|
Electronic fetal monitors continuously record the instantaneous fetal heart rate on the
upper channel and uterine contractions on the lower channel. They do this by attaching,
either externally (and non-invasively) or internally, to detect the fetal heart and each
uterine contraction.
Listen to a normal
fetal heart beat
 Labor is an inherently dangerous life event for a fetus and its
mother. In the majority of cases, everything goes smoothly enough and
ends happily. In a minority of cases, there are some problems.
Electronic fetal monitoring is used to provide: Labor is an inherently dangerous life event for a fetus and its
mother. In the majority of cases, everything goes smoothly enough and
ends happily. In a minority of cases, there are some problems.
Electronic fetal monitoring is used to provide:
-
Minute-by-minute information on the status of the fetus
-
Accurate historical information on fetal status and the
frequency/duration of contractions from earlier in labor.
-
Insight into the stresses on the fetus and its ability to tolerate
those stresses.
Originally, electronic fetal monitoring was thought to be able to
prevent such newborn problems as stillbirth, brain damage, seizure
disorders, and cerebral palsy. This hope proved to be overly optimistic.
Unfortunately, and contrary to earlier thinking, most of the problems
that lead to stillbirth, brain damage, seizure disorders and cerebral
palsy are not intrapartum problems, but have already occurred by the
time a patient comes in to labor and delivery. Nonetheless, electronic
fetal monitoring has proved so useful in so many ways that it has become
a prominent feature of intrapartum care, and indispensable for high risk
patients. 
Two forms of continuous electronic fetal heart monitoring
are used, internal and external. Internal monitoring provides the most
accurate information, but requires a scalp electrode be attached to the
fetus, and a pressure-sensing catheter to be inserted inside the uterine
cavity. Both of these require membranes be ruptured and both have small,
but not inconsequential risks. For that reason, they are usually used
only when the clinical circumstances justify the small increased risk of
complication.
External monitoring usually provides very good
information about the timing of contractions and the fetal response.
External monitoring consists of belts worn by the mother during labor
that record the abdominal tension (indirectly recording a contraction),
and the instantaneous fetal heart rate. External monitoring has the
advantages of simplicity, safety, availability, and reasonable
reliability under most general obstetrical circumstances. However, it is
subject to more artifact than internal monitoring, may not detect subtle
changes, and may not accurately record the information, particularly if
the mother is overweight or active. 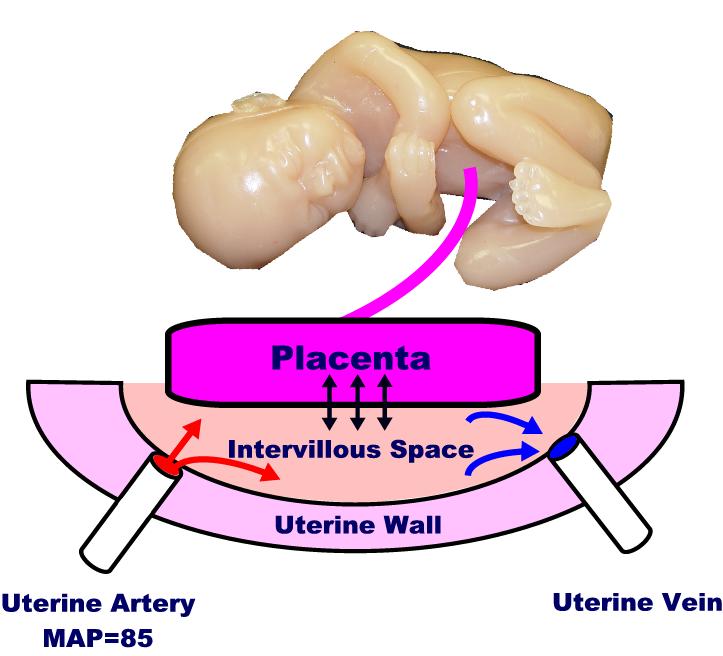
Uterine Blood Flow
Maternal blood flows to the uterus primarily through the uterine
arteries. The arteries branch out, once they enter the uterus, and
supply blood to the muscle cells of the myometrium, and through the wall
to the intervillous space (IVS). Once the maternal blood reaches the
IVS, it simply dumped into the space, where it drifts about until some
is drained off through the maternal venous system. Unlike the highly
controlled capillary circulation, there is little control over this
process. It is similar to a swimming pool (the IVS), where fresh water
is dumped in through a faucet (the maternal arterioles), while the
drains in the bottom of the pool (maternal venous system) sucks up any
available water that happens to be nearby.
