at breathing movements the
04:46
assessment of fetal anomalies is going
04:48
to be important as we do the genetic
04:50
sonogram to identify is there a placenta
04:53
previa where there is pregnancy bleeding
04:56
and as I talked about just a minute or
04:58
so ago with fetal anemia we can look at
05:01
the middle cerebral artery peak systolic
05:04
velocity to see if there’s evidence of
05:06
fetal anemia we’ll talk more about that
05:08
under a low immunization the genetic
05:11
ultrasound is a procedure which is no
05:15
different than any other ultrasound but
05:17
it is performed specifically to identify
05:20
if there are any abnormalities
05:21
specifically anatomic markers of fetal
05:24
aneuploidy the ideal time to do the
05:27
genetic ultrasound is 18 to 20 weeks now
05:30
let me just say that this is not a
05:32
diagnosis of aneuploidy but what it will
05:35
do is to change the risk of aneuploidy
05:39
because if you have a normal genetic
05:42
ultrasound it cuts your predicted risk
05:45
of fetal aneuploidy by half in other
05:48
words if the likelihood of a given
05:51
woman’s age let’s say at age 35
05:54
you have likelihood of Down syndrome of
05:56
one in 300 with a normal ultrasound it
06:00
would be 1 in 600 so the generic things
06:03
that we look for or any structural
06:05
abnormalities is there any evidence of
06:07
any kind of syndromes and there are
06:09
hundreds if not thousands of syndromes
06:11
but the specific areas that we will look
06:14
for which are called genetic markers for
06:17
aneuploidy would be neutral skin fall
06:19
thickness which would be at the junction
06:22
of the neck and the thorax in the head
06:24
the shortened long bone specifically the
06:27
humerus and the femur PI Alexis’s is
06:30
where we have enlargement of the renal
06:32
pelvis
06:33
echogenic intracardiac focus you can see
06:36
when you look at the heart that there is
06:39
echogenic
06:39
areas
06:40
which are very clear and the densities
06:44
should be equal to that of bone and then
06:46
is hyper echoic bowel which is also
06:49
associated with it so these are the five
06:51
areas that we look for with the nuclear
06:53
skinfold being the one that is the
06:55
strongest predictor the nuclear
06:57
transitions or NT measurements is a
07:01
fairly recent screening test which is
07:04
performed in the first trimester which
07:07
is between 10 and 14 weeks and it
07:10
measures the fetal fluid collection
07:12
behind the neck a thickened and T
07:15
measurement increases the likelihood of
07:18
aneuploidy and cardiac disease we
07:21
combine the NT measurement with two
07:24
maternal blood tests which is free beta
07:27
HCG and pap A which is pregnancy
07:31
associated plasma protein a and by
07:34
looking at the levels of these two blood
07:36
tests along with the NT screening we can
07:39
come up with a number giving sensitivity
07:41
and specificity for aneuploidy screening
07:44
so the second trimester screening is a
07:47
quadruple marker screen which has four
07:49
blood tests the first trimester
07:51
screening has two blood tests and the NT
07:55
or nuchal translucency measurement this
07:59
ultrasound image shows very well the NT
08:03
the nuchal translucency and you can see
08:05
down in the lower middle part of the
08:08
image the NT measures 2.1 millimeters
08:14
you can also see that they have marked
08:18
the NB the nasal bone and they’re also
08:23
looking at the angle between the nasal
08:25
bone and the head you can also see the
08:27
mandible and maxilla these findings can
08:31
be very helpful in identifying normality
08:34
and they’re very reassuring if things
08:36
look like they should chorionic villus
08:40
sampling is an outpatient office
08:43
procedure performed under ultrasound
08:46
guidance without anesthesia it can be
08:50
done either tran cervical e or done
08:53
transferred
08:54
a catheter is placed into the precursor
08:59
for the placenta which is the chorionic
09:02
villus it does not enter the amniotic
09:06
cavity it does not go into where the
09:09
