|
Lesson 8: Perioperative Patient Care
SECTION II. THE INTRAOPERATIVE PHASE
a. Key Members. The intraoperative phase begins when the patient is received in the surgical area and lasts until the patient is transferred to the recovery area. Although the surgeon has the most important role in this phase, there are five key members of the surgical team.
b. The Surgeon. The surgeon is the leader of the surgical team. The surgeon is ultimately responsible for performing the surgery effectively and safely; however, he is dependent upon other members of the team for the patient's emotional well being and physiologic monitoring.
c. Anesthesiologist/Anesthetist. An anesthesiologist is a physician trained in the administration of anesthetics. An anesthetist is a registered professional nurse trained to administer anesthetics. The responsibilities of the anesthesiologist or anesthetist include:
(1) Providing a smooth induction of the patient's anesthesia in order to prevent pain.
(2) Maintaining satisfactory degrees of relaxation of the patient for the duration of the surgical procedure.
(3) Continuous monitoring of the physiologic status of the patient for the duration of the surgical procedure.
(4) Continuous monitoring of the physiologic status of the patient to include oxygen exchange, systemic circulation, neurologic status, and vital signs.
(5) Advising the surgeon of impending complications and independently intervening as necessary.
d. Scrub Nurse/Assistant. The scrub nurse or scrub assistant is a nurse or surgical technician who prepares the surgical set-up, maintains surgical asepsis while draping and handling instruments, and assists the surgeon by passing instruments, sutures, and supplies. The scrub nurse must have extensive knowledge of all instruments and how they are used. In the Army, the Operating Room Technician (MOS 91D) often fills this role. The scrub nurse or assistant wears sterile gown, cap, mask, and gloves.
e. Circulating Nurse. The circulating nurse is a professional registered nurse who is liaison between scrubbed personnel and those outside of the operating room. The circulating nurse is free to respond to request from the surgeon, anesthesiologist or anesthetist, obtain supplies, deliver supplies to the sterile field, and carry out the nursing care plan. The circulating nurse does not scrub or wear sterile gloves or a sterile gown. Other responsibilities include:
(1) Initial assessment of the patient on admission to the operating room, helping monitoring the patient.
(2) Assisting the surgeon and scrub nurse to don sterile gowns and gloves.
(3) Anticipating the need for equipment, instruments, medications, and blood components, opening packages so that the scrub nurse can remove the sterile supplies, preparing labels, and arranging for transfer of specimens to the laboratory for analysis.
(4) Saving all used and discarded gauze sponges, and at the end of the operation, counting the number of sponges, instruments, and needles used during the operation to prevent the accidental loss of an item in the wound.
8-7. MAJOR CLASSIFICATIONS OF ANESTHETIC AGENTS
|
a. There are three major classifications of anesthetic agents: general anesthetic, regional anesthetic, and local anesthetic. A general anesthetic produces loss of consciousness and thus affects the total person. When the patient is given drugs to produce central nervous system depression, it is termed general anesthesia.
(1) There are three phases of general anesthesia: induction, maintenance, and emergence. Induction, (rendering the patient unconscious) begins with administration of the anesthetic agent and continues until the patient is ready for the incision. Maintenance (surgical anesthesia) begins with the initial incision and continues until near completion of the procedure. Emergence begins when the patient starts to come out from under the effects of the anesthesia and usually ends when the patient leaves the operating room. The advantage of general anesthesia is that it can be used for patients of any age and for any surgical procedure, and leave the patient unaware of the physical trauma. The disadvantage is that it carries major risks of circulatory and respiratory depression.
(2) Routes of administration of a general anesthetic agent are rectal (which is not used much in today's medical practices), intravenous infusion, and inhalation. No single anesthetic meets the criteria for an ideal general anesthetic. To obtain optimal effects and decrease likelihood of toxicity, administration of a general anesthetic requires the use of one or more agents. Often an intravenous drug such as thiopental sodium (Pentothal) is used for induction and then supplemented with other agents to produce surgical anesthesia. Inhalation anesthesia is often used because it has the advantage of rapid excretion and reversal of effects.
(3) Characteristics of the ideal general anesthetic are:
(a) It produces analgesia.
(b) It produces complete loss of consciousness.
(c) It provides a degree of muscle relaxation.
(d) It dulls reflexes.
(e) It is safe and has minimal side effects.
(4) General anesthesia is used for major head and neck surgery, intracranial surgery, thoracic surgery, upper abdominal surgery, and surgery of the upper and lower extremities.
b. A regional or block anesthetic agent causes loss of sensation in a large region of the body. The patient remains awake but loses sensation in the specific region anesthetized. In some instances, reflexes are lost also. When an anesthetic agent is injected near a nerve or nerve pathway, it is termed regional anesthesia.
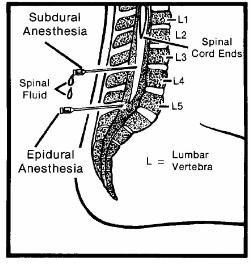
(1) Regional anesthesia may be accomplished by nerve blocks, or subdural or epidural blocks (see figure 8-3).