The placenta floats on top of the IVS, with its chorionic villi
dipping down into the pool. Across the villous membrane pass oxygen,
carbon dioxide, nutrients and waste products. Some of this passage is
active transport (eg, glucose), some facilitated (eg, because of pH
gradient), and some is passive.
Many factors influence uterine blood flow delivery to the IVS,
including:
-
Maternal position (lateral, recumbant improves flow)
-
Maternal exercise (decreases flow)
-
Surface area of the placenta (placental abruption decreases flow)
-
Hypotension or hypertension (both decrease flow)
-
Uterine contractions (contractions reduce flow)
Once the maternal blood reaches the IVS, oxygen and nutrients must
still must traverse the villous membrane. If thickened (as with edema or
infection), then transvillous transport of materials will be impaired,
at least to some degree.
Listen to the Doppler sound of maternal blood flowing through the
uterine artery
Baseline Fetal Heart Rate
The baseline fetal heart rate is normally between 120 and 160 beats
per minute (110 to 160 at full term). This seems to be the range that
the normal, healthy fetus prefers to keep itself well-supplied with
oxygen and nutrients. The heart can be faster, but only at a cost of
increased energy utilization that is normally not justified. The heart
can beat slower, but if the bradycardia is prolonged, it can lead to
progressive tissue oxygen debt.
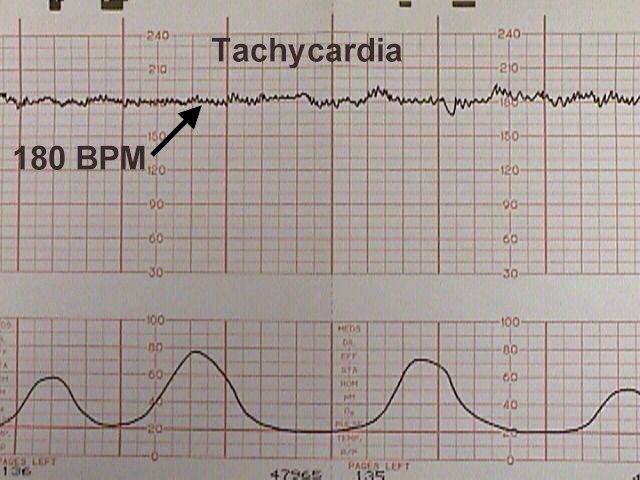
Tachycardia
Tachycardia is the sustained elevation of fetal heart rate baseline above a 160 BPM.
Tachycardia can be a normal response to some increased need for oxygen,
for example:
-
Increased fetal activity (everyone's heart rate goes up when we
exercise)
-
Maternal fever (with an elevated body temperature, all enzyme
systems speed up, increasing the need for oxygen on a metabolic basis)
It can also increase in the presence of more worrisome problems,
including:
Most tachycardias are not indicative of fetal jeopardy, particularly
in the absence of any other FHR abnormalities.