fetus is but it takes part of the
09:12
placental tissue a sample is sent to the
09:15
laboratory for karyotyping because this
09:19
is an invasive procedure there is a low
09:23
but real pregnancy loss rate which we
09:26
quote at 0.7% the basis of the chorionic
09:30
villus sampling or CBS is that the
09:33
origin of the placenta and the origin of
09:37
the fetus were both the same namely the
09:41
zygote
09:42
so whatever the chromosomes of the
09:44
zygote were should be the chromosomes of
09:48
the fetus and should be the chromosomes
09:50
also of the placenta so if we identify
09:54
normal placental chromosome it is highly
09:59
likely that the fiel karyotype is normal
10:02
as well there is a very low rate of
10:07
placental mosaicism in other words the
10:09
placenta may be abnormal but the fetal
10:12
chromosomes are normal that’s about one
10:15
in a thousand so this is chorionic
10:17
villus sampling and this is a first
10:19
trimester procedure with the CBS you do
10:23
not have any assessment of neural tube
10:27
defects when you do an amniocentesis and
10:29
you take amniotic fluid you can do
10:31
amniotic fluid AFP so the CBS patients
10:35
are going to have to have the second
10:38
trimester blood test drawn to assess for
10:41
neural tube defects probably the most
10:44
common invasive obstetric or procedure
10:48
is amniocentesis this is an outpatient
10:51
procedure which is performed after 15
10:54
weeks the reason it isn’t performed
10:56
between 15 weeks is because there isn’t
10:58
enough amniotic fluid and if you
11:00
aspirate the fluid you can have an
11:02
increased pregnancy loss a needle is
11:05
placed into a pocket of amniotic
11:07
fluid under direct ultrasound guidance
11:10
so you’re actually watching as the
11:12
needle goes through the abdominal wall
11:14
through into the amniotic sac and then
11:17
you aspirate amniotic fluid the amniotic
11:20
fluid contains these living fetal cells
11:24
which are shed off from the fetal skin
11:26
which are called amnio sites and fetal
11:29
karyotyping can be performed on the
11:31
amnio sites you can also do the amniotic
11:34
fluid AFP more definitive test the
11:37
maternal serum AFP is not as specific
11:41
and as sensitive as is the amniotic
11:43
fluid AFP so we will do that in addition
11:46
most commonly if we have the very
11:48
precious amniotic fluid we’ll probably
11:50
do a chromosomes even if the main
11:53
purpose is to look for in neural tube
11:55
defect the pregnancy last rate is about
11:58
one in 200 which is about the same as a
12:02
likelihood of finding aneuploidy at age
12:04
35 this is an artist conception of an
12:09
amniocentesis and you can see the blue
12:12
ultrasound transducer which is being
12:15
held on the abdomen by the
12:17
ultrasonographer you can see that there
12:20
is a placenta which is in the fundus of
12:22
the uterus this fetus is in cephalic
12:25
presentation with the head down and the
12:28
needle is placed directly under
12:30
ultrasound guidance into the amniotic
12:32
sac and you can see the aspiration of
12:34
the amniotic fluid with the amnio sites
12:39
within it pregnancy loss rate is about
12:42
half a percent
12:44
percutaneous umbilical blood sampling or
12:47
pubb’s is another invasive procedure a
12:51
needle is placed trans abdominally goes
12:54
into the umbilical vein and we aspirate
12:58
fetal blood this is done under direct
13:02
ultrasound guidance after 20 weeks
13:04
gestation and the reason it isn’t done
13:06
before 20 weeks gestation is because the
13:09
umbilical vein is so small so tiny is
13:12
difficult to get a needle in and when
13:15
you try to do pubb’s very early it has a
13:18
significant pregnancy loss rate
13:21
this is done trance abdominal II it can
13:23
be diagnostic it can be therapeutic in
13:26
terms of diagnosis we can assess blood
13:29
gases of the fetus we can assess carrier
13:33
typing of the fetus we can assess IgG
13:36
IgM antibodies you can do electrolytes
13:40
on the blood in terms of therapy we can
13:44
do any treatment transfusion if we have