(2) Nerve blocks are done by injecting a local anesthetic around a nerve trunk supplying the area of surgery such as the jaw, face, and extremities.
(3) Subdural blocks are used to provide spinal anesthesia. The injection of an anesthetic, through a lumbar puncture, into the cerebrospinal fluid in the subarachnoid space causes sensory, motor and autonomic blockage, and is used for surgery of the lower abdomen, perineum, and lower extremities. Side effects of spinal anesthesia include headache, hypotension, and urinary retention.
(4) For epidural block, the agent is injected through the lumbar interspace into the epidural space, that is, outside the spinal canal.
c. Local anesthesia is administration of an anesthetic agent directly into the tissues. It may be applied topically to skin surfaces and the mucous membranes in the nasopharynx, mouth, vagina, or rectum or injected intradermally into the tissue. Local infiltration is used in suturing small wounds and in minor surgical procedures such as skin biopsy. Topical anesthesia is used on mucous membranes, open skin surfaces, wounds, and burns. The advantage of local anesthesia is that it acts quickly and has few side-effects.
8-8. SELECTION OF AN ANESTHETIC AGENT
a. Depending on its classification, anesthesia produces states such as narcosis (loss of consciousness), analgesia (insensibility to pain), loss of reflexes, and relaxation. General anesthesia produces all of these responses. Regional anesthesia does not cause narcosis, but does result in analgesia and reflex loss. Local anesthesia results in loss of sensation in a small area of tissue.
b. The choice of route and the type of anesthesia is primarily made by the anesthetist or anesthesiologist after discussion with the patient. Whether by intravenous, inhalation, oral, or rectal route, many factors effect the selection of an anesthetic agent:
(1) The type of surgery.
(2) The location and type of anesthetic agent required.
(3) The anticipated length of the procedure.
(4) The patient's condition.
(5) The patient's age.
(6) The patient's previous experiences with anesthesia.
(7) The available equipment.
(8) Preferences of the anesthesiologist or anesthetist and the patient.
(9) The skill of the anesthesiologist or anesthetist.
c. Factors considered by the anesthetist or anesthesiologist when selecting an agent are the smoking and drinking habits of the patient, any medications the patient is taking, and the presence of disease. Of particular concern are pulmonary function, hepatic function, renal function, and cardiovascular function.
(1) Pulmonary function is adversely affected by upper respiratory tract infections and chronic obstructive lung diseases such as emphysema, especially when intensified by the effects of general anesthesia. These conditions also predispose the patient to postoperative lung infections.
(2) Liver diseases such as cirrhosis impair the ability of the liver to detoxify medications used during surgery, to produce the prothrombin necessary for blood clotting, and to metabolize nutrients essential for healing following surgery.
(3) Renal insufficiency may alter the excretion of drugs and influence the patient's response to the anesthesia. Regulation of fluids and electrolytes, as well as acid-base balance, may be impaired by renal disease.
(4) Well-controlled cardiac conditions pose minimal surgical risks. Severe hypertension, congestive heart failure, or recent myocardial infarction drastically increase the risks.
d. Medications, whether prescribed or over-the-counter, can affect the patient's reaction to the anesthetic agent, increase the effects of the anesthesia, and increase the risk from the stress of surgery. Medication is usually withheld when the patient goes to surgery; but some specific medications are given even then. For example, patients with cardiovascular problems or diabetes mellitus may continue to receive their prescribed medications.
(1) Because some medications interact adversely with other medications and with anesthetic agents, preoperative assessment should include a thorough medication history. Patients may be taking medication for conditions unrelated to the surgery, and are unaware of the potential for adverse reactions of these medications with anesthetic agents.
(2) Drugs in the following categories increase surgical risk.
(a) Adrenal steroids--abrupt withdrawal may cause cardiovascular collapse in long-term users.
(b) Antibiotics--may be incompatible with anesthetic agent, resulting in untoward reactions. Those in mycin group may cause respiratory paralysis when combined with certain muscle relaxants used during surgery.
(c) Anticoagulants--may precipitate hemorrhage.
(d) Diuretics--may cause electrolyte (especially potassium) imbalances, resulting in respiratory depression from the anesthesia.
(e) Tranquilizers--may increase the hypotensive effect of the anesthetic agent, thus contributing to shock.
8-9. REASONS FOR SURGICAL INTERVENTION
Descriptors used to classify surgical procedures include ablative, diagnostic, constructive, reconstructive, palliative, and transplant. These descriptors are directly related to the reasons for surgical intervention:
a. To cure an illness or disease by removing the diseased tissue or organs.
b. To visualize internal structures during diagnosis.
c. To obtain tissue for examination.
d. To prevent disease or injury.
e. To improve appearance.
f. To repair or remove traumatized tissue and structures.
g. To relieve symptoms or pain.