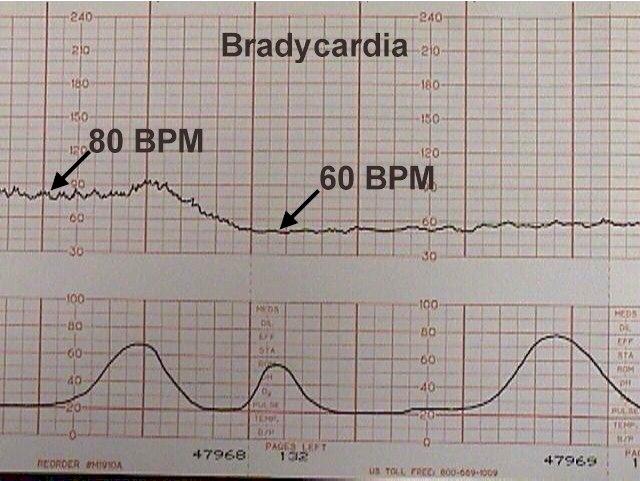
Bradycardia
Bradycardia is the sustained depression of fetal heart rate baseline below 120 BPM
(110 at full term).
Most of these are caused by increased vagal tone, although congenital cardiac
abnormalities can also be responsible.
Mild bradycardia (to 80 or 90 BPM) with retention of beat-to-beat variability is common
during the second stage of labor and not of great concern so long as delivery occurs
relatively soon. Moderate to severe bradycardia (below 80 BPM) with loss of beat-to-beat
variability, particularly in association with late decelerations, is more troubling and
may indicate fetal distress, requiring prompt resolution.
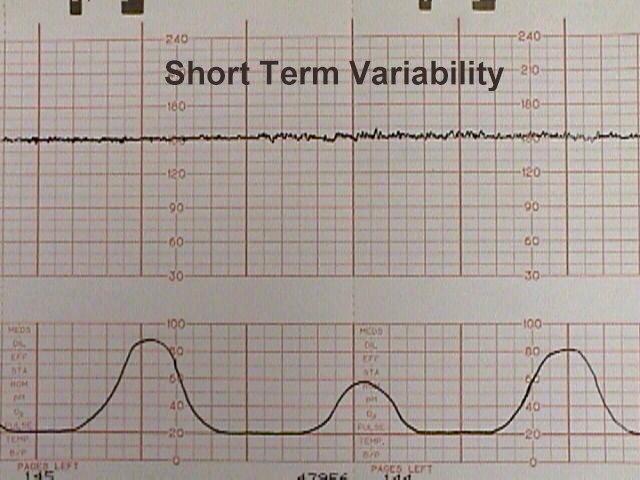
Variability
The normal fetal heart rate baseline is from 120 to 160 BPM and has both short and long-term
"variability." Short term variability means that from one moment to the next,
the fetal heart speeds up slightly and then slows down slightly, usually with a range of
3-5 BPM from the baseline.
Variability is normally controlled by the fetal brain through
sympathetic and parasympathetic influences. Reduced variability occurs
normally during fetal sleep and usually returns after 20 to 40 minutes.
Reduced variability may also occur:
-
Following narcotic administration
-
With fetal anomalies or injury
-
With hypoxia and acidosis in combination with such FHR
abnormalities as late decelerations, tachycardia, bradycardia, and
severe variable decelerations.
Persistent or progressively reduced variability is not, by itself, a
sign of fetal jeopardy. But in combination with other abnormalities may
indicate fetal intolerance of labor.
