Duration 16:23
Teaching Script: Ovarian Neoplasm
Clinical Case Applicability:
Adnexal Mass, Complications of Metastatic Disease
Learning Objectives:
1) Understand the different cell types involved in ovarian neoplasms
2) Review use of biochemical markers in identifying ovarian neoplasms (CA125 and larger sequence used)
3) Review genetic predispositions to ovarian neoplasm (briefly BRCA and Lynch syndrome)
Clinical Presentation:
Pregnancy with ovarian mass; Perimenopausal with gastrointestinal symptoms and adnexal mass
Considering anatomy and histology of the ovary, what cell types may evolve into ovarian neoplasms?
• Ovarian Anatomy
o Premenopausal ovaries are about 3x2x2 cm in size; suspended between the ovarian ligament medially and the
infundipulopelvic ligament laterally and superiorly.
o Outer cortex: ova and follicles; Inner medulla: fibromuscular layer of blood vessels and connective tissue
• Ovarian Cell types: 3 main types of which several neoplasms can emerge.
o Epithelial: derived from stem cells that would give rise to the fallopian tube and ovarian surface epithelium
o Germ Cell Tumors: derived from primordial germ cells of the ovary
o Sex Cord Stromal Tumors: derived from stems cells that would create the ovarian stroma or follicles
• Epithelial Tumors (90% of ovarian malignancies)
o Benign Epithelial tumors include: serous cystadenoma, mucinous cystadenoma or endometroid
o Malignant Epithelial tumors include:
§ High grade serous carcinoma: key feature is marked cytologic atypia with prominent mitotic activity.
§ Endometrioid carcinoma: usually presents in women 40-50yo and diagnosed at an early
§ Clear cell carcinoma: arises from endometriosis in perimenopausal women. Tubal ligation protective.
§ Mucinous carcinoma: nearly all present stage I; usually perimenopausal women, usually very big up to 20cm and
confined to one side, have KRAS mutation that seems to indicate the mucinous cyst carcinoma arises from
mucinous cystadenomas and mucinous borderline tumors
§ Low grade serous carcinoma: key feature is hyalinized stroma with numerous psammoma bodies
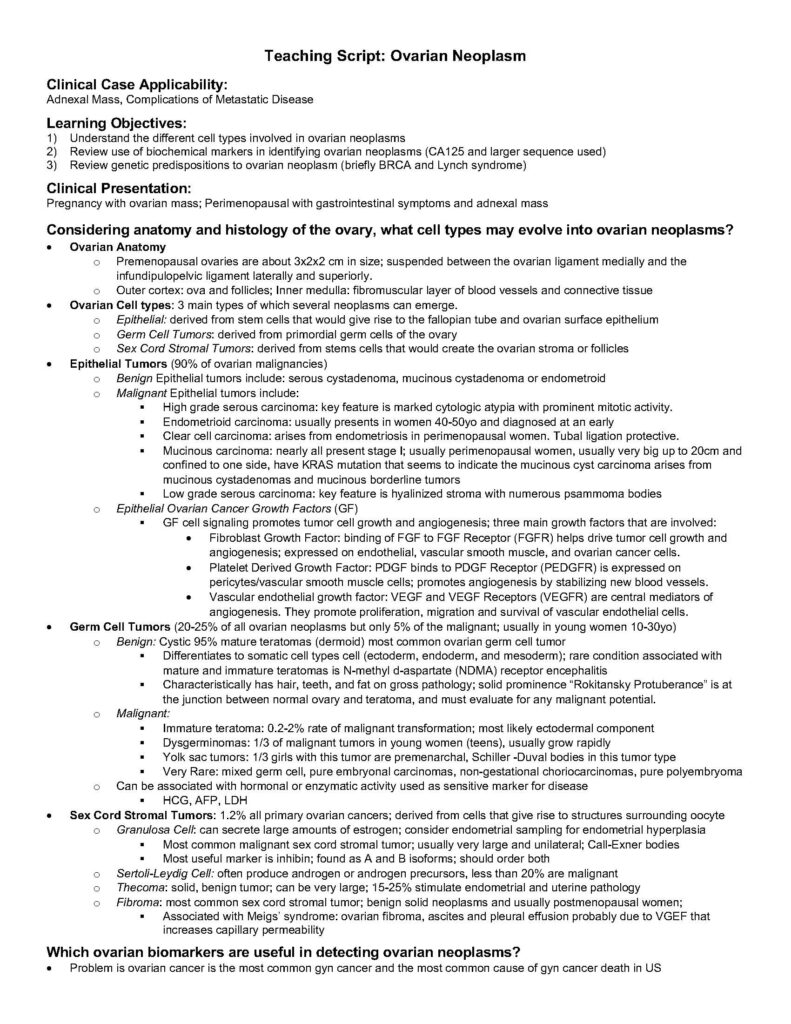
o Epithelial Ovarian Cancer Growth Factors (GF)
§ GF cell signaling promotes tumor cell growth and angiogenesis; three main growth factors that are involved:
• Fibroblast Growth Factor: binding of FGF to FGF Receptor (FGFR) helps drive tumor cell growth and
angiogenesis; expressed on endothelial, vascular smooth muscle, and ovarian cancer cells.
