1-18. VISUAL DEFECTS
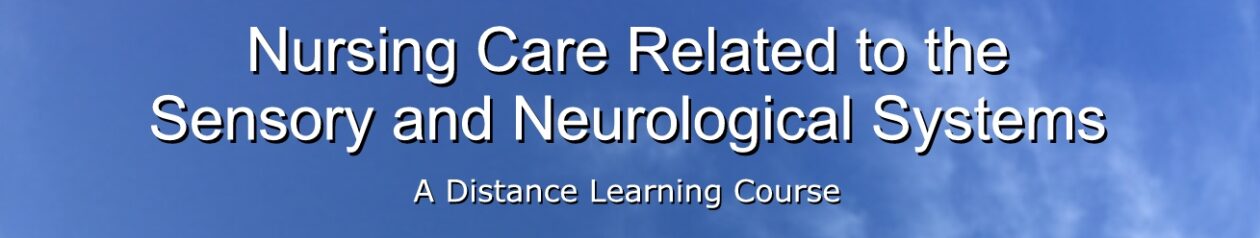
a. Myopia. Also referred to as “nearsightedness”, myopia is a refractive error caused by a structural defect of the eye.
(1) The eyeball is too long from front to back, causing light rays to focus in front of the retina rather than on it.
(2) Close objects can be seen more clearly than distant objects, which appear blurred and unfocused.
(3) Vision may be corrected with the use of a concave lens, which will cause the light rays to focus on the retina.
b. Hyperopia. Also known as hypermetropia and “farsightedness”, hyperopia is a refractive error caused by a structural defect of the eye.
(1) The eyeball is too short from front to back, causing light rays to focus behind the retina rather than on it.
(2) Distant objects can be seen more clearly than those close up. Near objects are blurred and unfocused.
(3) Vision may be corrected with the use of a convex lens, which will cause the light rays to focus on the retina.
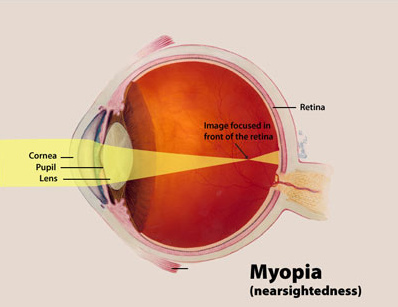
c. Presbyopia. Presbyopia is a refractive error caused by a decrease in the power of accommodation of the crystalline lens, due to weakening of the ciliary muscles with aging.
(1) The near point of distinct vision becomes further from the eye. (This is why you may see someone reading while holding the reading material at arm’s length.)
(2) Vision may be improved with the use of corrective lenses such as bifocals, which have a small lens for near vision placed within the lower half of a larger lens for distant vision.
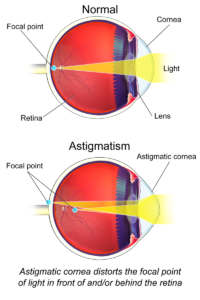
d. Astigmatism. This is a refractive error caused by uneven curvature of the refractive surfaces of the eye.
(1) Light rays are not focused along equal planes because of the curvature, causing vision to be unfocused.
(2) Vision can be improved with the use of a lens called a cylinder lens, which compensates for the uneven curvature and allows the light rays to focus sharply.
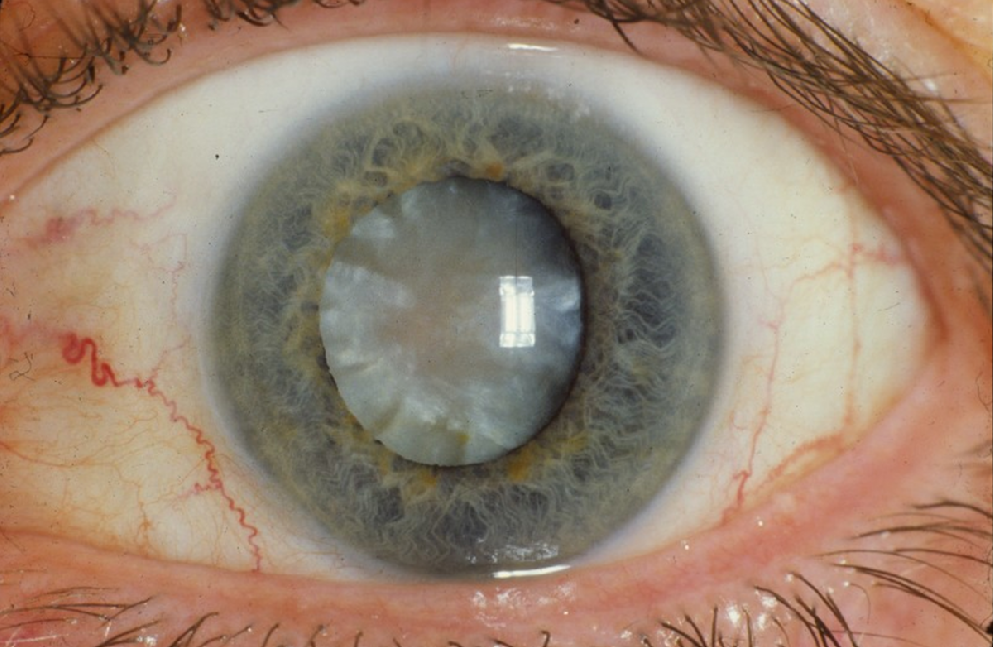
e. Cataract. A cataract is an opacity of the crystalline lens or its capsule. It is the leading cause of blindness in the United States.
