|
Clinical Warts
Condyloma acuminata, (venereal warts) are caused by a virus known as
"Human Papilloma Virus"
(HPV).
There are two categories of warts, clinical and subclinical. Clinical
warts appear as tiny, cauliflower-like, raised lesions around the
opening of the vagina or inside the vagina. These lesions appear
flesh-colored or white, are not tender and have a firm to hard
consistency. If they are on the outside of the vagina or vulva, they are
generally symptomatic, causing itching, burning, and an uncomfortable
sensation during intercourse. If they are inside the vagina, they
generally cause no symptoms.
Subclinical Warts
The second category, subclinical warts, are
invisible to the naked eye, are flat and colorless. They usually do not
cause symptoms, although they may cause similar symptoms to the raised
warts. These subclinical warts can be visualized if the skin is first
soaked for 2-3 minutes with vinegar (3-4% acetic acid) and then viewed
under magnification (4-10X) using a green or blue (red-free) light
source.
Venereal warts are not dangerous and have virtually no malignant
potential. Clinical warts may be a nuisance and so are usually
treated. Subclinical warts are usually not treated since they are
not a nuisance (most people with subclinical warts are unaware of their
presence).
Treatment
Treatment consists of removal of the wart. This can
be accomplished in any number of ways, some more painful than others:
-
Apply a small amount of bichloracetic acid (80-90%) directly to
the wart, taking care to avoid spreading the acid onto the normal
surrounding skin. For larger lesions, use a cotton-tipped applicator
dipped in the acid. For smaller lesions, use the "stick" end of the
cotton-tipped applicator. Apply enough acid (very tiny amounts) to
cause the lesion to turn white, but not so much that it runs down onto
the normal surrounding skin. No anesthetic is necessary. The patient
may feel nothing, some slight tingling, or a minor stinging. After a
minute or two, rinse the skin with warm water to dilute any remaining
acid and prevent it from coming into contact with the surrounding
skin.
-
Cryosurgery can effectively remove warts. Freezing the wart with
any convenient tool (liquid nitrogen, cryosurgical probe, etc.) can be
done without anesthetic and results in sloughing of the wart in a week
or two. Be careful not to freeze normal skin. Two freeze-thaw cycles
usually work better than a single freeze-thaw cycle.
-
Podophyllum resin can be applied directly to the wart, followed by
washing off the residual podophyllin in 3-6 hours. This effective
approach runs the risk of podophyllin toxicity. This is a minor issue
if the wart is very small and you use tiny quantities of podophyllin.
If you use large amounts, or apply it inside the vagina, toxicity is a
real issue.
Don't apply large amounts of podophyllin and don't apply
any inside the vagina or on the cervix.
-
Under anesthetic, warts can be surgically removed, burned, or
electrocuted, but such methods are usually unnecessary for the typical
small wart(s).
-
If untreated, many warts will gradually resolve and disappear
spontaneously, but this may require many months or years.
Remember that in treating the warts, you are actually destroying the
patient's skin which has responded in a strange and annoying way to the
presence of the HPV. You are not getting rid of the HPV itself.
Persistence of Virus
HPV is a sexually-transmitted virus which usually causes no symptoms
but occasionally causes warts. The virus spreads throughout the skin of
the vulva and vagina (as well as the inner thighs and lower abdomen),
where it disappears into the skin cells and usually remains dormant
forever.
Like many other viruses, if the patient's immune system allows the
virus to grow, it can reappear and cause warts. This virus is extremely
common, infecting as many as 1/3 of the adult, sexually-active
population. There is no known way to eliminate the virus from all skin
cells.
Transmission
Patients with HPV are contagious to others, but there is no
effective way to prevent its spread. Some physicians recommend condoms,
but because the virus is found in areas of the skin beyond the condom,
this is not likely to be effective. Some physicians recommend aggressive
treatment of all warts, in the belief that active warts are more
contagious than inactive virus within the skin. This theory has not, so
far, been proven to be true.
Dysplasia
While warts are not considered dangerous, HPV infection is
associated with another skin change known as "dysplasia." Dysplasia
means that the skin (mainly of the cervix) begins growing faster than it
should. There are different degrees of dysplasia: mild, moderate and
severe. None of these is malignant, but it is true that the next step
beyond severe dysplasia is cancer of the cervix.
About 1/3 of all adult, sexually-active women have been infected with
HPV, but probably less than 10% will ever develop dysplasia. Most (90%)
of those with dysplasia will have mild dysplasia which will either
regress back to normal or at least will never progress to a more
advanced stage.
Relation to Cancer
Most women (About 90%) with mild dysplasia of the cervix will never
develop a more advanced problem, and often the abnormality regresses
back to normal.
Most women with moderate to severe dysplasia of the cervix, if
left untreated, will ultimately develop cancer of the cervix. If
treated, most of these abnormalities will revert to normal, making this
form of cervical cancer largely preventable.
Cervical dysplasia is usually a slowly-changing clinical problem.
There is indirect evidence to suggest that on average, it takes about 10
years to advance from normal, through the various stages of dysplasia,
and into cancer of the cervix. Of course, any individual may not follow
these rules. In providing medical care to women with cervical dysplasia,
good follow-up is important, but urgent medical evacuation is usually
not indicated for less threatening categories of dysplasia.
Evaluation
In any patient with venereal warts (condyloma), you should look for
possible dysplasia of the cervix. This is best done with colposcopy, but
a simple Pap smear can be very effective. Because HPV causes warts and
is also associated with dysplasia, more frequent Pap smears (every 6
months) is a wise precaution, at least initially.
If dysplasia is found, gynecologic consultation will be necessary,
although this may be safely postponed for weeks or months if operational
requirements make consultation difficult. |
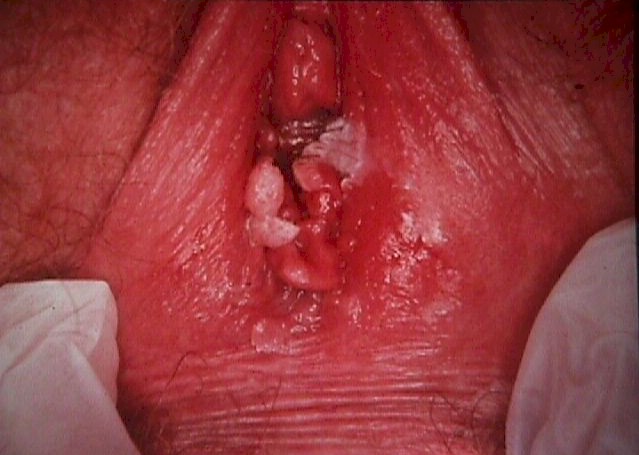
Condyloma at vaginal opening

Apparently normal cervix

After application of acetic acid

Vaginal wall condyloma
|