• Platelet Derived Growth Factor: PDGF binds to PDGF Receptor (PEDGFR) is expressed on
pericytes/vascular smooth muscle cells; promotes angiogenesis by stabilizing new blood vessels.
• Vascular endothelial growth factor: VEGF and VEGF Receptors (VEGFR) are central mediators of
angiogenesis. They promote proliferation, migration and survival of vascular endothelial cells.
• Germ Cell Tumors (20-25% of all ovarian neoplasms but only 5% of the malignant; usually in young women 10-30yo)
o Benign: Cystic 95% mature teratomas (dermoid) most common ovarian germ cell tumor
§ Differentiates to somatic cell types cell (ectoderm, endoderm, and mesoderm); rare condition associated with
mature and immature teratomas is N-methyl d-aspartate (NDMA) receptor encephalitis
§ Characteristically has hair, teeth, and fat on gross pathology; solid prominence “Rokitansky Protuberance” is at
the junction between normal ovary and teratoma, and must evaluate for any malignant potential.
o Malignant:
§ Immature teratoma: 0.2-2% rate of malignant transformation; most likely ectodermal component
§ Dysgerminomas: 1/3 of malignant tumors in young women (teens), usually grow rapidly
§ Yolk sac tumors: 1/3 girls with this tumor are premenarchal, Schiller -Duval bodies in this tumor type
§ Very Rare: mixed germ cell, pure embryonal carcinomas, non-gestational choriocarcinomas, pure polyembryoma
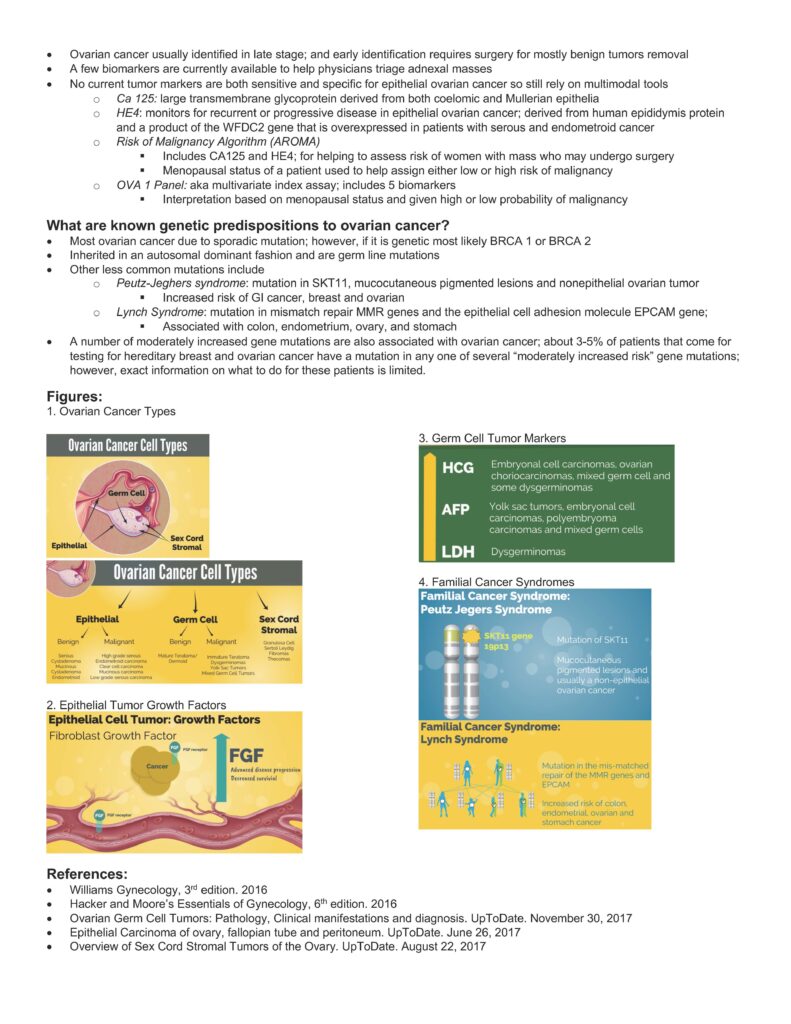
o Can be associated with hormonal or enzymatic activity used as sensitive marker for disease
§ HCG, AFP, LDH
• Sex Cord Stromal Tumors: 1.2% all primary ovarian cancers; derived from cells that give rise to structures surrounding oocyte
o Granulosa Cell: can secrete large amounts of estrogen; consider endometrial sampling for endometrial hyperplasia
§ Most common malignant sex cord stromal tumor; usually very large and unilateral; Call-Exner bodies
§ Most useful marker is inhibin; found as A and B isoforms; should order both
o Sertoli-Leydig Cell: often produce androgen or androgen precursors, less than 20% are malignant
o Thecoma: solid, benign tumor; can be very large; 15-25% stimulate endometrial and uterine pathology
o Fibroma: most common sex cord stromal tumor; benign solid neoplasms and usually postmenopausal women;
