|
Lesson 8: Perioperative Patient Care
SECTION IV. POSTOPERATIVE PATIENT CARE
8-16. RECEIVING THE POST-OP PATIENT
a. The nursing process is used during all phases of perioperative care, with emphasis on the special and unique needs of each patient in each phase. Ongoing postoperative care is planned to ease the patient's recovery from surgery. The nursing care plan includes promoting physical and psychological health, preventing complications, and teaching self-care for the patient's return home. While the patient is in the operating and recovery room, an unoccupied bed is prepared. The top linen is folded to the side or bottom of the bed. Absorbent pads are placed over the drawsheet to protect bottom linens. Equipment and supplies, such as blood pressure apparatus, tissues, an emesis basin, and a pole for hanging the intravenous fluid containers, should be in place when the patient returns. The unit nurse should be informed by the recovery room nurse if other items, such as suction or oxygen equipment will be needed.
b. Postoperative patient care begins with the unit nurse assisting recovery room personnel in transferring the patient to the bed in his room. Data from the preoperative and intraoperative phases is used to make an initial assessment. The assessment is often combined with implementation of the doctor's postoperative orders and should include the following.
(1) Position and safety. Place the patient in the position ordered by the doctor. The patient who has had spinal anesthesia may have to remain lying flat for several hours. If the patient is not fully conscious, place him in a side-lying position and raise the side rails.
(2) Vital signs. Take vital signs and note alterations from postoperative and recovery room data, as well as any symptoms of complications.
(3) Level of consciousness. Assess the patient's reaction to stimuli and ability to move extremities. Help the patient become oriented by telling him that his surgery is over and that he is back in his room.
(4) Intravenous fluids. Assess the type and amount of solution, the tubing, and the infusion site. Count the rate at which the intravenous fluid is infusing.
(5) Wound. Check the patient's dressing for drainage. Note the color and amount, if any. If there is a large amount of drainage or bright red bleeding, report this immediately to the supervisor.
(6) Drains and tubes. Assess indwelling urinary catheter, gastrointestinal suction, and other tubes for drainage, patency, and amount of output. Be sure drainage bags are hanging properly and suction is functioning. If the patient is receiving oxygen, be sure that the application and flow rate is as ordered.
(7) Color and temperature of skin. Feel the patient's skin for warmth and perspiration. Observe the patient for paleness or cyanosis.
(8) Comfort. Assess the patient for pain, nausea, and vomiting. If the patient has pain, note the location, duration and intensity. Determine from recovery room data if analgesics were given and at what time.
c. Make sure that the patient is warm and comfortable, and allow family members to visit after you have completed the initial assessment.
|
8-17. THE EFFECTS OF ANESTHESIA
a. The effects of anesthesia tend to last well into the postoperative period. Anesthetic agents may depress respiratory function, cardiac output, peristalsis and normal functioning of the gastrointestinal tract, and may temporarily depress bladder tone and response.
(1) Effects on the respiratory system. Pulmonary efficiency is reduced, increasing the possibility of postoperative pneumonia. Pneumonia is an inflammation of the alveoli resulting from an infectious process or the presence of foreign material. Pneumonia can occur postoperatively because of aspiration, infection, depressed cough reflex, immobilization, dehydration, or increased secretions from anesthesia. Signs and symptoms common to pneumonia are an elevated temperature, chills, cough producing purulent or rusty sputum, dyspnea, and chest pain. The purposes of medical intervention is to treat the underlying infection, maintain respiratory status, and prevent the spread of infection.
(2) Effects on the cardiovascular system. Anesthesia may affect cardiac output, thus increasing the possibility of unstable blood pressure. Shock is the reaction to acute peripheral circulatory failure because of an alteration in circulatory control or to a loss of circulating fluid.
(3) Effects on the urinary system. Anesthesia can cause urinary retention. Decreased fluid intake can lead to dehydration. Assess urinary elimination status by measuring intake and output. Offer the bedpan or urinal at regular intervals to promote voiding. If catheter is present, monitor drainage.
(4) Effects on gastrointestinal system. Anesthesia slows or stops the peristaltic action of the intestines resulting in constipation, abdominal distention, and flatulence. Anesthesia may also cause nausea and vomiting resulting in a fluid imbalance. Ordinarily, intravenous infusions are used while the patient takes nothing by mouth until bowel sounds are heard upon auscultation. Observe the patient for abdominal distention. Have the patient move about in bed and walk to help promote the movement and expulsion of the flatus.
b. A wide variety of factors increase the risk of postoperative complications. Comfort is often the priority for the patient following surgery. Nausea, vomiting, and other effects of anesthesia cause alterations in comfort. The nursing care plan should include activities to meet the patient's needs while helping him cope with these alterations.
