|
First trimester scanning is useful to identify abnormalities in the early
development of a pregnancy, including miscarriage and ectopic pregnancy, and
provides the most accurate dating of a pregnancy.
Technique
First trimester scanning can be performed using either an abdominal approach or
a vaginal approach. Abdominal scanning is performed with a full maternal
bladder, provides a wider field of view, and provides the greatest depth of
view. Vaginal scanning is best performed with the bladder empty, gives a much
greater resolution with greater crispness of fine detail. In circumstances where
both approaches are readily available, the greater detail provided by
transvaginal scans usually outweighs other considerations, and is preferred.
The patient is scanned in the normal examination position (dorsal lithotomy)
with her feet secure in stirrups and her perineum even with the end of the
examination table. Place a small amount of ultrasonic
coupling gel on the tip of
the transvaginal transducer. Then cover the transducer with a condom. After
lubricating the vaginal opening, gently insert the transducer into the vagina.
Visualize the longitudinal plane of the uterus (sagital section) and evaluate
its' size. It can be measured from the cervix to the fundus, AP diameter, and
width. Normal uterine volume is less than 100 cc (nulliparous patients) and less
than 125 cc (multiparous patients). Identify (if present), the gestational sac,
yolk sac, fetus (or fetuses), presence or absence of fetal movement and fetal
heart beat.
After the uterus is evaluated by sweeping up and down and side to side, the
ovaries are identified and evaluated. This is most easily accomplished by first
identifying the internal iliac vessels. The ovaries are usually located just
anterior to the iliac vessels.
Document important views and measurements on film or electronically. Then
document your findings in some written format.
|
1st Trimester Ultrasound Scan |
Gestational Sac
The gestational sac is the earliest sonographic finding in pregnancy.
The gestational sac appears as an echogenic (bright echoes) ring surrounding a
sonolucent (clear) center. The gestational sac does not correspond to specific
anatomic structures, but is an ultrasonic finding characteristic of early
pregnancy. Ectopic pregnancies can also have a gestational sac identified with
ultrasound, even though the pregnancy is not within the endometrial
cavity.
The gestational sac first appears at about 4 weeks gestational age, and grows
at a rate of about 1 mm a day through the 9th week of pregnancy.
Your ability to identify an early gestational sac will depend on many
factors, including the capabilities of the ultrasound equipment, your approach
(vaginal or abdominal), your experience, the orientation of the uterus
(generally it is easier to see if the uterus is anteflexed or retroflexed), and
the presence of such complicating factors as fibroid tumors of the uterus. While
a gestational sac is sometimes seen as early as during the 4th week of
gestation, it may not be seen until the end of the 5th week, when the serum HCG
levels have risen to 1000-1500 mIU.
Gestational sac size may be determined by measuring the largest diameter, or
the mean of three diameters. These differences rarely effect gestational age
dating by more than a day or two.
|

1st Trimester Ultrasound Scan |
Yolk Sac
As the pregnancy advances, the next structure to become visible to
ultrasound is the yolk sac. This is a round, sonolucent structure with a bright
rim.
The yolk sac first appears during the fifth week of pregnancy and grows to be
no larger than 6 mm. Yolk sacs larger than 6 mm are usually indicative of an
abnormal pregnancy. Failure to identify (with transvaginal ultrasound) a yolk
sac when the gestational sac has grown to 12 mm is also usually indicative of a
failed pregnancy.
Yolk sacs that are moving within the gestational sac ("floating"),
contain echogenic material (rather than sonolucent), or are gross misshapen are
ominous findings for the pregnancy.
Fetal Heart Beat
Using endovaginal scanning, fetal cardiac activity is often seen even before a
fetal cell mass can be identified. The fetal cardiac muscle begins its' rhythmic
contractions, and that rhythmic motion can be seen along the edge of the yolk
sac. Initially, the fetal cardiac motion has a slower rate (60-90 BPM), but
cardiac rate increases as the fetus develops further. Thus, for these early
pregnancies, the actual cardiac rate is less important that its presence or
absence.
Sometimes, with normal pregnancies, the fetal heartbeat is not visible until
a fetal pole of up to 4 mm in length is seen. Failure to identify fetal cardiac
activity in a fetus whose overall length is greater than 4 mm is an ominous
sign.
