|
Lesson 8: Perioperative Patient Care
SECTION III. RECOVERY ROOM CARE
a. The recovery room is defined as a specific nursing unit, which accommodates patients who have undergone major or minor surgery. Following the operation, the patient is carefully moved from the operating table to a wheeled stretcher or bed and transferred to the recovery room. The patient usually remains in the recovery room until he begins to respond to stimuli. General nursing goals of care for a patient in the recovery room are:
(1) To support the patient through his state of dependence to independence. Surgery traumatizes the body, decreasing its energy and resistance. Anesthesia impairs the patient's ability to respond to environmental stimuli and to help himself. An artificial airway is usually maintained in place until reflexes for gagging and swallowing return. When the reflexes return, the patient usually spits out the airway. Position the unconscious patient with his head to the side and slightly down. This position keeps the tongue forward, preventing it from blocking the throat and allows mucus or vomitus to drain out of the mouth rather than down the respiratory tree. Do not place a pillow under the head during the immediate postanesthetic stage. Patients who have had spinal anesthetics usually lie flat for 8 to 12 hours. The return of reflexes indicates that anesthesia is ending. Call the patient by name in a normal tone of voice and tell him repeatedly that the surgery is over and that he is in the recovery room.
(2) To relieve the patient's discomfort. Pain is usually greatest for 12 to 36 hours after surgery, decreasing on the second and third post-op day. Analgesics are usually administered every 4 hours the first day. Tension increases pain perception and responses, thus analgesics are most effective if given before the patient's pain becomes severe. Analgesics may be administered in patient controlled infusions.
(3) Early detection of complications. Most people recover from surgery without incident. Complications or problems are relatively rare, but the recovery room nurse must be aware of the possibility and clinical signs of complications.
(4) Prevention of complications. Complications that should be prevented in the recovery room are respiratory distress and hypovolemic shock.
b. The difference between the recovery room and surgical intensive care are:
(1) The recovery room staff supports patients for a few hours until they have recovered from anesthesia.
(2) The surgical intensive care staff supports patients for a prolonged stay, which may last 24 hours or longer.
|
|
a. Respiratory distress is the most common recovery room emergency. It may be caused by laryngospasm, aspiration of vomitus, or depressed respirations resulting from medications.
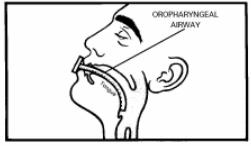
(1) A laryngospasm is a sudden, violent contraction of the vocal cords; a complication, which may happen after the patientís endotracheal tube, is removed. During the surgical procedure with general anesthesia, an endotracheal tube is inserted to maintain patent air passages. The endotracheal tube may be connected to a mechanical ventilator. Upon completion of the operation, the endotracheal tube is removed by the anesthesiologist or anesthetist and replaced by an oropharyngeal airway (figure 8-4).
(2) Swallowing and cough reflexes are diminished by the effects of anesthesia and secretions are retained. To prevent aspiration, vomitus or secretions should be removed promptly by suction.
(3) Ineffective airway clearance may be related to the effects of anesthesia and drugs that were administered before and during surgery. If possible, an unconscious or semiconscious patient should be placed in a position that allows fluids to drain from the mouth.
b. After removal of the endotracheal tube by the anesthesiologist or anesthetist, an oropharyngeal airway is inserted to prevent the tongue from obstructing the passage of air during recovery from anesthesia. The airway is left in place until the patient is conscious.
8-12. PREVENTION OF RESPIRATORY DISTRESS
a. Monitor respiratory status as frequently as prescribed. Respiratory function is assessed by monitoring the patient's respiratory rate, rhythm, and depth, and by observing skin color. The following observations indicate ineffective ventilation:
(1) Restlessness and apprehension.
(2) Unequal chest expansion with use of accessory muscles.
(3) Shallow, noisy respirations.
(4) Cyanosis.
(5) Rapid pulse rate.
b. Report labored respirations to supervisor.
c. Report shallow, rapid respirations to the supervisor.
d. Maintain a patent airway with or without an oropharyngeal tube.
e. Maintain the patient in a position to facilitate lung expansion, usually in Fowler's position.
f. Administer oxygen as ordered.
g. Prevent aspiration of vomitus.
(1) Maintain the position of the patient's head to one side and place an emesis basin under the cheek, extending from just below the eye to the lower edge of the bottom lip.
(2) Wipe vomitus or secretions from the nose or mouth in order to avoid possible aspiration of these fluids into the lungs.
h. Suction the patient either through the nose or mouth as ordered.
a. When there is an alteration in circulatory control or a loss of circulating fluid, the body's reaction is shock. The most common type of shock seen in the postoperative patient is hypovolemic shock, which occurs with a decrease in blood volume. Common signs and symptoms are hypotension; cold, clammy skin; a weak, thready, and rapid pulse; deep, rapid respirations; decreased urine output; thirst; apprehension; and restlessness.
b. Hemorrhage, which is an excessive blood loss, may lead to hypovolemic shock. Postoperative hemorrhage may occur from a slipped suture, a dislodged clot in a wound, or stress on the operative site. It also may result from the pathological disorder for which the patient is being treated, or be caused by certain medications.
c. The primary nursing care goal is to maintain tissue perfusion by eliminating the cause of the shock.
(1) The blood loss from surgery that causes hypovolemic shock may be internal or external.
(2) The loss of fluid or blood volume does not have to be rapid or copious amounts to cause shock.
d. The primary purposes of care for the patient having a hemorrhage include stopping the bleeding and replacing blood volume.