8-18. OTHER POSTOPERATIVE COMPLICATIONS
a. Atelectasis is the incomplete expansion or collapse of alveoli with retained mucus, involving a portion of the lung and resulting in poor gas exchange. Signs and symptoms of atelectasis include dyspnea, cyanosis, restlessness, apprehension, crackles, and decreased lung sounds over affected areas. The primary purposes of care for the patient with atelectasis are to ensure oxygenation of tissue, prevent further atelectasis, and expand the involved lung tissue.
b. Hypovolemic shock is the type most commonly seen in the postoperative patient. Hypovolemic shock occurs when there is a decrease in blood volume. Signs and symptoms are hypotension; cold, clammy skin; a weak, thready and rapid pulse; deep, rapid respirations; decreased urine output; thirst; restlessness; and apprehension.
c. Hemorrhage is excessive blood loss, either internally or externally. Hemorrhage may lead to hypovolemic shock.
d. Thrombophlebitis is inflammation of a vein associated with thrombus (blood clot) formation. Thrombophlebitis is more commonly seen in the legs of a postoperative patient. Signs and symptoms are elevated temperature, pain and cramping in the calf or thigh of the involved extremity, redness and swelling in the affected area, and pain with dorsiflexion of the foot (figure 8-5). Care for the patient with thrombophlebitis includes preventing a clot from breaking loose and becoming an embolus that travels to the lungs, heart, or brain and preventing other clot formation.
|
a. Nursing implications in relation to prevention and early detection of wound complications include assessing vital signs, especially monitoring an elevated temperature; assisting the patient to maintain nutritional status, and use of medical asepsis. The integumentary system is the body's natural barrier against invasion of infectious microorganisms. Possible negative effects of surgery on the integumentary system include wound infection, dehiscence, and evisceration.
(1) Wound infection. Surgical wounds are assessed for possible complications by inspection (sight and smell) and palpation for appearance, drainage, and pain. The wound edges should be clean and well approximated with a crust along the wound edges. If infection is present, the wound is slightly swollen, reddened, and feels hot. Hand washing is the most frequently used medical aseptic practice and the single most effective way to prevent the spread of microorganisms that cause wound infections.
(2) Dehiscence. Dehiscence is the separation of wound edges without the protrusion of organs. An appreciable increase in serosanguinous fluid on the wound dressing (usually between the 6th and 8th postoperative day) is a clue to impending dehiscence.
(3) Evisceration. Evisceration is the separation of wound edges with the protrusion of organs through the incision. Wound disruption is often preceded by sudden straining. The patient may feel that something "gave way."
b. If dehiscence is suspected or occurs, place the patient on complete bed rest in a position that puts the least strain on the operative area and notify the surgeon. If evisceration occurs, cover the wound area with sterile towels soaked in saline solution and notify the surgeon immediately. These are both emergency situations that require prompt surgical repair.
c. Predisposing factors and causes of wound separation are:
(1) Infection.
(2) Malnutrition , particularly insufficient protein and vitamin C, which interferes with the normal healing process.
(3) Defective suturing or allergic reaction to the suture material.
(4) Unusual strain on the wound from severe vomiting, coughing, or sneezing.
(5) Extreme obesity, an enlarged abdomen, or an abdomen weakened by prior surgeries may also contribute to the occurrence of wound dehiscence and evisceration.
8-20. WOUND CLOSURES AND HEALING
a. Any wound or injury results in repair to the damaged skin and underlying structures. All wounds follow the same phases in healing, although differences occur in the length of time required for each phase of the healing process and in the extent of granulation tissue formed. Wounds heal by one of three processes: primary, secondary, or tertiary intention.
(1) Primary intention is the ideal method of wound healing. The wound is a clean, straight line with little loss of tissue. All wound edges are well approximated and sutured closed. It is a form of connective tissue repair that involves proliferation of fibroblasts and capillary buds and the subsequent development of collagen to produce a scar. Most surgical incisions and small sutured lacerations heal by primary intention. These wounds normally heal rapidly with minimal scarring.
(2) Secondary intention is healing of an open wound where there has been a significant loss of tissue. The edges may be so far apart that they cannot be pulled together satisfactorily. Infection may also cause a separation of tissue surfaces and prevent wound approximation. The wound is usually not sutured closed. Granulation tissue is allowed to form, followed by a large scar formation. Epithelium ultimately grows over the scar tissue.