§ Associated with Meigs’ syndrome: ovarian fibroma, ascites and pleural effusion probably due to VGEF that
increases capillary permeability
Which ovarian biomarkers are useful in detecting ovarian neoplasms?
• Problem is ovarian cancer is the most common gyn cancer and the most common cause of gyn cancer death in US
• Ovarian cancer usually identified in late stage; and early identification requires surgery for mostly benign tumors removal
• A few biomarkers are currently available to help physicians triage adnexal masses
• No current tumor markers are both sensitive and specific for epithelial ovarian cancer so still rely on multimodal tools
o Ca 125: large transmembrane glycoprotein derived from both coelomic and Mullerian epithelia
o HE4: monitors for recurrent or progressive disease in epithelial ovarian cancer; derived from human epididymis protein
and a product of the WFDC2 gene that is overexpressed in patients with serous and endometroid cancer
o Risk of Malignancy Algorithm (AROMA)
§ Includes CA125 and HE4; for helping to assess risk of women with mass who may undergo surgery
§ Menopausal status of a patient used to help assign either low or high risk of malignancy
o OVA 1 Panel: aka multivariate index assay; includes 5 biomarkers
§ Interpretation based on menopausal status and given high or low probability of malignancy
What are known genetic predispositions to ovarian cancer?
• Most ovarian cancer due to sporadic mutation; however, if it is genetic most likely BRCA 1 or BRCA 2
• Inherited in an autosomal dominant fashion and are germ line mutations
• Other less common mutations include
o Peutz-Jeghers syndrome: mutation in SKT11, mucocutaneous pigmented lesions and nonepithelial ovarian tumor
§ Increased risk of GI cancer, breast and ovarian
o Lynch Syndrome: mutation in mismatch repair MMR genes and the epithelial cell adhesion molecule EPCAM gene;
§ Associated with colon, endometrium, ovary, and stomach
• A number of moderately increased gene mutations are also associated with ovarian cancer; about 3-5% of patients that come for
testing for hereditary breast and ovarian cancer have a mutation in any one of several “moderately increased risk” gene mutations;
however, exact information on what to do for these patients is limited.
