This is the Archived Desktop Edition.
You should be transferred to the Newest Edition for Desktop and Mobile within 2 seconds.
|
|
Lesson 1: Reproductive Anatomy and Physiology
Section II. THE MALE REPRODUCTIVE SYSTEM
a. The male reproductive tract consists of external genitals and internal organs. These organs are located in the pelvic cavity (see figure 1-8). The male's reproductive system begins to develop in response to testosterone during early fetal life. Essentially no testosterone is produced during childhood. Resumption of testosterone production at the onset of puberty stimulates growth and maturation of the male's reproductive structures and secondary sex characteristics. Testosterone is the male sex hormone secreted by the interstitial cells of the testes.
b. The primary function of the male's reproduction system is to produce male sex cells, which are called sperm cells. The primary organs of the male's reproduction system are the two testes in which the sperm cells are formed. The other structures are the duct system and the accessory glandular structure.
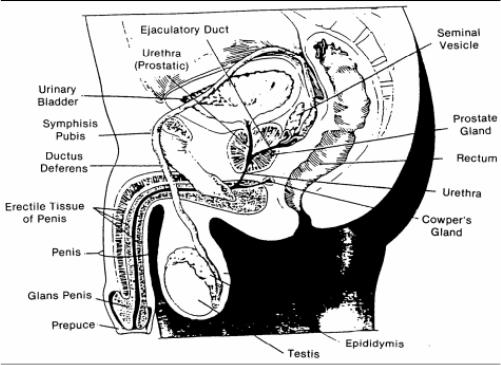
Figure 1-8. The male reproductive organs.
1-10. MALE REPRODUCTIVE ORGANS
a. Testes
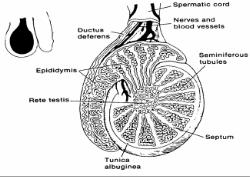
(Two). The testes are two almond-shaped glands whose functions are for the production of sperm and testosterone. The testes are suspended in the scrotal sac outside the abdominopelvic cavity. It is believed that the testes lie outside the body cavity because they are very sensitive to heat and the higher temperature within the body is unfavorable to the production of sperm. Each testis is enclosed by a tough, white fibrous capsule called the tunica albuginea. Extension of the capsule divides it into a large number of lobes. Each lobe contains four tightly coiled seminiferous tubules (this is the location of actual sperm production). The seminiferous tubules empty sperm into the testicular network where they travel to the epididymis. The epididymis is located outside of the testis (see figures 1-8 and 1-9).b. Duct System. The duct system is the passageway for the sperm to exit the body. It contains the epididymis and the vas deferens. (1) Epididymis. The epididymis is a coiled tube about 20 inches long. It caps the superior part of the testis and runs down its posterior side. It forms the first part of the duct system and provides a temporary storage site for immature sperm.
When the male is sexually stimulated, the walls of the epididymis contract to expel sperm into the next part of the duct system. (2) Vas deferens (ductus deferens). The sperm continue their journey through the vas deferens. The vas deferens runs upwards from the epididymis through the inguinal canal into the pelvic cavity and arches over the bladder (see figure 1-8). It is enclosed with blood vessels and nerves in a connective tissue sheath, which is called a spermatic cord. The vas deferens empties into the ejaculatory duct that carries the sperm through the process to empty into the urethra.
c. Accessory Glandular Structure. The accessory glandular structure includes the seminal vesicles, prostate gland, Cowper's glands, and the penis.
(1) Seminal vesicles. The two seminal vesicles are pouches that store sperm. Sixty percent of fluid volume of semen (seminal fluid) is produced there. The secretion is rich in sugar (fructose), which nourishes and activates the sperm passing through the tract.
(2) Prostate gland. The prostate gland is a single gland about the size and shape of a chestnut. It encircles the upper area of the urethra just below the bladder. It secretes a milky alkaline fluid, which has the role in protecting the sperm against acid conditions of the vagina.
(3) Cowper's glands. The cowper's glands are tiny pea-sized glands inferior to the prostate. They form a thick, clear mucus, which drains into the urethra. The secretion is believed to serve primarily as a lubricant during sexual intercourse.
(4) Penis. The penis is a cylinder-shaped organ located externally on the mons pubis, immediately above the scrotum. It is made of erectile tissue with cavern-like spaces in it. At the time of sexual excitement, blood fills these spaces, changing the soft, limp penis to an enlarged, rigid, erect organ. The smooth cap of the penis is called the glans penis and is covered by a fold of loose skin that forms the headlock foreskin. Surgical removal of this foreskin, called circumcision, is frequently performed. The penis also serves as part of the urinary tract in the male.
1-11. SPERMATOGENESIS (SPERM FORMATION)
a. Spermatogenesis begins during puberty and continues throughout life.
b. Millions of sperm are produced in a 24-hour period. This occurs in the seminiferous tubules (see figure 1-10).
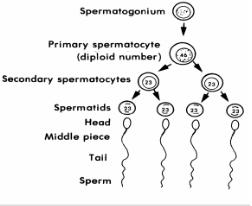
c. The process is begun by primitive stem cells, which are called spermatogonia and are found in the outer region of each tubules. Follicle stimulating hormone is secreted by the anterior pituitary beginning at puberty. Follicle stimulating hormone is influences division of spermatogonia into primary spermatocytes.
d. Each spermatocyte undergoes meiosis and produces four spermatids. All of the male's body cells contain the same 23 pairs of chromosomes. The spermatid contains one chromosome of each of the 23 pairs. The same chromosome configuration occurs in the ovum. When the sperm and egg unite, the normal number of chromosomes is reestablished--46 chromosomes or 23 pairs.
e. The mature sperm contains three regions: the head, which contains deoxyribonucleic acid (DNA), the midpiece, and the tail (see figure 1-11).
f. The acrosome is anterior to the head of the mature sperm. It contains special enzymes, which help the sperm to penetrate the egg.
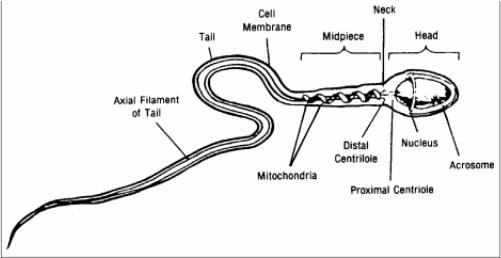
Figure 1-11. Structure of the sperm.
1-12. PROCESS OF TESTOSTERONE PRODUCTION
The interstitial cells, which lie between the seminiferous tubules, produce testosterone. These cells are activated during puberty by two hormones, FSH and LH, which is called interstitial cell stimulating hormone (ICSH). A rise in testosterone production in the young male stimulates his reproductive organs to develop to their adult size and causes secondary sex characteristics to appear. These characteristics are:
a. Deepening of the voice due to enlargement of the larynx.
b. Increased hair growth especially on the face, axillary, and pubic regions.
c. Enlargement of skeletal muscles.
d. Increase in skeletal size.
The Brookside Associates Medical Education Division is dedicated to the development and dissemination of medical information that may be useful to medical professionals and those in training to become medical professionals. This website is privately-held and not connected to any governmental agency. The views expressed here are those of the authors, and unless otherwise noted, do not necessarily reflect the views of the Brookside Associates, Ltd., any governmental or private organizations. All writings, discussions, and publications on this website are unclassified.
© 2007 Medical Education Division, Brookside Associates, Ltd. All rights reserved