(3) Tertiary intention is delayed primary closure. The wound is left open for several days and is then sutured closed. There is increased risk of infection and inflammatory reaction. The wound is usually one that is fairly deep and likely to contain accumulating fluid. A drain or pack gauze may be placed into the wound to provide for drainage.
b. The greater the tissue damage, the greater the demand on the body's reparative processes. The ability to close an open wound affects the rate of healing and prevention of complications.
8-21. FACTORS WHICH MAY IMPAIR WOUND HEALING
a. Developmental Stage. Children and adults in good health heal more rapidly than do elderly persons who have undergone physiologic changes that result in diminished fibroblastic activity and diminished circulation. Older adults are more likely to have chronic illnesses that cause pathologic changes that may impair wound healing.
b. Poor Circulation and Oxygenation. Blood supply to the affected area may be diminished in elderly persons and in those with peripheral vascular disorders, cardiovascular disorders, hypertension, or diabetes mellitus. Oxygenation of tissues is decreased in persons who smoke, and in those with anemia or respiratory disorders. Obesity slows wound healing because of the presence of large amounts of fat, which has fewer blood vessels.
c. Physical and Emotional Wellness. Chronic physical illness and severe emotional stress have a negative affect on wound healing. Patients who have inadequate nutrition, those who are taking steroid drugs, and those who are receiving postoperative radiation therapy have a higher risk of wound complications and impaired wound healing.
d. Condition of the Wound. The specific condition of the wound affects the healing process. Wounds that are infected or contain foreign bodies (including drains, pack gauze) heal slowly.
a. Inserting Drains. The use of drains, tubes, and suction devices at the wound site is often necessary to promote healing. A drain or tube is inserted into or near a wound after the surgical procedure is completed. One end of a tube or drain is placed in or near the incision when it is anticipated that fluid will collect in the closed area and delay healing. The other tube end is passed through the incision or through a separate opening called a stab wound. Tubes that are to be connected to suction or have a built-in reservoir are sutured to the skin. It is important that you know the type of drain or tube in use so that patency and placement can be accurately assessed.
b. Penrose Drain (figure 8-6). This is the most commonly used drain. It is made of flexible, soft rubber and causes little tissue reaction. It acts by drawing any pus or fluid along its surfaces through the incision or through a stab wound adjacent to the main incision. It has a large safety pin outside the wound to maintain its position. To facilitate drainage and healing of tissues from the inside to the outside, the tube is often pulled out and shortened 1 to 2 inches each day until it falls out. The safety pin should be placed in its new position prior to cutting the drain. Advance the drain with a dressing forceps or hemostat, use surgical scissors to cut excess drain.
c. Jackson-Pratt/Hemovac Closed Suction Device (figure 8-7). Tubes are connected to suction or there is a built-in reservoir to maintain constant low suction. In the operating room, the surgeon places the perforated drainage tubing in the desired area, makes a stab wound, then draws the excess tubing through the wound creating a tightly sealed porthole. The tubing is then attached via an adaptor to the suction device. To establish negative pressure, compress the device and place the plug in the air hole.
8-23. POSTOPERATIVE PATIENT CARE ACCORDING TO BODY SYSTEM
a. Respiratory System. The cough reflex is suppressed during surgery and mucous accumulates in the trachea and bronchi. After surgery, respiration is less effective because of the anesthesia and pain medication, and because deep respirations cause pain at the incision site. As a result, the alveoli do not inflate and may collapse, and retained secretions increase the potential for respiratory infection and atelectasis.
(1) Turn the patient as ordered.
(2) Ambulate the patient as ordered.
(3) If permitted, place the patient in a semi-Fowler's position, with support for the neck and shoulders, to aid lung expansion.
(4) Reinforce the deep breathing exercises the patient was taught preoperatively. Deep breathing exercises hyperventilate the alveoli and prevent their collapse, improve lung expansion and volume, help to expel anesthetic gases and mucus, and facilitate oxygenation of tissues. Ask the patient to:
(a) Exhale gently and completely.
(b) Inhale through the nose gently and completely.
(c) Hold his breath and mentally count to three.
(d) Exhale as completely as possible through pursed lips as if to whistle.
(e) Repeat these steps three times every hour while awake.
(5) Coughing, in conjunction with deep breathing, helps to remove retained mucus from the respiratory tract. Coughing is painful for the postoperative patient. While in a semi-Fowler's position, the patient should support the incision with a pillow or folded bath blanket and follow these guidelines for effective coughing:
(a) Inhale and exhale deeply and slowly through the nose three times.