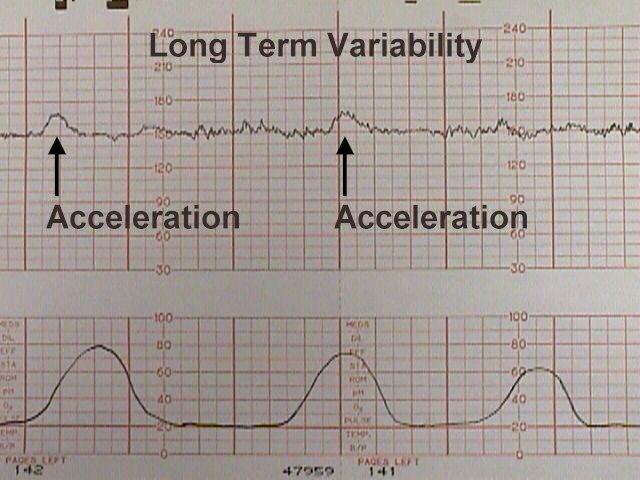
Long-term variability
Long-term variability represents broad-based swings in fetal heart rate, or
"waviness," occurring up to several times a minute. One form of long-term
variability of particular significance is a fetal heart "acceleration." These
usually occur in response to fetal movement, and are 15 BPM above the baseline or more,
lasting 10-20 seconds or longer. They can often be provoked by stimulating the fetal scalp
during a pelvic examination, or by acoustically stimulating the fetus with a loud,
obnoxious noise. The presence of fetal accelerations is reassuring that the fetus is
healthy and tolerating the intrauterine environment well.
During labor, no significance is attached to the absence of fetal accelerations.
Effect of Contractions
During a uterine contraction, blood flow through the uterus slows. If
the contraction is strong enough, all blood flow through it will stop.
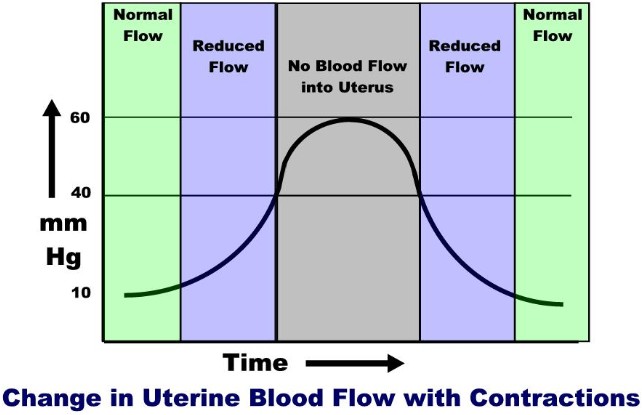
This decreased flow occurs because of the pressure gradients in the
system.
Maternal mean arterial pressure (MAP) is around 85 mm Hg. The
pressure on the inside of the uterus (at rest) is around 10 mm Hg. The
pressure within the uterine muscle (intramyometrial pressure or IMP) is
usually about 2-3 times that of the intra-amniotic pressure. Because of
these pressures, blood flows from the high pressure uterine arteries,
through the intramyometrial spiral arteries (and past the medium
pressure intramyometrial zone) and into the low pressure intravillous
space. From the IVS, blood is drained out through the even lower
pressure venous system and returned to the mother's circulation.
During a contraction, the intramyometrial pressures rise with the
increased muscle tone. As the compressive pressure rises, blood flow
through the spiral arteries diminishes (less pressure gradient to drive
the blood through them), and then stops when the IMP equals the MAP. The
IMP usually equals the MAP when the amniotic fluid pressure is around 40
mm Hg. (Remember that the intramyometrial pressure is 2-3 time that of
the amniotic fluid pressure). As the contraction eases up, blood flow
through the spiral arteries resumes and by the end of the contraction,
blood flow is back to normal.
Thus, with each contraction of any significance, there is initially
reduced blood flow to the intervillous space, then a cessastion of blood
flow, followed by a gradual resumption of blood flow.
On one level, you could imagine the danger of the fetal oxygen supply
being interrupted by each uterine contraction. On another level is the
realization that for a normal fetus, this interruption is nearly trivial
(similar to holding your breath for 5 seconds). But if the contractions
are coming too frequently (with very little time between contractions
for the fetus to resupply), or if the fetus already has a significant
problem, then contractions can pose a threat.
Contraction Patterns
During latent phase labor (prior to 4 cm), contractions may occur every
3-5 minutes and may or may not be painful.
