This is the Archived Desktop Edition.
You should be transferred to the Newest Edition for Desktop and Mobile within 2 seconds.
|
|
Lesson 1: Reproductive Anatomy and Physiology
Section I. THE FEMALE REPRODUCTIVE SYSTEM
1-4. EXTERNAL FEMALE GENITALIA
The external organs of the female reproductive system include the mons pubis, labia majora, labia minora, vestibule, perineum, and the Bartholin's glands. As a group, these structures that surround the openings of the urethra and vagina compose the vulva, from the Latin word meaning covering. See Figure 1-6.
a. Mons Pubis. This is the fatty rounded area overlying the symphysis pubis and covered with thick coarse hair.
b. Labia Majora. The labia majora run posteriorly from the mons pubis. They are the 2 elongated hair covered skin folds. They enclose and protect other external reproductive organs.
c. Labia Minora. The labia minora are 2 smaller folds enclosed by the labia majora. They protect the opening of the vagina and urethra.
d. Vestibule. The vestibule consists of the clitoris, urethral meatus, and the vaginal introitus.
(1) The clitoris is a short erectile organ at the top of the vaginal vestibule whose function is sexual excitation.
(2) The urethral meatus is the mouth or opening of the urethra. The urethra is a small tubular structure that drains urine from the bladder.
(3) The vaginal introitus is the vaginal entrance.
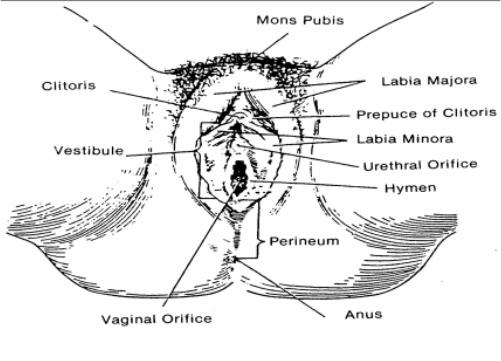
Figure 1-6. External female
genitalia.
e. Perineum. This is the skin covered muscular area between the vaginal opening (introitus) and the anus. It aids in constricting the urinary, vaginal, and anal opening. It also helps support the pelvic contents.
f. Bartholin's Glands (Vulvovaginal or Vestibular Glands). The Bartholin's glands lie on either side of the vaginal opening. They produce a mucoid substance, which provides lubrication for intercourse.
The blood supply is derived from the uterine and ovarian arteries that extend from the internal iliac arteries and the aorta. The increased demands of pregnancy necessitate a rich supply of blood to the uterus. New, larger blood vessels develop to accommodate the need of the growing uterus. The venous circulation is accomplished via the internal iliac and common iliac vein.
1-6. FACTS ABOUT THE MENSTRUAL CYCLE
Menstruation is the periodic discharge of blood, mucus, and epithelial cells from the uterus. It usually occurs at monthly intervals throughout the reproductive period, except during pregnancy and lactation, when it is usually suppressed.
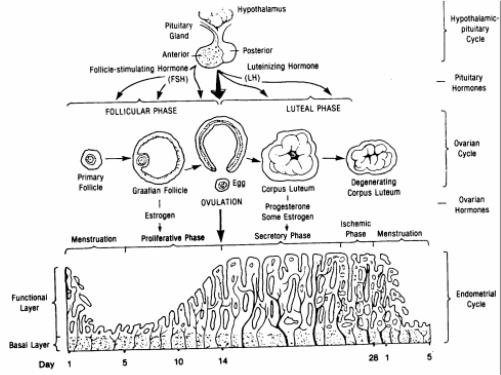
a. The menstrual cycle is controlled by the cyclic activity of follicle stimulating hormone (FSH) and LH from the anterior pituitary and progesterone and estrogen from the ovaries. In other words, FSH acts upon the ovary to stimulate the maturation of a follicle, and during this development, the follicular cells secrete increasing amounts of estrogen (see figure 1-7).
b. Hormonal interaction of the female cycle are as follows:
(1) Days 1-5. This is known as the menses phase. A lack of signal from a fertilized egg influences the drop in estrogen and progesterone production. A drop in progesterone results in the sloughing off of the thick endometrial lining which is the menstrual flow. This occurs for 3 to 5 days.
(2) Days 6-14. This is known as the proliferative phase. A drop in progesterone and estrogen stimulates the release of FSH from the anterior pituitary. FSH stimulates the maturation of an ovum with graafian follicle. Near the end of this phase, the release of LH increases causing a sudden burst like release of the ovum, which is known as ovulation.
(3) Days 15-28. This is known as the secretory phase. High levels of LH cause the empty graafian follicle to develop into the corpus luteum. The corpus luteum releases progesterone, which increases the endometrial blood supply. Endometrial arrival of the fertilized egg. If the egg is fertilized, the embryo produces human chorionic gonadotropin (HCG). Thehuman chorionic gonadotropin signals the corpus luteum to continue to supply progesterone to maintain the uterine lining. Continuous levels of progesterone prevent the release of FSH and ovulation ceases.
c. Additional Information.
(1) The length of the menstrual cycle is highly variable. It may be as short as 21 days or as long as 39 days.
(2) Only one interval is fairly constant in all females, the time from ovulation to the beginning of menses, which is almost always 14-15 days.
(3) The menstrual cycle usually ends when or before a woman reaches her fifties. This is known as menopause.
Ovulation is the release of an egg cell from a mature ovarian follicle (see figure 1-5 for ovulation). Ovulation is stimulated by hormones from the anterior pituitary gland, which apparently causes the mature follicle to swell rapidly and eventually rupture. When this happens, the follicular fluid, accompanied by the egg cell, oozes outward from the surface of the ovary and enters the peritoneal cavity. After it is expelled from the ovary, the egg cell and one or two layers of follicular cells surrounding it are usually propelled to the opening of a nearby uterine tube. If the cell is not fertilized by union of a sperm cell within a relatively short time, it will degenerate.
As mentioned in paragraph 1-6c(3), menopause is the cessation of menstruation. This usually occurs in women between the ages of 45 and 50. Some women may reach menopause before the age of 45 and some after the age of 50. In common use, menopause generally means cessation of regular menstruation. Ovulation may occur sporadically or may cease abruptly. Periods may end suddenly, may become scanty or irregular, or may be intermittently heavy before ceasing altogether. Markedly diminished ovarian activity, that is, significantly decreased estrogen production and cessation of ovulation, causes menopause.
The Brookside Associates Medical Education Division is dedicated to the development and dissemination of medical information that may be useful to medical professionals and those in training to become medical professionals. This website is privately-held and not connected to any governmental agency. The views expressed here are those of the authors, and unless otherwise noted, do not necessarily reflect the views of the Brookside Associates, Ltd., any governmental or private organizations. All writings, discussions, and publications on this website are unclassified.
© 2007 Medical Education Division, Brookside Associates, Ltd. All rights reserved