It can sometimes be difficult identifying a fetal heartbeat from the
background movement and maternal pulsations. You may find it useful in these
cases to scan with one hand while taking the maternal pulse with the other. This
makes it easier to identify sonographic movements that are dyssynchronous with
the maternal pulse.
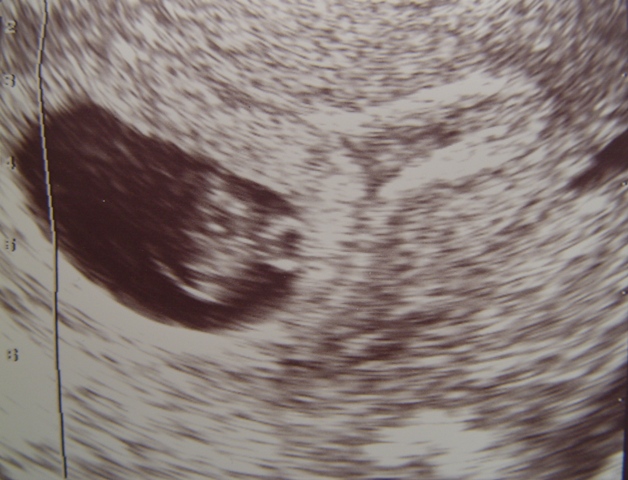
Fetal Pole
A mass of fetal cells, separate from the yolk sac, first becomes apparent on
transvaginal ultrasound just after the 6th week of gestation. This mass of cells
is known as the fetal pole. It is the fetus in its somite stage. Usually you can
identify rhythmic fetal cardiac movement within the fetal pole, although it may
need to grow several mm before this is apparent.
The fetal pole grows at a rate of about 1 mm a day, starting at the 6th week
of gestational age. Thus, a simple way to "date" an early pregnancy is
to add the length of the fetus (in mm) to 6 weeks. Using this method, a fetal
pole measuring 5 mm would have a gestational age of 6 weeks and 5 days.
Crown Rump Length
This term is borrowed from the early 20th century embryologists who found that
preserved specimens of early miscarriages assumed a "sitting in the
chair" posture in both formalin and alcohol. This posture made the
measurement of head-to-toe length impossible. Instead, they subsituted the
head-to-butt length (crown rump length) as a reproducible method of measuring
the fetus.
Early ultrasonographers used this term (CRL) because early fetuses also
adopted the sitting in the chair posture in early pregnancy. Today, the crown
rump length is a universally recognized term, very useful for measuring early
pregnancies. The CRL is highly reproducible and is the single most accurate
measure of gestational age. After 12 weeks, the accuracy of CRL in predicting
gestational age diminishes and is replaced by measurement of the fetal
biparietal diameter.
In at least some respects, the term "crown rump length" is
misleading:
- For much of the first trimester, there is no fetal crown and no fetal rump
to measure.
- Until 53 days from the LMP, the most caudad portion of the fetal cell mass
is the caudal neurospone, followed by the tail. Only after 53 days is the
fetal rump the most caudal portion of the fetus.
- Until 60 days from the LMP, the most cephalad portion of the fetal cell
mass is initially the rostral neurospore, and later the cervical flexure.
After 60 days, the fetal head becomes the most cephalad portion of the fetal
cell mass.
- What is really measured during this early development of the fetus is the
longest fetal diameter.
From 6 weeks to 9 1/2 weeks gestational age, the fetal CRL grows at a rate of
about 1 mm per day.
|
Gestational
Age (Weeks)
|
Sac
Size
(mm)
|
CRL
(mm)
|
|
4
|
3
|
|
|
5
|
6
|
|
|
6
|
14
|
|
|
7
|
27
|
8
|
|
8
|
29
|
15
|
|
9
|
33
|
21
|
|
10
|
|
31
|
|
11
|
|
41
|
|
12
|
|
51
|
|
13
|
|
71
|
Determination of Gestational
Age
Measurement of the gestational sac diameter or the length of the fetal pole (CRL)
can be used to determine gestational age. Charts have been developed for this
purpose, but some simple rules of thumb can also be effectively used.
- Gestational Sac: Gestational age = 4 weeks plus (mean sac diameter in mm x
days). This relies on the growth of the normal gestational sac of 1 mm per
day after the 4th week of gestation. For example, a gestational sac
measuring 11 mm would be approximately 5 weeks and 4 days gestational age.
(4 weeks plus 11 days = 5 weeks and 4 days).