A normal contraction pattern in
active labor shows contractions occurring about every 2-3 minutes and
lasting about 60 seconds.
-
If contractions are less
often than every 2-3 minutes in the active phase, labor may progress
more slowly, if at all. While less frequent contractions are the rule
in latent phase labor (prior to 4 cm), they are the exception in
active labor.
Coupling
Coupling means that two contractions occur one right after the other
rather than the normal pattern. Usually, coupling is followed by a
longer contraction-free interval. Tripling can also be seen where three
contraction occur without any significant recovery time.
If labor is progressing
normally, coupling can be ignored. Often, however, coupling is
associated with dysfunctional progress in labor. In these cases,
coupling can be treated with:
-
Rest
-
Hydration
-
Narcotics
-
Epidural Anesthesia
-
Oxytocin
Tachysystole
If contractions are persistently more often than 5 contractions in 10
minutes, this is called "tachysystole." Tachysystole poses a problem for
the fetus because it allows very little time for resupply of the fetus
with oxygen and removal of waste products. For a normal fetus,
tachysystole can usually be tolerated for a while, but if it goes on
long enough, the fetus can be expected to become increasingly hypoxic
and acidotic.
Tachysystole is most often
caused by too much oxytocin stimulation. In these cases, the simplest
solution is to reduce or stop the oxytocin to achieve a more normal and
better tolerated labor pattern. Other causes of tachysystole include:
-
Dehydration
-
Placental abruption
-
Pre-eclampsia
-
Amnionitis
In cases of spontaneous
tachysystole, increasing maternal hydration and placement in the lateral
decubitus position may slow the contractions.
|
Periodic Heart
Rate Changes
These heart rate changes are recurring throughout labor. They are
typically associated in some way with uterine contractions. There are
three basic recognized types:
-
Early Decelerations
-
Late Decelerations
-
Variable Decelerations
Each has its own features and clinical
significance. In addition, a fetus may demonstrate combined
decelerations (for example, a severe variable deceleration with a late
deceleration component.)
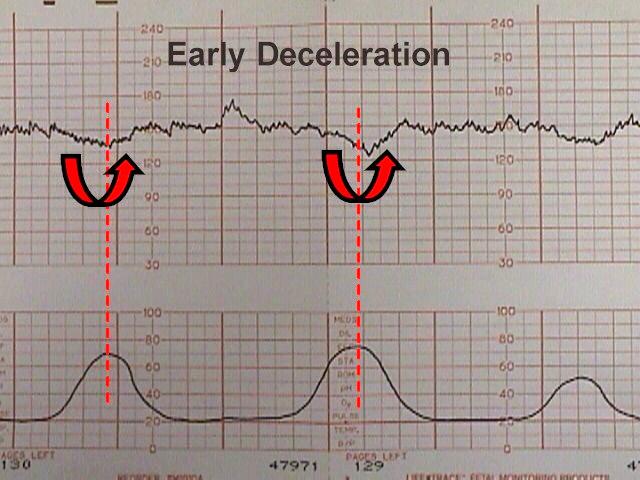
Early
Decelerations
Early decelerations are periodic slowing of the fetal heartbeat,
synchronized exactly with the contractions. These dips are rarely more
than 20 or 30 BPM below the baseline.
These innocent changes are thought to be
due, in many cases, to fetal head compression within the birth canal.
Sometimes, patients demonstrating early
decelerations will later develop variable decelerations (see below).
Late decelerations
Late decelerations are repetitive, gradual slowings of the fetal
heartbeat toward the end of the contraction cycle. They are felt to
represent some degree of utero-placental insufficiency.
