Menopause
Physiology · Symptoms · Medical Issues · Osteoporosis · Philosophy of Menopause · Benefits and Risks of Estrogen · Breast Cancer · Progesterone · Testosterone · Estrogen Replacement Regimens · Serum Estradiol · Abnormal Bleeding · Resumption of Ovarian
Function
Menopause is the physiologic cessation of ovarian function (and
menstrual flows) that occurs with advancing age in all women. In North
America, the average age of menopause is 51, but there is considerable
variation from individual to individual. Some (a few) 55 year olds are
still having normal menstrual cycles, while some (a few) 47 year olds
have stopped.
Many people view menopause as a distinct point in time,
beyond which all ovarian function ceases. That might be true for a few
women, but for most, menopause is a more gradual process, characterized
by waxing and waning ovarian function over a period of many years.
During this time, ovarian function may cease altogether for a few months
(accompanied by vasomotor symptoms and amenorrhea), only to return (with
disappearance of the symptoms and resumption of menstrual flows). This
"off again, on again" pattern is not at all unusual and is probably more
the rule than the exception. This many-year period of time is frequently
called "peri-menopause."
Physiology
Ovarian function consists of:
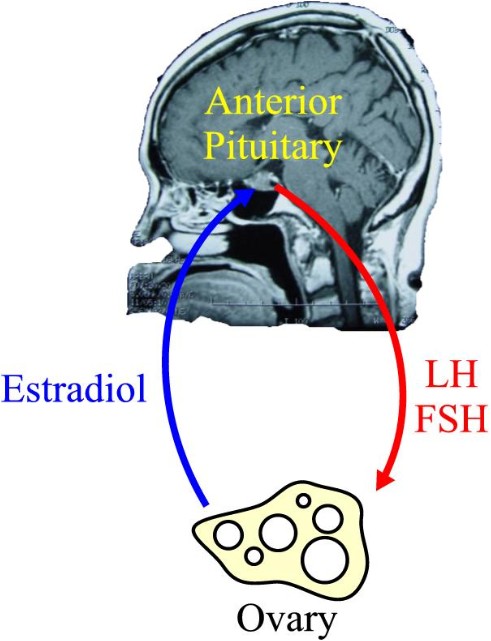
During the reproductive years, the ovaries function under control of
the anterior pituitary gland, through its release of follicle
stimulating hormone (FSH) and luteinizing hormone (LH). This causes
production of estrogen (quite a bit), progesterone (some), testosterone
(not much, but very important), and ovulation. Of these functions,
ovulation is the most complex, while production of testosterone is the
simplest.
The estradiol (estrogen) produced by the ovary circulates through the
woman's bloodstream to receptors in the brain (primarily anterior
pituitary), where it inhibits release of FSH. Consequently, the stimulus
to the ovary to produce its hormones and release its eggs diminishes,
menstruation occurs, and the whole process begins anew.
Menopause occurs because the ovaries stop responding to FSH and LH,
not because the brain stops releasing FSH and LH. A menopausal woman
will generally have very high levels of FSH and LH, but very low levels
of estrogen (estradiol) in her bloodstream.
Symptoms
Common symptoms of menopause include:
-
Hot flashes (sudden, unprovoked flushing of the face and trunk,
accompanied by redness and profuse sweating, and often followed by
chills.
-
Night sweats (awakening in the middle of the night drenched in
sweat, requiring a change in night clothes).
-
Vaginal dryness (particularly noticable during intercourse)
-
Diminished memory (forgetfulness)
-
Dry skin
-
Mood changes, including fatigue, depression and irritability
-
Sleeplessness
-
Cessation of menstrual flows
-
Decreased libido
Medical Issues
Accompanying menopause are two medical problems, bone loss and heart
disease.
Women slowly lose bone mass, starting at a relatively early age.
Menopause rapidly accelerates this process, resulting in osteopenia
(decreased bone density) or osteoporosis (so much bone loss that
pathologic fractures are a realistic possibility).
The incidence of heart disease also increases rapidly after
menopause. During their reproductive years, women enjoy a substantial
advantage over men in heart disease. With menopause, the risk of heart
disease among women rises to that of men, with women losing the relative
protection that they had earlier.
Osteoporosis
This demineralization problem can be extremely serious. Pathologic
fractures are notorious for poor healing. The morbidity and mortality
associated with recovery from fractures of the hip, spine and long bones
is substantial.
Taking extra calcium (1000-1500 grams of elemental
calcium/day) is helpful in preventing osteoporosis, but the help is very
small. Similarly, regular weight-bearing exercise is helpful, but only
to a limited extent. Taking estrogen helps a great deal, but usually
won't reverse the effects of osteoporosis. Bisphosphonates, such as alendronate are even more powerful and can reverse osteoporosis,
although they can cause significant side effects.