13:46
fetal anemia which we will talk about
13:49
later on under a low immunization when
13:52
you go in through the uterine wall you
13:55
can irritate the uterus you could have
13:57
preterm contractions you you have to go
14:00
through the membrane so you could
14:02
potentially rupture the membranes
14:04
pregnancy loss rate is not high but it
14:07
is higher than amniocentesis it is one
14:09
to two percent pregnancy loss rate the
14:13
last procedure that we will talk about
14:15
is fetus copy this is performed with a
14:18
fiber-optic scope it is done in the
14:21
operating room after 20 weeks gestation
14:25
under general anesthesia typically this
14:30
scope is going to be larger than a
14:32
needle and so the likelihood of
14:35
rupturing membranes is higher the
14:37
likelihood of preterm labor is higher
14:40
the pregnancy loss rate is 2 to 5
14:42
percent clearly the loss rate will be a
14:46
function of the experience of the
14:50
operator the more of these you’ve done
14:52
the less problems you’ll have
14:54
indications for this would be
14:56
intrauterine surgery and what is done
14:58
more and more lately is to do laser
15:02
vaporization of placental vessels which
15:05
are joining to fetuses with twin twin
15:09
transfusion syndrome and if you don’t do
15:12
a laser ablation before the pregnancy
15:16
goes much further you can get either
15:18
loss of both twins or one twin up to 80%
15:20
of the time so this is going to be
15:22
important
15:22
there are rare situations in which you
15:24
need to do a fetal skin biopsy and this
15:27
would be another indication for fetus
15:28
copy the risks bleeding infection
15:31
rupture of membranes and fetal loss this
15:34
is the highest
15:35
pregnancy loss rate of any of the
15:37
procedures this is a artist’s conception
15:41
of a fetus cope which is placed into the
15:45
uterus and you can see we have two
15:47
fetuses one which is stuck on the bottom
15:51
of the uterus with Allah goyim Nia’s the
15:53
other one which is floating in
15:55
polyhydramnios this is a twin twin
15:57
transfusion syndrome and the fetus cope
16:01
is being used to laser the connection
16:04
between the twin
16:05
okay let’s summarize what we have just
16:08
said this is on prenatal diagnostic
16:10
testing in your notes a chorionic villus
16:14
sampling is done between 10 to 12 weeks
16:16
of gestation with a pregnancy loss rate
16:19
of 0.7 percent and we aspirate placental
16:22
precursors the first trimester screening
16:25
is done between 10 and 14 weeks zero
16:28
pregnancy loss rate because none of
16:29
these are invasive procedures and this
16:31
involves the nuchal translucency and two
16:34
blood tests the pregnancy associated
16:35
plasma protein a and free beta HCG the
16:39
amniocentesis is the most common
16:41
invasive procedure is done at fifteen
16:43
weeks or more a 0.5 pregnancy loss rate
16:46
and we aspirate from the amniotic fluid
16:49
amniotes and amniotic fluid AFP we could
16:53
also do chromosome the expanded AFP you
16:57
can see is expanded with the X the X is
16:59
a shorthand for expanded AFP is now the
17:02
quadruple marker screen it is done
17:05
between 15 to 20 weeks go talk about
17:07
that coming up zero pregnancy loss rate
17:09
because it’s non-invasive and the four
17:12
tests that we do are maternal serum AFP
17:15
beta HCG estriol
17:16
and inhibin a the sonogram is probably
17:19
the most common prenatal diagnostic
17:22
procedure done between 18 to 20 weeks
17:24
zero pregnancy loss rate it is
17:26
non-invasive and this involves a genetic
17:28
sonogram the fetus copy is done between
17:30
18 to 20 weeks with the 3 to 5 percent
17:33
pregnancy loss rate this can be lasering
17:36
the blood vessels in twin twin
17:38
transfusion syndrome and fetal biopsy
17:41
the percutaneous umbilical blood sample
17:43
or pubs is done at 20 or more weeks
17:46
gestation
17:47
we have a 1 to 2% pregnancy loss rate
17:49
and we aspirate blood from the umbilical
17:52
vein because that’s the largest vessel
17:55
and that’s the end of chapter 3