|
Lesson 8: Perioperative Patient Care
SECTION I. PREOPERATIVE PATIENT CARE
a. Patients are admitted to the health care facility for surgical intervention from a variety of situations and in various physical conditions. The nurse is responsible for completion of preoperative forms, implementing doctor's orders for preoperative care, and documentation of all nursing measures.
b. The following nursing implications are related to preparing a patient for surgery.
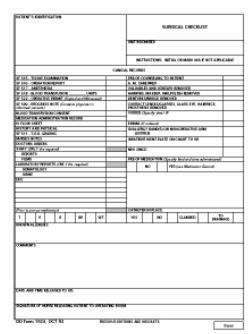
(1) Prepare the patient's chart using DD Form 1924, Surgical Check List (figure 8-1). DD Form 1924 contains the following information:
(a) Space for the patient's identification.
(b) A checklist for pertinent clinical records.
(c) A space for recording the most current set of vital signs taken prior to preoperative medications.
(d) A space to indicate allergies.
(e) A space to document all preoperative nursing measures.
(f) A space to document any comment that indicates something very special about this particular patient (for example, removal of prosthesis, patient hard of hearing).
(g) A space for signature of release by the registered nurse when all actions are completed.
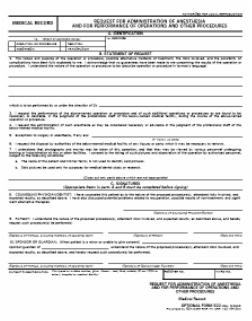
(2) Ensure completion of SF 522, Request for Administration of Anesthesia and for Performance of Operations and Other Procedures (figure 8-2).
(a) SF 522 is a legal document, which satisfies requirement of informed consent. A surgical consent form must be signed by the patient before surgery can be performed.
(b) It must be signed by the physician and anesthesiologist to indicate that all risks of surgery and anesthesia have been fully explained to the patient.
|
(c) The patient must sign in the presence of a witness, to consent for the surgical procedure. The witness is attesting to the patient's signature, not to the patient's understanding of the surgical risks. If the adult patient is unconscious, semiconscious, or is not mentally competent, the consent form may be signed by a family member or legal guardian.
(d) If the patient is a minor (usually under the age of 18), the consent form is signed by a parent or legal guardian. A minor who lives away from home and is self-supporting is considered emancipated and he may sign.
(e) Legal age is established on a state-by-state basis. Be familiar with the age of consent for the state in which the health care facility is located and with legal implications when a person other than the patient signs the consent form.
(f) Legal consent forms must be signed prior to administration of preoperative medication or any type of mind-altering medication or the document is not legally binding.
(g) SF 522 must be timed and dated.
(3) Implement doctor's orders for preoperative care.
(a) If ordered, administer an enema. The enema cleanses the colon of fecal material, which reduces the possibility of wound contamination during surgery.
(b) If ordered, assure that the operative site skin prep (shave) is done. An operating room technician or other designated person will clean and shave a wide area surrounding the planned site for the incision. (This may be done in the operating room immediately before surgery). The skin prep frees the skin of hair and microorganisms as much as possible, thus decreasing the possibility of them entering the wound via the skin surface during surgery.
(c) The doctor will give specific directions concerning withholding food and fluid before surgery. Assure that the order is followed. Typically, the patient may eat solid food until supper, but can have nothing by mouth (NPO) beginning at midnight before surgery. Place the NPO sign outside the patient's room. Instruct the patient of the importance and the reason for being NPO. Remove the water pitcher and the drinking glass. Clearly mark the diet roster.
(d) If ordered, administer a sedative. The evening before surgery a hypnotic drug, such as flurazepam hydrochloride (Dalmane®) may be given so that the patient can get a good night's sleep.
8-4. PREPARING THE PATIENT FOR SURGERY
a. Preoperative preparation may extend over a period of several days. The patient may undergo tests, radiographic studies, and laboratory procedures. A medical history is taken and a physical examination performed before surgery. Patients scheduled for elective surgery may have laboratory tests such as urinalysis, complete blood count, hemoglobin, and hematocrit done as an outpatient. The nurse plays an important role in explaining the necessity for preoperative tests and in carrying out preparations for these tests. The immediate preparation for surgery usually starts the evening before surgery. Nursing implications related to the preoperative preparation of a patient are:
(1) Assist the patient with personal hygiene and related preoperative care.