Increased risk factors for osteoporosis include:
Bone density studies (Dexa Scan) will
show a T-value of -2.5 or worse among women with osteoporosis.
Osteopenic women have T-values of -1.0 to -2.5.
 Philosophy of Menopause Philosophy of Menopause
Two basically opposite and conflicting philosophies of menopause
complicate the treatment of menopause.
One philosophy holds that:
-
Menopause is a natural event, affecting everyone sooner or later.
-
The normal status of women after approximately age 50 is to be
menopausal, without any estrogen.
-
The role of medication, if any, is to ease the transition from
pre-menopause to menopause, helping women adjust to not having any
estrogen
-
Any medical treatment of menopause should involve the smallest
amount of the fewest number of medications, for the shortest period of
time possible. Then, the medications should be steadily withdrawn so
that the menopausal woman will not become dependent upon it.
The other philosophy holds that:
-
Menopause is an estrogen-deficiency state.
-
Womanhood is more or less defined by the effects of estrogen,
which assists in the development not only of the breasts and genitals,
but the skin, body fat, voice, memory, verbal skills, and to some
extent the charitable disposition, sociability, and nurturing
personalities that are so characteristic of women across geographic
and racial boundaries.
-
Estrogen deprivation creates problems that are not only medical,
but frequently annoying, psychologically distressing, and largely
corrected through the use of estrogen replacement therapy.
-
The fact that everyone is affected by menopause sooner or later
should not deter us from treating it, any more than the commonality of
arthritis or age-related dementia would deter us from treating them.
-
We should treat estrogen-deficient women with estrogen to restore
them to their normal status, just as we would treat hypothyroid
patients with thyroid medication to make them euthyroid, or give
diabetic patients insulin...enough to restore them to their normal
situation.
-
Menopause is not a universal experience in the animal kingdom...it
is seen only among humans.
Given these two differing philosophies, it is not difficult to
imagine that there are disagreements among conscientious practitioners
as to the proper role of estrogen replacement therapy.
Menopause is a relatively new issue in the human experience. Until
recently, very few women lived long enough to reach menopause. The
average life expectancy for women in North America in 1900 was age 42.
Currently it is age 82. Because of this, our clinical experience with
large numbers of menopausal patients is really limited to the last
century. As physicians, I expect we will learn a great deal more about
menopause in the coming century, when the philosophical differences may
be resolved.
 Benefits and Risks of Estrogen
Replacement Therapy Benefits and Risks of Estrogen
Replacement Therapy
There is conflicting evidence in research studies about the relative
benefits and risks of estrogen replacement therapy. That said, it is
probably true that estrogen replacement of the proper dose will:
-
Eliminate hot flashes and night sweats
-
Provide moderate protection of the bones against demineralization
-
Improve or eliminate vaginal dryness
-
Improve sleep
-
Improve memory
-
Provide for an improved general sense of well-being for many
menopausal women.
It is also probably true that estrogen replacement therapy:
-
Will not protect against cardiovascular disease and may increase
that risk slightly
-
Will increase the risk of gall bladder disease.
-
Will not affect the overall risk of developing cancer.
-
For those who develop cancer while taking estrogen replacement,
will increase the chance that the cancer will originate in the breast,
but decrease the risk of it arising in the colon or uterus.
-
Will not affect the overall risk of death
-
Will increase the risk of certain types of strokes, while
decreasing the risk of other types of strokes, with an overall slight
increase in risk of stroke from all types.
Breast Cancer
There is conflicting evidence over the role of estrogen in causing
breast cancer, causing its recurrence, or speeding its growth and
development. Some physicians feel that any woman with a past history of
breast cancer should never take estrogen. Others feel that for some
women, the risks are modest (particularly if the breast cancer was many
years ago), and the benefits in terms of quality of life are
considerable, and willingly prescribe estrogen to these patients.
Progesterone
Taken alone, estrogen replacement in standard doses is associated with
an increased risk of uterine cancer. The addition of progesterone to the
estrogen not only blocks the increased risk of uterine cancer, it
reduces the risk to less than that of women who don't take any ERT at
all. For this reason, progesterone has routinely been added to estrogen
replacement regimens for women who have uteruses. Women who have
undergone hysterectomy have no need for the progesterone addition.
Progesterone blunts, to some extent, some of the other estrogenic
effects, and the best of the long term studies have not reported their
results from estrogen-alone therapies. It is possible that some of the
risks of ERT are actually a result of the progesterone.
Testosterone
Male hormone, primarily testosterone, is produced in small amounts by
women, with about one-third coming from the ovaries. As ovarian function
gradually slows down, testosterone production stops, usually a few years
after the onset of amenorrhea. At that time, serum testosterone levels
will fall by about 30%.