- Crown Rump Length: Gestational age = 6 weeks plus (CRL x days). This
relies on the growth of the normal fetus of 1 mm per day after the 6th week
of gestation. For example, a CRL of 16 mm would correspond to a gestational
age of 8 weeks and two days (6 weeks plus 16 days = 8 weeks and 2 days).
|
Twins
Twins and other multiple gestations can usually be identified fairly early in
pregnancy. They may be seen with two separate gestational sacs (diamniotic,
dichorionic twins). They may be seen as two fetal poles occupying the same
gestational sac (monochorionic twins). It is useful to identify twins early as
the prognosis varies, depending on the chorionicity and amnionicity of the
twins.
|
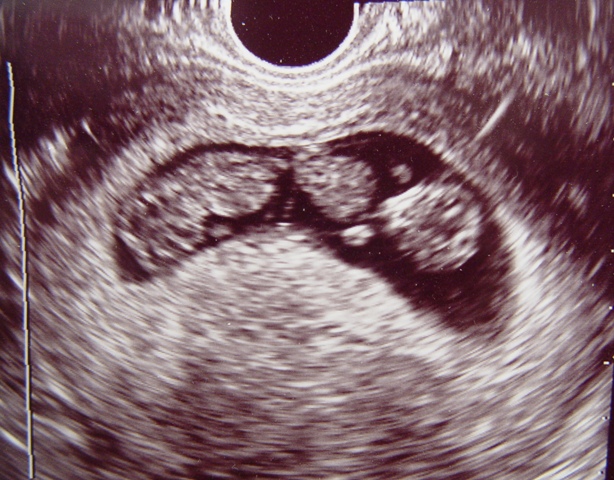
Twins |
A "vanishing twin" occurs in about 20% of twin pregnancies. In
these cases, one of the twins fails to grow and thrive. Instead, its development
arrests and it is reabsorbed, with no evidence at delivery of the twin
pregnancy. It will prove useful to advise patients of this phenomenon who are
found to have twins early in pregnancy.
Missed Abortion
A missed abortion is an abnormal pregnancy that is destined to miscarry.
About one in five early pregnancies will not survive. These will grow for a
while, with HCG in the urine and serum, but eventually will stop growing
normally, and then will stop growing at all. Most of these (two-thirds) will
have abnormal chromosomes. Evidence of a missed abortion using high-resolution
transvaginal scanning includes:
- Absence of a visible fetal heartbeat when the CRL is greater than 5 mm.
- Absence of a fetal pole when the average sac diameter is more than 18 mm.
- Loss of fetal cardiac activity that was previously seen.
Read
more about missed abortion
Threatened Abortion
A threatened abortion is any 1st trimester pregnancy that demonstrates uterine
bleeding and/or cramping. Such patients are frequently evaluated with
ultrasound. Bleeding in early pregnancy is a common event and is seen in 25 to
40% of pregnancies. About half of these will go on to miscarry while the other
half will be normal.
The benefits to ultrasound evaluation include:
- Detection of abnormal pregnancies that are destined to miscarry.
- Enabling scheduled intervention, if desired by the patient.
- Enabling collection of pregnancy tissue for chromosomal analysis, if
desired by the patient.
- Reassurance to the patients with normal ultrasound scans.
Unfortunately, diagnosis of an abnormal pregnancy does not allow for
intervention to correct the abnormality.
In the presence of uterine bleeding, visualization of a gestational sac, a
yolk sac, a fetal pole and fetal heart beat changes the risk of a threatened
abortion leading to miscarriage from 50/50 to about 5%.
Observation of subchorionic bleeding (blood outside the sac) is noted in
about 20% of patients with threatened abortion. This is a worrisome sign, and
reduces the pregnancy continuation rate to about 2/3.
Read
more about threatened abortion
Incomplete Abortion
Ultrasound is sometimes used after passage of pregnancy tissue to
determine whether any pregnancy tissue remains inside the uterus. Findings will
vary in these cases. Sometimes, it is obvious that there is nothing left inside
the uterus, as evidenced by a thin, complete endometrial stripe. In other cases,
there will be obvious pregnancy tissue. In the remaining cases, some material
will still be present inside the uterus, but it won't be clear (on ultrasound)
whether this is blood, blood clot, or retained products of conception.