(a) The evening before surgery, the patient should take a bath or shower, and shampoo hair to remove excess body dirt and oils. The warm water will also help to relax the patient. Sometimes plain soap and water are used for cleansing the skin, but a topical antiseptic may be used.
(b) Remove all makeup and nail polish. Numerous areas (face, lips, oral mucosa, and nail beds) must be observed for evidence of cyanosis. Makeup and nail polish hide true coloration.
(c) Jewelry and other valuables should be removed for safe keeping. The patient may wear a wedding band to surgery, but it must be secured with tape and gauze wrapping. Do not wrap tightly; circulation may be impaired. Do not leave valuables in the bedside stand or store in the narcotics container. If possible, send these items home with a relative until the patient has need of them. Chart what has been done with the valuables.
|
(2) Provide information concerning surgery.
(a) The patient is told about the risks and benefits of surgery, the likely outcome if surgery is not performed, and alternative methods of treatment by his doctor. However, the nurse can help the patient cope with the upcoming surgery by taking the time to listen to the patient and others who are concerned about his well being, and answering other questions.
(b) Explain each preoperative nursing measure.
(c) Provide an opportunity for the patient to express his feelings. Ask about spiritual needs and whether he wishes to see a Chaplain.
(d) Provide family members with information concerning their role the morning of the surgery. Give them the surgical waiting room location, and the probable time that they can visit the patient after surgery. Explain the rationale for the patient's stay in the recovery room. Inform them of any machines or tubes that may be attached to the patient following surgery.
(3) Provide preoperative morning care.
(a) Awake the patient early enough to complete morning care. Give him a clean hospital gown and the necessary toiletries. The patient should have another shower or bath using a topical antiseptic, such as povidone-iodine. The skin cannot be made completely sterile, but the number of microorganisms on it can be substantially reduced. If the surgery is extensive, it may be several days before the patient has another shower or "real" bath.
(b) The patient should have complete mouth care before surgery. A clean mouth provides comfort for the patient and prevents aspiration of small food particles that may be left in the mouth. Instruct the patient not to chew gum.
(4) Remove prostheses. Assist the patient or provide privacy so that the patient can remove any prostheses. These includes artificial limbs, artificial eyes, contact lenses, eyeglasses, dentures, or other removable oral appliances. Place small items in a container and label them with the patient's name and room number. Dentures are usually left at the bedside.
(5) Record vital signs. Obtain and record the patient's temperature, pulse, respiration, and blood pressure before the preoperative medication is administered.
b. Allow the patient time to complete any last minute personal measures and visit with the family.
c. Recheck the accuracy of DD Form 1924, Surgical Check List.
d. If ordered, administer preoperative medications. Pre-op medications are usually ordered by the anesthesiologist, and administered about 30 to 60 minutes before the patient is taken to the operating room.
(1) The medications may be ordered given at a scheduled time or on call (the operating room will call and tell you when to give the medications).
(2) The medications may consist of one, two, or three drugs: a narcotic or sedative; a drug to decrease secretions in the mouth, nose, throat, and bronchi; and an antiemetic.
(3) Have the patient void before administering the medications.
(4) Explain to the patient the effects experienced following administration of the medications (drowsiness, extreme dry mouth).
(5) Instruct the patient to remain in bed. Raise the side rails on the bed and place the call bell within easy reach.
e. Assist the operating room technician. The patient is usually transported to the operating room on a wheeled litter, or gurney. The technician should cover the patient with a clean sheet or cotton blanket. Assist the technician to position the patient on the litter. See that the patient is comfortable, and that the restraint is fastened to prevent him from falling off the litter.
8-5. DOCUMENT NURSING MEASURES
a. All necessary information should be recorded on the chart before the patient leaves the nursing unit. Check the patient's identification band to be sure the right patient is being taken to surgery. Check the consent form to be sure that it is correctly signed and witnessed.
b. "Sign out" the patient in the nurse's notes. Include the date, the time, the event, and your observations on the status of the patient. "Sign off" DD Form 1924, Surgical Check List.