For many women, this 30% drop in testosterone
will be unnoticed. For others, they may experience symptoms of low
testosterone, the most prominent of which are lethargy and decreased sex
drive.
For women with complaints of lethargy and decreased libido during
menopause, some physicians will routinely measure serum testosterone. If
testosterone levels are relatively low, these women may benefit from a
therapeutic trial of small doses of testosterone, usually in addition to
estrogen replacement. Serum testosterone levels are followed to make
sure that the woman is not receiving too much hormone. Many women find
this combination neatly resolves their symptoms.
Not everyone benefits from this regimen. Some have side-effects (hair
growth, voice changes, adverse lipid changes), that require stopping the
testosterone. Others notice no difference in their energy levels or
libido.
Continuous
therapy: |
|
Cyclic therapy: |
|
*May substitue estradiol 1.0 mg |
**May substitute
micronized progesterone 100 mg |
Estrogen Replacement Regimens
A number of satisfactory treatment strategies and doses are available
for estrogen replacement therapy. They include both continuous and
cyclic approaches. The benefits to continuous therapy are simplicity and
absence of menstrual bleeding in the majority of women. For a minority,
spotting or breakthrough bleeding complicate continuous therapy and
these women generally do better on a cyclic approach. For those on
cyclic therapy, 1/3 experience normal menstrual flows, 1/3 have no
periods at all, and 1/3 will initially experience menstrual flows, but
the flows will gradually abate over time. The following are examples of
typical ERT doses:
Once the patient is started on the estrogen
replacement, it is important to see how she's doing in 1-3 months after
starting it. If she continues to have vasomotor symptoms, then she needs
a higher dose of estrogen. If she has persistent breast tenderness or
headaches, she may be getting too much estrogen. Measuring serum
estrogen (estradiol) levels may prove helpful in managing such women.
Serum Estradiol Levels |
Proliferative Phase |
60-250
pg/ml |
Luteal
Phase |
75-450
pg/ml |
Menopause |
<10
pg/ml |
ERT |
50-100
pg/ml |
Serum Estradiol
Blood estrogen levels may be useful in the management of many menopausal
women and their estrogen replacement therapy.
During the reproductive
years, estrogen levels vary with the menstrual cycle:
In menopause, the estradiol levels typically are less than 32 pg/ml
and often <10. When treating menopausal women with estrogen, a
reasonable target would be estradiol levels of 50-100 pg/ml. If the
patient has levels a little higher or lower, but feels fine, then she
can remain on the same dose. However, a woman on standard doses of
estrogen who continues to have vasomotor symptoms and whose estradiol
level is only 40 will likely benefit from a higher dose, nudging her
into the typical therapeutic range.
 Abnormal Bleeding Abnormal Bleeding
The progesterone component of estrogen replacement therapy provides some
protection against endometrial hyperplasia and carcinoma, but the
protection is not absolute. For that reason, women taking estrogen
replacement therapy who experience abnormal bleeding (any bleeding that
is not expected) should be carefully evaluated. Usually, nothing
significant is found.
Resumption of ovarian
function
It is relatively common for women who are started on estrogen
replacement therapy to resume some degree of ovarian function. Giving
estrogen will inhibit the release of FSH and LH and serum levels of
these gonadotropins will fall. Then, in response to stopping the
estrogen (as in some forms of cyclic therapy), the FSH will again rise.
The ovaries, particularly if they are still relatively close to the time
of menopause may respond briefly to the rising level of FSH, even though
they didn't respond to the sustained high levels of FSH.
Such an
occurrence can lead to brief resumption of estrogen production (and
resultant estrogen excess symptoms of breast tenderness or bleeding), or
even ovulation (resulting in a full-blown menstrual period two weeks
later). Pregnancy occurring in this circumstance would be very unlikely
because the the quality of the older ovarian follicle is usually poor.
The main problem is an unexpected menstrual flow occurring in a woman
who was advised she was menopausal and who is now receiving treatment
for menopause. An advance explanation of this possibility will relieve
the patient's anxiety and concern over the depth of your knowledge and
skill.
At least two approaches to this problem can be effective:
-
One approach is to stop estrogen replacement and allow the woman's
natural cycle to continue for as long as it wants. Eventually, she
will again become amenorrheic and experience vasomotor symptoms and
conventional ERT can be resumed.
-
A second approach is to switch from conventional ERT to oral
contraceptive pills. The pills have enough estrogen in them to provide
reasonable coverage for most women, and the progestin is strong enough
to suppress further ovarian function. After taking the OCPs for a
reasonable time (6-12 months), she can be switched back to
conventional ERT.
|