(b) Take a deep breath and hold it for 3 seconds.
(c) Give two or three "hacking" coughs while exhaling with the mouth open and the tongue out.
(d) Take a deep breath with the mouth open.
(e) Cough deeply once or twice.
(f) Take another deep breath.
(g) Repeat these steps every 2 hours while awake.
(6) An incentive spirometer may be ordered to help increase lung volume, inflation of alveoli, and facilitate venous return. Most patients learn to use this device and can carry out the procedure without a nurse in attendance. Monitor the patient from time to time to motivate them to use the spirometer and to be sure that they use it correctly.
(a) While in an upright position, the patient should take two or three normal breaths, then insert the spirometer's mouthpiece into his mouth.
(b) Inhale through the mouth and hold the breath for 3 to 5 seconds.
(c) Exhale slowly and fully.
(d) Repeat this sequence 10 times during each waking hour for the first 5 post-op days. Do not use the spirometer immediately before or after meals.
b. Cardiovascular System. Venous return from the legs slows during surgery and may actually decrease in some surgical positions. With circulatory stasis of the legs, thrombophlebitis and emboli are potential complications of surgery. Venous return is increased by flexion and contraction of the leg muscles.
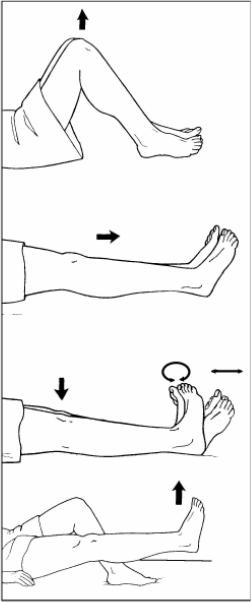
(1) To prevent thrombophlebitis, instruct the patient to exercise the legs while on bedrest. Leg exercises are easier if the patient is in a supine position with the head of the bed slightly raised to relax abdominal muscles. Leg exercises (figure 8-8) should be individualized using the following guidelines.
(a) Flex and extend the knees, pressing the backs of the knees down toward the mattress on extension.
(b) Alternately, point the toes toward the chin (dorsiflex) and toward the foot of the bed (plantar flex); then, make a circle with the toes.
(c) Raise and lower each leg, keeping the leg straight.
(d) Repeat leg exercises every 1 to 2 hours.
(2) Ambulate the patient as ordered.
(a) Provide physical support for the first attempts.
(b) Have the patient dangle the legs at the bedside before ambulation.
(c) Monitor the patient's blood pressure while he dangles.
(d) If the patient is hypotensive or experiences dizziness while dangling, do not ambulate. Report this event to the supervisor.
c. Urinary System. Patients who have had abdominal surgery, particularly in the lower abdominal and pelvic regions, often have difficulty urinating after surgery. The sensation of needing to urinate may temporarily decrease from operative trauma in the region near the bladder. The fear of pain may cause the patient to feel tense and have difficulty urinating.
(1) If the patient does not have a catheter, and has not voided within eight hours after return to the nursing unit, report this event to the supervisor.
(2) Palpate the patient's bladder for distention and assess the patient's response. The area over the bladder may feel rounder and slightly cooler than the rest of the abdomen. The patient may tell you that he feels a sense of fullness and urgency.
(3) Assist the patient to void.
(a) Assist the patient to the bathroom or provide privacy.
(b) Position the patient comfortably on the bedpan or offer the urinal.
(4) Measure and record urine output. If the first urine voided following surgery is less than 30 cc, notify the supervisor.
(5) If there is blood or other abnormal content in the urine, or the patient complains of pain when voiding, report this to the supervisor.
(6) Follow nursing unit standing operating procedures (SOP) for infection control, when caring for the patient with a Foley catheter.
d. Gastrointestinal System. Inactivity and altered fluid and food intake during the perioperative period alter gastrointestinal activities. Nausea and vomiting may result from an accumulation of stomach contents before peristalsis returns or from manipulation of organs during the surgical procedure if the patient had abdominal surgery.
(1) Report to the supervisor if the patient complains of abdominal distention.
(2) Ask the patient if he has passed gas since returning from surgery.
(3) Auscultate for bowel sounds. Report your assessment to the supervisor, and document in nursing notes.
(4) Assess abdominal distention, especially if bowel sounds are not audible or are high-pitched, indicating an absence of peristalsis.
(5) Provide a privacy so that the patient will feel comfortable expelling gas.
(6) Encourage food and fluid intake when the patient in no longer NPO.