(1) Vision becomes distorted and/or unfocused. Bright lights produce a glare.
(2) Vision is improved by surgical removal of the opaque lens. The missing lens is compensated for by the use of special eyeglasses or contact lenses, or by intraocular implant of an artificial lens.
f. Glaucoma. Glaucoma is a condition in which there is increased pressure within the eyeball. If uncorrected, glaucoma will lead to blindness.
(1) Increased pressure is caused by faulty drainage of aqueous fluid.
(2) Drug therapy is used to promote drainage of the aqueous fluid, or decrease the production rate of the aqueous fluid, or both.
(3) When drug therapy is not effective, surgical intervention is indicated. There are many different procedures used, but the objective of all is to decrease intraocular pressure by facilitating the filtration and drainage of the aqueous fluid.
1-19. CONJUNCTIVITIS

Conjunctivitis is the inflammation of the conjunctiva. It is also referred to as “pink eye.”
a. Causes of conjunctivitis include:
(1) Allergies.
(2) Physical trauma.
(3) Chemical irritation.
(4) Bacterial or viral infection.
b. Signs and symptoms include:
(1) Redness.
(2) Lacrimation (tearing).
(3) Swelling.
(4) Discharge.
(5) Pain.
c. Nursing management includes:
(1) Normal saline irrigations to flush out drainage.
(2) Warm compresses (15 minutes, 3-4 times per day).
(3) Administration of prescribed therapeutic medications.
(4) Patient education to avoid further irritation or spread of infection.
1-20. DETACHED RETINA
Detachment of the sensory retina from the pigment epithelium of the retina causes loss of clear vision. Tears, rips, or holes in the retina allow the vitreous humor to seep behind the retina, separating it from the epithelium. Unless the holes are sealed, the retina will progressively detach. There will be loss of central vision as well as peripheral vision.
a. Causes of detached retina include:
(1) Trauma (rapid detachment and visual deterioration).
(2) Aging (slow process of deteriorating vision).
b. Signs and symptoms of retinal detachment include:
(1) Flashes of light.
(2) Blurred vision.
(3) Sensations of “particles” or “lights” in the visual fields.
(4) Progressive loss of peripheral vision.
c. Nursing implications:
(1) Detachment of the retina must be corrected surgically. There are many different procedures used, but the objective of all is to seal the retinal holes, ensuring that the retina adheres to the retinal pigment epithelium.
(2) Nursing care should involve all aspects of care for the patient undergoing ophthalmic surgery. Refer to the following paragraphs for care of patients undergoing ophthalmic surgery.
1-21. PREOPERATIVE NURSING CARE OF THE PATIENT UNDERGOING OPHTHALMIC SURGERY
The eye is a delicate and important organ, and its care and protection are of the utmost importance. Common conditions of the eye that may require surgical intervention include trauma, cataract, glaucoma, and detached retina. The ophthalmologist will determine the treatment required and procedure of choice in each patient’s case. The procedure may vary from a simple incision to facilitate drainage to total removal of the eyeball (enucleation).
a. Physical Orientation. The patient will require a thorough orientation to his immediate hospital environment. This is done to help the patient during the postoperative period, since he may be blind as a result of the procedure or the need for the eyes to be patched.
(1) Assist the patient to learn details of his room such as the location of furniture, doors, windows, and so forth.
(2) Familiarize the patient with the voices of those who will care for him after surgery. Familiarize him with the daily sounds and noises in the environment, since he will be more aware of sound without his vision.
b. Observation. The patient should be observed for tendencies to cough or sneeze (smoker’s cough, allergies, and so forth). Such observations should be reported to the professional nurse for consideration in the plan of care. Such violent movements of the head during the postoperative course may cause increased intraocular pressure, leading to hemorrhage or rupture of incisions.
c. Education. The patient must receive a thorough education about the postoperative course of events and his responsibilities and restrictions. The patient must understand the objective of resting the eyes and avoiding actions that increase intraocular pressure.
(1) The head must be kept very still.
(2) No reading.
(3) No showers, no shampooing, no tub baths.
(4) No bending over at the waist.
(5) No lifting of heavy objects.
(6) No sleeping on the operative side. If both eyes are affected, the patient must sleep on his back.
d. Physical Preparation.