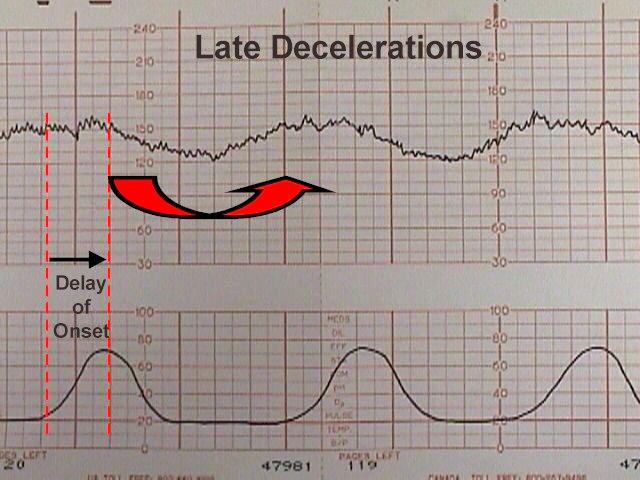
All
blood flow in and out of the IVS stops briefly during a contraction. A
normal fetus with normal reserve (oxygen in its bloodstream, in the
blood of the placenta, and in the intravillous space) will probably not
notice the tiny drop in total oxygen availability during these
contractions. But a fetus who has used up its reserve, or cannot
maintain its reserve will, over the course of the contraction, develop
some degree of hypoxia, hypercarbia and acidosis. This otherwise normal
fetus will respond by slowing its heart rate, to conserve energy. The
fetal heart is the largest consumer of oxygen in the fetus and if the
rate can be slowed, the fetus will survive longer on less oxygen. After
the contraction passes and fresh blood resupplies the intervillous
space, the hypoxia, hypercarbia and acidosis is eased and the fetal
heart rate returns to normal.
Clinically, the development of late
decelerations is a worrisome sign that the fetus has very little
reserve. Techniques that may be used to correct this problem include:
-
Changing maternal position to improve
uterine blood flow
-
IV hydration to increase maternal blood
volume, presumably leading to increased uterine blood flow
-
Administering oxygen to the mother to
try to get some additional oxygen through to the fetus. Of the three
standard treatments, oxygen administration is the least useful, since
the maternal hemoglobin oxygen saturation is likely already 99%. The
effect of breathing additional oxygen will probably have minimal
effect on the oxygen saturation.
-
Decreasing or discontinuing oxytocin
infusion to slow down or stop contractions that are provoking the
decelerations.
-
Tocolytic drugs to slow down or stop
contractions that are provoking the decelerations.
If the late decelerations are persistent
and non-remediable, this is considered "fetal distress," "fetal
intolerance of labor," or a "non-reassuring fetal heart rate pattern."
Such patients should be delivered promptly to avoid fetal injury or
death. Sometimes cesarean section is required to achieve prompt
delivery.
If persistent and not correctable, they
represent a threat to fetal well-being.
Variable Decelerations
Variable decelerations are variable in onset,
duration and depth. They may occur with contractions or between
contractions.
Typically, they have an abrupt onset and
rapid recovery (in contrast to other types of decelerations which
gradually slow and gradually recover.
Variable decelerations are thought to
represent a vagal response to some degree of umbilical cord compression.
If the umbilical cord is only slightly compressed, this will obstruct
the umbilical vein (low pressure system) which returns re-oxygenated
blood to the fetal heart. The initial normal fetal response to this is a
slight increase in fetal heart rate to compensate for the lack of blood
return and the slowly diminishing oxygen supplies. If this slight
increase in FHR is followed by a major drop in FHR, this phenomenon is
called a "shoulder."
As pressure on the umbilical cord
increases, the high-pressure umbilical arteries become occluded. When
this happens, there is an immediate rise in fetal blood pressure. 30% of
the fetal cardiac output goes to the placenta and if that flow is
blocked, the fetus will rapidly develop significant hypertension. The
normal fetus will respond to this hypertension by immediately slowing
the heart down by sending a signal through the vagus nerve. When the
umbilical cord obstruction is released, the vagal response disappears
and the fetal heart returns to normal.
