|
Clinical Warts
Condyloma acuminata, (venereal warts) are caused by a virus known as "Human
Papilloma Virus" (HPV).
 There are two categories of warts, clinical and subclinical. Clinical warts appear as
tiny, cauliflower-like, raised lesions around the opening of the vagina or inside the
vagina. These lesions appear flesh-colored or white, are not tender and have a firm to
hard consistency. If they are on the outside of the vagina or vulva, they are generally
symptomatic, causing itching, burning, and an uncomfortable sensation during intercourse.
If they are inside the vagina, they generally cause no symptoms. There are two categories of warts, clinical and subclinical. Clinical warts appear as
tiny, cauliflower-like, raised lesions around the opening of the vagina or inside the
vagina. These lesions appear flesh-colored or white, are not tender and have a firm to
hard consistency. If they are on the outside of the vagina or vulva, they are generally
symptomatic, causing itching, burning, and an uncomfortable sensation during intercourse.
If they are inside the vagina, they generally cause no symptoms.
Subclinical Warts
The second category, subclinical warts, are invisible to the naked eye, are flat and
colorless. They usually do not cause symptoms, although they may cause similar symptoms to
the raised warts. These subclinical warts can be visualized if the skin is first soaked
for 2-3 minutes with vinegar (3-4% acetic acid) and then viewed under magnification
(4-10X) using a green or blue (red-free) light source.
Venereal warts are not dangerous and have virtually no malignant potential. Clinical
warts may be a nuisance and so are usually treated. Subclinical warts are usually
not treated since they are not a nuisance (most people with subclinical warts are unaware
of their presence).
Treatment
Treatment consists of removal of the wart. This can be accomplished in any number of
ways, some more painful than others:
- Apply a small amount of bichloracetic acid (80-90%) directly to the wart, taking care to
avoid spreading the acid onto the normal surrounding skin. For larger lesions, use a
cotton-tipped applicator dipped in the acid. For smaller lesions, use the
"stick" end of the cotton-tipped applicator. Apply enough acid (very tiny
amounts) to cause the lesion to turn white, but not so much that it runs down onto the
normal surrounding skin. No anesthetic is necessary. The patient may feel nothing,
some slight tingling, or a minor stinging. After a minute or two, rinse the skin with warm
water to dilute any remaining acid and prevent it from coming into contact with the
surrounding skin.
- Cryosurgery can effectively remove warts. Freezing the wart with any convenient tool
(liquid nitrogen, cryosurgical probe, etc.) can be done without anesthetic and results in
sloughing of the wart in a week or two. Be careful not to freeze normal skin. Two
freeze-thaw cycles usually work better than a single freeze-thaw cycle.
- Podophyllum resin can be applied directly to the wart, followed by washing off the
residual podophyllin in 3-6 hours. This effective approach runs the risk of podophyllin
toxicity. This is a minor issue if the wart is very small and you use tiny quantities of
podophyllin. If you use large amounts, or apply it inside the vagina, toxicity is a real
issue.
Remember that in treating the warts, you are actually destroying the patient's skin
which has responded in a strange and annoying way to the presence of the HPV. You are not
getting rid of the HPV itself.
Persistence of Virus
HPV is a sexually-transmitted virus which usually causes no symptoms but occasionally
causes warts. The virus spreads throughout the skin of the vulva and vagina (as well as
the inner thighs and lower abdomen), where it disappears into the skin cells and usually
remains dormant forever. Like many other viruses, if the patient's immune system allows
the virus to grow, it can reappear and cause warts. This virus is extremely common,
infecting as many as 1/3 of the adult, sexually-active population. There is no known way
to eliminate the virus from all skin cells.
Transmission
Patients with HPV are contagious to others, but there is no effective way to prevent
its spread. Some physicians recommend condoms, but because the virus is found in areas of
the skin beyond the condom, this is not likely to be effective. Some physicians recommend
aggressive treatment of all warts, in the belief that active warts are more contagious
than inactive virus within the skin. This theory has not, so far, been proven to be true.
Evaluation
In any patient with venereal warts (condyloma), you should look for possible dysplasia
of the cervix. This is best done with colposcopy, but a simple Pap smear can be very
effective. Because HPV causes warts and is also associated with dysplasia, more frequent
Pap smears (every 6 months) is a wise precaution, at least initially.
If dysplasia is found, gynecologic consultation will be necessary, although this may be
safely postponed for weeks or months if operational requirements make consultation
difficult.
|

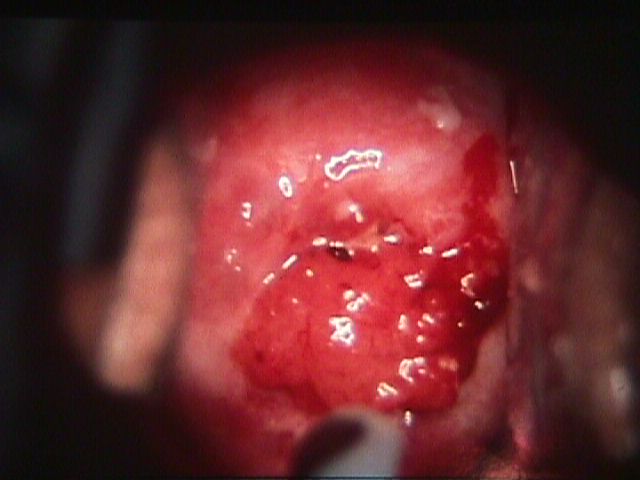
Condyloma at hymeneal ring

Apparently normal cervix

After application of acetic acid
Dysplasia
While warts are not considered dangerous, HPV infection is associated with another skin
change known as "dysplasia." Dysplasia means that the skin (mainly of the
cervix) begins growing faster than it should. There are different degrees of dysplasia:
mild, moderate and severe. None of these is malignant, but it is true that the next step
beyond severe dysplasia is cancer of the cervix.
About 1/3 of all adult, sexually-active women have been infected with HPV, but probably
less than 10% will ever develop dysplasia. Most (90%) of those with dysplasia will have
mild dysplasia which will either regress back to normal or at least will never progress to
a more advanced stage.
Relation to Cancer
Most women (About 90%) with mild dysplasia of the cervix will never develop a more
advanced problem, and often the abnormality regresses back to normal.
Most women with moderate to severe dysplasia of the cervix, if left untreated,
will ultimately develop cancer of the cervix. If treated, most of these abnormalities will
revert to normal, making this form of cervical cancer largely preventable.
Cervical dysplasia is usually a slowly-changing clinical problem. There is indirect
evidence to suggest that on average, it takes about 10 years to advance from normal,
through the various stages of dysplasia, and into cancer of the cervix. Of course, any
individual may not follow these rules. In providing medical care to women with cervical
dysplasia, good follow-up is important, but urgent medical evacuation is usually not
indicated for less threatening categories of dysplasia.
Cervical Cancer
|