(7) Ambulate the patient to assist peristalsis and help relieve gas pain, which is a common postoperative discomfort.
(8) Instruct the patient to tell you of his first bowel movement following surgery. Record the bowel movement on the intake and output (I&O) sheet.
(9) If nursing measures are not effective, the doctor may order medication or an enema to facilitate peristalsis and relieve distention. A last measure may require the insertion of a nasogastric or rectal tube.
(10) Document nursing measures and the results in the nursing notes.
e. Integumentary System. Follow doctor's orders for wound care, wound irrigations and cultures. In addition to assessment of the surgical wound, you should evaluate the patient's general condition and laboratory test results. If the patient complains of increased or constant pain from the wound, or if wound edges are swollen or there is purulent drainage, further assessment should be made and your findings reported and documented. Generalized malaise, increased pain, anorexia, and an elevated body temperature and pulse rate are indicators of infection. Important laboratory data include an elevated white blood cell count and the causative organism if a wound culture is done. Staples or sutures are usually removed by the doctor using sterile technique. After the staples or sutures are removed, the doctor may apply Steri-Strip® to the wound to give support as it continues to heal.
|
Precautions for Contact with Blood and Body Fluids
|
(1) There are two methods of caring for wounds: the open method, in which no dressing is used to cover the wound, and the closed method, in which a dressing is applied. The basic objective of wound care is to promote tissue repair and regeneration, so that skin integrity is restores. Dressings have advantages and disadvantages.
(a) Advantages. Dressings absorb drainage, protect the wound from injury and contamination, and provide physical, psychological, and aesthetic comfort for the patient.
(b) Disadvantages. Dressings can rub or stick to the wound, causing superficial injury. Dressings create a warm, damp, and dark environment conducive to the growth of organisms and resultant infection.
(2) At some time, most wounds are covered with a dressing and you may be responsible for changing the dressing. First, gather needed supplies. Items may be packaged individually or all necessary items may be in a sterile dressing tray. Some surgical units have special dressing carts, with agents needed to clean the wound, and materials to cover and secure the dressing. Next, prepare the patient for the dressing change by explaining what will be done, providing privacy for the procedure, and assisting the patient to a position that is comfortable for him and for you. Finally, use appropriate aseptic techniques when changing the dressing and follow precautions for contact with blood and body fluids. The most common cause of nosocomial infections is carelessness in observing medical and surgical asepsis when changing dressings. It is especially important to wash hands thoroughly before and after changing dressings and to follow the Centers for Disease Control (CDC) guidelines (figure 8-9).
8-24. GENERAL POSTOPERATIVE NURSING IMPLICATIONS
a. Monitor vital signs as ordered.
b. Report elevated temperature and rapid/weak pulse immediately to supervisor (infection).
c. Report lowered blood pressure and increased pulse to supervisor (hypovolemic shock).
d. Administer analgesics as ordered.
e. Apply all nursing implications related to the patient receiving analgesics whether narcotic or nonnarcotic, to include the following.
(1) Check each medication order against the doctor's order.
(2) Prepare the medications (check labels, accurately calculate dosages, observe proper asepsis techniques with needles and syringes).
(3) Check the patient's identification wristband to ensure positive identification before administering medications.
(4) Administer the medications. Offer each drug separately if administering more than one drug at the same time.
(5) Remain with the patient and see that the medication is taken. Never leave medications at the bedside for the patient to take later.
(6) Document the medications given as soon as possible.
f. Administer IV fluids as ordered. Maintain and monitor all IV sites. Follow SOP for infection control.
g. Participate with the health team in the patient's nutrition therapy.
h. Apply all nursing implications related to the patient diets (serving, recording intake, and food tolerance).
i. Coordinate with team leader for "take-home" wound care supplies and prescriptions for self-administration.
j. Prepare the patient and the family for disposition (transfer, return to duty, discharge). Supply the patient or family member with written instructions for:
(1) Wound care.
(2) Medications.
(3) Making outpatient appointments.
(4) An emergency, including the phone numbers for doctors and/or clinics.
k. Document the patient's disposition in the nurse's notes in accordance with unit SOP.
Surgical intervention often alters physical appearance and normal physiological functions and may threaten the patients psychological security. Any or all of these may lead to alterations in the patient's self-concept and body image. Some surgical patients react to the loss of a body part as to a death. Be aware of the patient's needs and establish interventions that will support his strengths and effective coping skills. The nursing process is used throughout the perioperative period to provide the patient with individualized care and the knowledge and ability for self-care following disposition.