Read
more about incomplete abortion
Ectopic Pregnancy
Early intrauterine pregnancies are relatively easy to see with high
resolution transvaginal ultrasound scanning. Pregnancies outside the uterus (ectopic
pregnancies) are more difficult. The appearance of the ectopic pregnancy itself
is the same as for intrauterine pregnancies. Depending of the gestational age
and normalcy of development, you may see a gestational sac, a yolk sac, a fetal
pole, and a fetal heartbeat. The difficulty lies in finding the pregnancy
without the normal uterine landmarks.
Using transvaginal scanning, about half of the ectopic pregnancies can be
directly visualized, but in the other half of cases, only indirect evidence of
an ectopic pregnancy will be found. Such indirect evidence includes:
- Absence of an identifiable intrauterine pregnancy with maternal serum HCG
levels of more than 1500 (this number varies and may be lower in some labs).
- Presence of an intrauterine gestational "pseudosac." These
thin-walled structures represent some fluid (sometimes blood) within a
decidualized endometrium that bears a superficial resemblence to a
gestational sac. However, it lacks the bright echogenic ring of a true
gestational sac and will never contain a yolk sac.
- Large amounts of free fluid (blood) inside the abdominal cavity. Small
amounts of free fluid are non-diagnostic, as this is commonly seen in cases
of spontaneous abortion, ruptured ovarian cysts, and ovulation.
Read
more about ectopic pregnancy
Corpus Luteum Cyst
Following release of the egg, the ovarian follicle changes into a corpus luteum,
responsible for production of hormones that will help support the developing
pregnancy. The observation of these small (usually less than 5 cm) ovarian cysts
during early pregnancy is essentially a normal finding. Should the cyst be large
(5 cm or more), or have suspicious characteristics, they may be followed as most
corpus luteum cysts will resolve spontaneously sometime during the first
trimester.
|
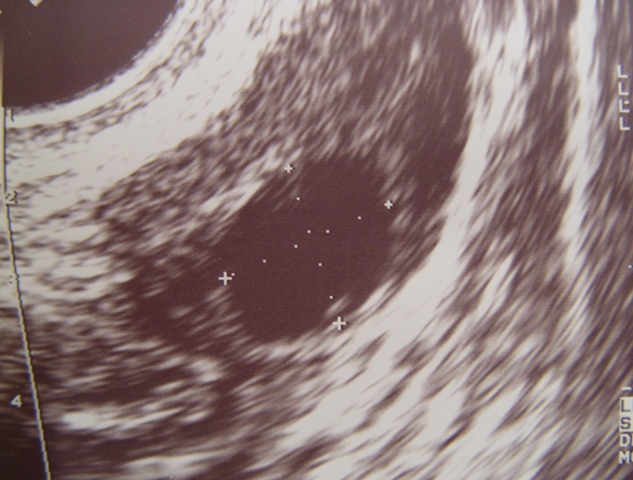
Ovarian Follicle |
Not all ovarian cysts identified during the first trimester are corpus luteum
cysts. Innocent paratubal cysts can be seen, requiring no treatment, as well as
ovarian dermoid tumors which can be more threatening.
Nuchal
Translucency Thickness
Late in the first trimester, an echolucent area can be identified at the
back of the neck of normal fetuses. Normally thin, it has been observed that an
unusually thick translucency is sometimes associated with such abnormalities as
trisomy 21 and other fetal malformations.
Between the 11th and end of the 13th week of gestation, the measurement of
nuchal translucency is obtained with the fetus in saggital section and a neutral
position of the fetal head (neither hyperflexed nor extended, either of which
can influence the nuchal translucency thickness). The fetal image is enlarged to
fill 75% of the screen, and the maximum thickness is measured, from leading edge
to leading edge. It is important to distinguish the nuchal lucency from the
underlying amnionic membrane.
Normal thickness depends on the overall size of the fetus (CRL), but it
should not exceed 3 mm at any gestational age. Among those fetuses whose nuchal
translucency exceeds the normal values, there is a relatively high risk of
significant abnormality. Between 65 and 85% of trisomic fetuses will have a
large nuchal thickness. Further, other, non-trisomic abnormalities may also
demonstrate an enlarged nuchal transparency. This leaves the measurement of
nuchal transparency as a potentially useful 1st trimester screening tool,
particularly in combination with biochemical screening. Abnormal findings allow
for early careful evaluation of chromosomes and possible structural defects on a
targeted basis.
|