8-14. DETECTION OF PENDING HYPOVOLEMIC SHOCK
a. Inspect the surgical dressing frequently and report any bleeding to the supervisor. Also inspect the bedding beneath the patient because blood may drain down the sides of a large dressing and pool under the patient. When reporting bleeding, note the color of the blood. Bright red blood signifies fresh bleeding. Dark, brownish blood indicates that the bleeding is not fresh.
b. Outline the perimeter of the blood stain on the original dressing. Reinforce the original dressing, and make note on the dressing of the date and time the outline was made.
c. Document your observations and the action taken in the nurse's notes.
d. Monitor the patient's vital signs as ordered and report any of the following abnormalities to the supervisor.
(1) A drop in blood pressure (systolic reading below 90 in an adult indicates possible shock; systolic below 80 means actual shock).
(2) A rapid, weak pulse.
(3) Restlessness.
(4) Cool, moist, pale skin.
(5) Tingling of the lips.
(6) Pallor or blueness (cyanosis) of the lips, nailbeds, or conjunctiva (a dark-skinned persons lips will appear a dusky gray).
e. Administer narcotics only after checking doctor's orders and consulting with supervisor. If shock is imminent, it may be precipitated by administration of narcotics.
f. Administer fluids to replace volume in accordance with the doctor's orders. The doctor may order that blood volume be replaced by intravenous (IV) fluids, plasma expanders, or whole blood products.
|
8-15. GENERAL NURSING CARE OF A PATIENT IN THE RECOVERY ROOM
a. When the patient is moved to the recovery room, every effort should be made to avoid unnecessary strain, exposure, or possible injury. The anesthesiologist or anesthetist goes to the recovery room with the patient, reports his condition, leaves postoperative orders and any special instructions, and monitors his condition until that responsibility is transferred to the recovery room nurses. The recovery room nurse should check the doctor's orders and carry them out immediately.
b. Patients are concentrated in a limited area to make it possible for one nurse to give close attention to two or three patients at the same time. Each patient unit has a recovery bed equipped with side rails, poles for IV medications, and a chart rack. The bed is easily moved and adjusted. Each unit has outlets for piped-in oxygen, suction, and blood pressure apparatus. The following are nursing implications for the general care of a patient in the recovery room:
(1) Maintain proper functioning of drains, tubes, and intravenous infusions. Prevent kinking or clogging that interferes with adequate flow of drainage through catheters and drainage tubes.
(2) Monitor intake and output precisely, to include all Intravenous fluids and blood products, urine, vomitus, nasogastric tube drainage, and wound drainage.
(3) Observe and document the patient's level of consciousness. The return of central nervous system function is assessed through response to stimuli and orientation. Levels of consciousness return in reverse order: unconscious, responds to touch and sound, drowsy, awake but not oriented, and awake and oriented. Specific criteria is usually used for categorizing the recovery room patient.
(a) Comatose -- unconscious; unresponsive to stimuli.
(b) Stupor -- lethargic and unresponsive; unaware of surroundings.
(c) Drowsy -- half asleep, sluggish; responds to touch and sounds.
(d) Alert -- able to give appropriate response to stimuli.
(4) Implement safety measures to protect the patient. Keep the side rails raised at all times. Assure that the patient is positioned so that he is not tangled in or laying on IV or drainage tubes. Do not use a head pillow while the patient is unconscious, or for eight hours if the patient had spinal anesthesia. Turn the patient's head to one side when he is in the supine position so that secretions can drain from the mouth and the tongue will not fall into the throat to block the air passage. When the patient is alert, show him how to use the call bell and place it where it is readily available.
(5) If the patient had a spinal anesthetic, observe and report any feeling or spontaneous movement. Movement usually returns before feeling. Movement returns in the patient's toes first, and moves upward. As the anesthesia wears off, the patient will begin to have sensation often described as "pins and needles." Spinal anesthesia wears off slowly. Keep the patient in a supine position for six to eight hours to prevent spinal headache. Turn the patient from side to side and prop up with pillows for a few minutes to relieve pressure on the back, but only if permitted by the doctor.
(6) Prevent nosocomial infections. Wash your hands before and after working with each patient. Maintain aseptic technique for incisional wounds. Turn the patient frequently to prevent respiratory infections. When the patient is alert, encourage and assist him to cough and take deep breaths several times each hour.
(7) If possible, engage the patient in a conversation to observe his level of orientation. Take into consideration each patient's normal responses due to various physical factors.
(8) Provide emotional support to the patient and his family. When the patient is alert, tell him that he is in the recovery room and that you are always nearby to help him. Reinforce any information that may have been provided by the surgeon. To decrease anxiety and increase lung expansion, encourage conversation with the patient. Use this opportunity to patient teach by explaining what you are about to do in brief, simple sentences. If family members are permitted in the recovery room, stay with them as they visit. They may be frightened of the environment and by their loved one's appearance.
(9) When the patient's physical status and level of consciousness are stable, the surgeon clears the patient for transfer to his room. Call the nursing unit and give a verbal report to include the following.
(a) Patient's name
(b) Type of surgery.
(c) Mental alertness.
(d) Care given in the recovery room.
(e) Vital signs, at what time they were taken, and any symptoms of complications.
(f) Presence, type and functional status of intravenous fluids, and any suction or drainage systems.
(g) Whether or not the patient has voided, if a catheter is not in place.
(h) Any medications given in the recovery room.
(10) Document all necessary information in the nurse's notes and transfer the patient to the unit in accordance with local standing operating procedures (SOP).