1-7. EXAMINATION OF THE EYE
An examination of the eye includes an external examination, examination by ophthalmoscope, and an assessment of the functions of the eye.
Basic Eye Exam from University of Iowa Ophthalmology on Vimeo.
a. External Examination. The anterior segment of the eyes and their appendages can be examined by visual inspection.
(1) Note the general appearance of the eyelids, eyelashes, and lacrimal apparatus. Observe for:
(a) Redness around the eye.
(b) Discharge or crusting.
(c) Growths on eyes or eyelids.
(d) Excessive tearing.
(2) Position and mobility can be observed by having the patient rotate the eyes, looking up, down, and to each side.
b. Pupillary Response. Normal pupils are rounded, centrally placed, and generally equal in size. (About 25 percent of normal individuals have pupils slightly unequal in size.)
(1) Reaction to light. Seat the patient in an area with even lighting and instruct him to fix his gaze on a distant object. Cover one eye and shine a flashlight in front of the exposed eye. The pupil should contract (constrict) because of the light. This response is called a direct reaction. The covered pupil should also contract. This response is called a consensual reaction.
(2) Near point reaction. When the gaze is changed from a distant object to an object close at hand, the pupils should contract.
c. Ophthalmoscopic Examination. By looking through the various lenses of an ophthalmoscope, the trained examiner can view and assess the internal structures of the eye. This examination is routinely performed by the physician.
d. Functional Examinations.
(1) Focusing power (power of accommodation) is tested by placing a line of print close to the eye, then slowly moving it back to the point at which the patient is able to read it. The nearest point at which it is readable is the near point of accommodation.
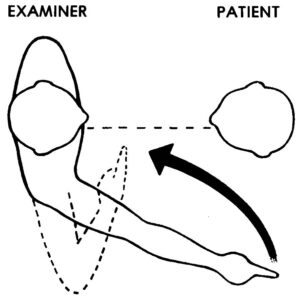
(2) Visual field refers to all that can be seen with both eyes fixed straight ahead. To perform a gross examination of visual field, the confrontation method is used (figure. 1-3). Have the patient and the examiner face each other at a distance of about 2-3 feet, each focusing his gaze at the other’s nose. The examiner should then extend his arm to the side, point his finger, and slowly move his arm back in, along a plane half-way between himself and the patient. The examiner’s finger should appear in the patient’s visual field at the same time the examiner sees it (assuming the examiner’s visual field is grossly normal).
(3) Color sense is tested by using specially designed color plates to distinguish reds, greens, and blues.
(4) Visual acuity testing is done with the Snellen chart or one of its modifications. Each eye is tested separately, both with and without glasses, if worn.
(a) Since the distance at which rays of light from an object are practically parallel and no accommodation of the lens is necessary to focus the object, the test is performed at a distance of 6 meters (20 feet),
(b) The Snellen chart contains rows of letters of varying sizes, arranged to that the normal eye can see them at distances of 6, 9, 12, 15, 21, 30, and 60 meters. (20, 30, 40, 50, 70, 100, and 200 feet.) If a patient is seated 6 meters (20 feet) from the chart and can read the line of letters for 6 meters, his vision is expressed by the fraction 6/6 (or 20/20).
(c) Vision is expressed by a fraction, the numerator denoting the distance at which the test was performed (normally, 6 meters or 20 feet), and the denominator denoting the smallest line of letters which could be read at that distance. If a patient is seated 6 meters from the chart and the smallest line of letters he is able to read is the one that should be read at a distance of 30 meters, then his vision is expressed at 6/30 (or 20/100).
(d) If the largest letters on the chart cannot be read at a distance of 6 meters, the patient is moved toward the chart until he can read the largest letters. Vision is then expressed as a fraction, with the numerator denoting the distance at which the largest line could be read, and the denominator denoting the number of the largest line.
(e) If the patient cannot read the largest line at a distance of one meter, the examiner tests the patient’s ability to see hand motion in front of his face. If the patient cannot see the examiner’s hand at a distance of one or two meters, he is tested for light perception. A light is flashed from different directions and the patient is asked from which direction the light appears and when it goes on and, it goes off. If the patient can do this, the examination is recorded as “light perception present”. If no light perception is present, a person is technically blind.
(5) These functional examinations are routinely performed by the physician or eye specialist. However, it is recommended that nursing personnel be knowledgeable of these examinations. To do so will facilitate identification of visual abnormalities. A gross examination using “field expedient techniques” can be performed when the proper equipment and personnel are not available. For example:
(a) Color sense can be observed by having the patient identify the color of objects around him.
(b) Gross acuity can be tested by having the patient read signs posted on the walls. Use signs of different sizes and position the patient at varying distances.
1-8. ASSESSING SYMPTOMS
In addition to the examinations mentioned previously, the patient should be assessed for the following:
a. Discomfort or pain in or around the eye.
b. Photophobia. (Abnormal sensitivity to light.)
c. Nystagmus. (Involuntary, rapid movement of the eyeball. May be horizontal, vertical, rotational, or mixed.)
d. Strabismus. (Deviation of the eye from the normal physiological axis: “crossed eyes.”)
e. Diplopia. (Seeing an object in double: “double vision.”)
f. Blurred vision.
g. “Spots” or “lights” in the visual field.
1-9. EXAMINATION OF THE EAR
a. The auditory canal is examined by means of an otoscope and ear speculum. The patient normally sits in an upright position for the exam. The lighted otoscope is inserted, using the largest speculum that will fit comfortably into the patient’s external ear canal.
b. Look through the eyepiece and examine the external ear canal for:
(1) Discharge.
(2) Impacted cerumen.
(3) Inflammation.
(4) Masses.
(5) Foreign bodies.
c. Examine the tympanic membrane for:
(1) Luster.
(2) Transparency.
(3) Integrity.
(4) Scarring.
(5) Color.
1-10. AUDIOMETRY
a. Hearing tests are conducted with a device called an audiometer. This apparatus produces sounds of specific frequencies and intensities. The patient sits in a soundproof room and listens to the sounds over a set of earphones. Sounds of varying frequency and intensity are than transmitted to each ear separately. The patient signals when a sound is heard by raising his hand or pressing a button to indicate which ear heard the sound. When a sound is transmitted and the patient does not signal, the examiner records that the sound was not heard.
b. When this equipment is not available, a gross examination can be performed using “field expedient techniques.” Have the patient sit with eyes closed and ask him to identify sounds made by an examiner moving in a perimeter around the patient. The patient should identify from which direction the sound originated and the type of sound heard. Sounds can be created by whistling, whispering, tapping, playing a radio, and so forth.
1-11. ASSESSING SYMPTOMS
In addition to the examinations mentioned above, the patient should be evaluated for signs that may be indicative of hearing defects.
a. Failure to react to loud noises.
b. Inattentiveness in a group conversation.
c. Inappropriate responses in conversation.
d. Facial expressions which indicate a difficulty in understanding what has been said.
e. Habitually asking “what?”
f. Speaking in a loud or monotonous voice.
g. Speech that is slurred or unclear.
h. Complaint of ringing, buzzing, or roaring in the ears. (Tinnitus)
i. Sensation of pressure or fullness in the ears.
j. Discomfort or pain in or around the ears.
k. Light-headedness, dizziness, or loss of balance.