If a mild degree of cord compression
continues (enough to continue to obstruct the umbilical veins for a
while), then another "shoulder" may appear at the end of the
deceleration.
If the variable deceleration lasts long
enough to cause hypoxia, there may be a more gradual rise back to the
baseline and some "overshoot." Overshoot means the heart rate goes
higher than the baseline for a while, to compensate for the mild degree
of hypoxia and acidosis that has occurred during that deceleration. If
you exercise vigorously for a minute, your muscle tissues will acquire
some degree of oxygen debt and a mild degree of local acidosis. When you
sit down and rest, your heart rate will be higher than before you
started exercising, but will return to normal as you resupply your
muscles with oxygen and remove the local waste products. The fetus
responds in a similar fashion.
Variable decelerations, unlike late
decelerations, are not caused by hypoxia, although if severe enough,
frequent enough and persistent enough, can ultimately lead to some
degree of fetal acidosis.
The interventions to effectively treat
variable decelerations may include:
-
Changing maternal position to improve
uterine blood flow
-
IV hydration to increase maternal blood
volume, presumably leading to increased uterine blood flow
-
Administering oxygen to the mother to
try to get some additional oxygen through to the fetus. Of the three
standard treatments, oxygen administration is the least useful, since
the maternal hemoglobin oxygen saturation is likely already 99%. The
effect of breathing additional oxygen will probably have minimal
effect on the oxygen saturation.
-
Amnioinfusion to improve
oligohydramnios
-
Decreasing or discontinuing oxytocin
infusion to slow down or stop contractions that are provoking the
decelerations.
-
Tocolytic drugs to slow down or stop
contractions that are provoking the decelerations.
-
Digital elevation of the fetal head out
of the maternal pelvis to ease pressure on the umbilical cord.
Occasional mild or moderate variable
decelerations are common and not considered threatening. They are seen
in the majority of laboring patients at some time or other. They are
more common in the second stage of labor.
Mild variable decelerations do not dip
below 70 BPM and last less than 30 seconds.
Severe variable decelerations dip below
60 BPM for at least 60 seconds ("60 x 60"). If persistent and not
correctable by simple means, they can be threatening to fetal
well-being. Like persistent, non-remediable late decelerations, fetuses
demonstrating persistent, non-remediable severe variable decelerations
should be delivered promptly, preferably vaginally, but by cesarean
section if necessary.
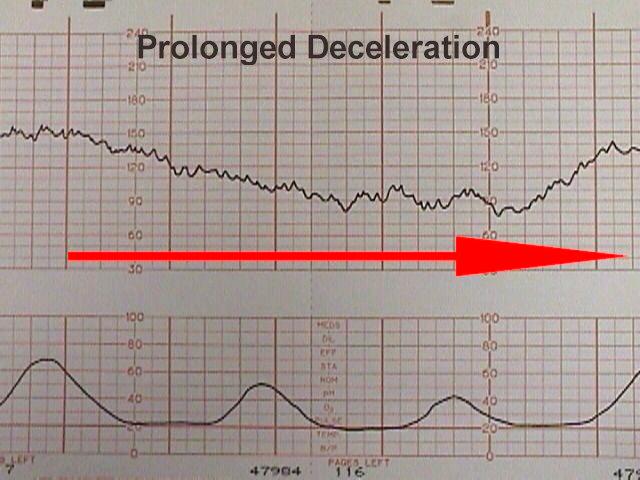
Prolonged
decelerations
Prolonged decelerations last more than 60 seconds and occur in
isolation. Causes include maternal supine hypotension, epidural
anesthesia, paracervical block, tetanic contractions, and umbilical cord
prolapse.
Some of these are largely
self-correcting, such as the deceleration following paracervical block,
while others (maternal supine hypotension) respond to simple measures
such as repositioning.
Other causes (such as umbilical cord
prolapse) require prompt intervention to avoid or reduce the risk of
fetal injury.
|