(1) A bowel prep is done the evening prior to surgery to prevent the patient from straining at stool during the immediate post-op period.
(2) Shaving of eyebrows, cutting of eyelashes, and shaving of face should be done only on the order of the surgeon.
(3) After the patient has been taken to surgery, prepare a post-op bed, ensuring that the bed is equipped with side rails.
(4) Sand bags should be made available for use in immobilizing the head.
e. Family. Often, if the patient must be kept absolutely still or will be temporarily blinded after surgery, a member of the family may be asked to stay with the patient. If this is the case, the family member should receive the same orientation and education given to the patient.
1-22. POSTOPERATIVE NURSING CARE OF THE PATIENT UNDERGOING OPHTHALMIC SURGERY
a. Return from Surgery.
(1) The patient must be lifted off the litter, he is not to move himself.
(2) The patient should be positioned in the bed as prescribed by the physician.
(3) Sandbags should be used to immobilize the patient’s head, if ordered.
(4) If both eyes are bandaged (they normally are), the side rails MUST be raised at all times to protect the patient in the event he becomes disoriented and attempts to get out of bed.
(5) Place the call bell within easy reach of the patient’s head and let the patient know exactly where it is located.
(6) Remind the patient that he should not cough, sneeze, or blow his nose. Instruct him to inform the staff if he feels the urge, since these actions will increase intraocular pressure.
b. Orientation.
(1) Reinforce the physical orientation given during the preoperative period by verbally reviewing the locations of objects in the room.
(2) Orient the patient to other people in the room.
(3) The patient should have an awareness of his surroundings and know what to expect to avoid being startled or frightened.
c. Precautions.
(1) Avoid dislodgement of the eye dressings by securing them with an eye shield or reinforcing loose tape.
(2) Restrain the arms of children and disoriented or uncooperative patients, as appropriate.
(3) A sleeping patient must be watched constantly to ensure that proper positioning is maintained. Often, a family member may be asked to stay with the patient for this purpose.
(4) Avoid jarring or bumping the bed, as this may startle the patient.
(5) If the patient is newly blinded as a result of the surgery, observe for depression and take precautions if patient is potentially suicidal.
(6) Check the physician’s orders before giving anything by mouth. Nausea and vomiting must be avoided. Additionally, the motion of chewing may be contraindicated.
d. Approaching the Patient. An important consideration in the care of a patient who has both eyes bandaged is the method of approaching him.
(1) ALWAYS speak to the patient upon entering his area and before touching him.
(2) Allay the patient’s fears by explaining each procedure or activity fully.
(3) Continue to reinforce his orientation to the surroundings.
(4) Always let the patient know when you are leaving his area.
e. Diversional Activity. Diversional activities will promote a relaxed atmosphere for convalescence and prevent the patient from dwelling on his situation.
(1) Provide activities that are not fatiguing to the eyes if the eyes are not bandaged.
(a) No reading.
(b) Minimal television.
(2) Encourage visitors to chat with the patient or read to him.
(3) Encourage the use of a radio for entertainment and to keep the patient “in touch” with current events if he is unable to read the daily newspaper.
1-23. NURSING CARE OF THE PATIENT WITH VISION LOSS
a. Physical Orientation. To prevent injury and encourage independence, the patient with vision loss should receive a thorough orientation to his surroundings.
(1) Describe the room and its contents in detail, so that the patient can form a mental image of his room.
(2) Lead the patient around the room, letting him feel the furniture, windows, and doorways. (3) Orient the patient to any personnel that may be expected to enter his room. For example, housekeeping personnel or laboratory technicians.
(4) Familiarize the patient with the sounds of his environment. Explain the source of those he is unfamiliar with. Remember, a patient with vision loss depends heavily on his hearing for environmental cues and orientation.
(5) Orient the patient to things around him by comparing their location to the numbers on the face of a clock, with the patient located in the center of the clock.
(a) When describing his room, identify locations by clock reference. For example, the bathroom door is at 2 o’clock and the door to the hallway is at 9 o’clock.
(b) When describing the food on his plate, identify the location of the food items by clock reference. For example, the potatoes are at 12 o’clock, the green beans are at 3 o’clock, the roast beef is at 6 o’clock, and the biscuit is at 9 o’clock.
b. Precautions. To protect the patient from accidental injury, follow these guidelines.
(1) Inform the patient when something in his room has been moved or is different from usual.
(2) Keep doors completely opened or completely closed. This will prevent walking into a partially opened door.
(3) Keep toilet articles in the location the patient places them. Do not move them without telling the patient.
(4) Remove hazardous items such as light cords, small trash cans, and other items that the patient could trip over.
c. Assisting the Patient.
(1) Always address the patient by name when entering his area.
(2) Always let the patient know when you are leaving his area.
(3) When walking with the patient, do not hold him or walk behind him and push him along. Allow the patient to place his hand on your arm or shoulder and walk beside you.
(4) Encourage the patient to be independent and self-sufficient.