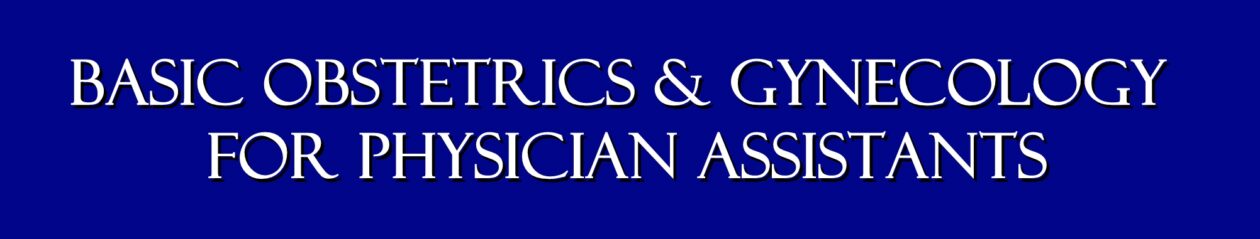
Figures:
1. Ovarian Cancer Types
2. Epithelial Tumor Growth Factors
3. Germ Cell Tumor Markers
4. Familial Cancer Syndromes
References:
• Williams Gynecology, 3rd edition. 2016
• Hacker and Moore’s Essentials of Gynecology, 6th edition. 2016
• Ovarian Germ Cell Tumors: Pathology, Clinical manifestations and diagnosis. UpToDate. November 30, 2017
• Epithelial Carcinoma of ovary, fallopian tube and peritoneum. UpToDate. June 26, 2017
• Overview of Sex Cord Stromal Tumors of the Ovary. UpToDate. August 22, 2017
Duration 15:09
Introduction
Adnexal masses may be encountered during a routine examination of an asymptomatic patient. They may be found while evaluating a patient with pain, bleeding, or other troublesome symptoms. Most of these masses will be benign and largely self-resolving, while a few will prove dangerous or life-threatening. The challenge, of course, is to determine which is which.
Simple Ovarian Cysts are the most common cause for an adnexal mass.
An ovarian cyst is a fluid-filled sac arising from the ovary.
Ovarian cysts can be broadly categorized as having two origins: physiologic cysts that occur as a consequence of ovulation, and neoplastic cysts. Of the two, ovulation- related cysts are by far the more common.
Functional cysts are common and generally cause no trouble. Each time a woman ovulates, she forms a small ovarian cyst (about 3.0 cm in diameter or less).
Depending on where she is in her menstrual cycle, you may find such a small ovarian follicular cyst. Large cysts (>7.0 cm) are less common and should be followed clinically or with ultrasound.
Occasionally, simple ovarian cysts may cause a problem by: Delaying menstruation, Rupturing , Twisting , or Causing pain .
About 95% of clinically significant ovarian cysts disappear spontaneously, usually after the next menstrual flow. Those that remain and those causing problems are often removed surgically.
Most Unruptured Ovarian Cysts will have no symptoms, but they can cause pain, particularly with strenuous exercise or intercourse. Treatment is symptomatic with rest for those with significant pain. The cyst usually ruptures within a month.
Once ruptured, symptoms will gradually subside and no further treatment is necessary. If it doesn’t rupture spontaneously, surgery is sometimes performed to remove it. This will relieve the symptoms and prevent torsion.
A Ruptured Ovarian Cyst is a cyst that has ruptured and spilled its’ contents into the abdominal cavity.
If the cyst is small, its’ rupture usually occurs unnoticed. If large, or if there is associated bleeding from the torn edges of the cyst, then cyst rupture can be accompanied by pain. The pain is initially one-sided and then spreads to the entire pelvis. If there is a large enough spill of fluid or blood, the patient will complain of right shoulder pain.
Symptoms should resolve with rest alone. Rarely, surgery is necessary to stop continuing bleeding.
Torsion of an Ovarian Cyst occurs when the cyst twists on its’ vascular stalk, disrupting its’ blood supply. The cyst and ovary (and often a portion of the fallopian tube) die and necrose.
Patients with this problem complain of severe unilateral pain with signs of peritonitis (rebound tenderness, rigidity). This problem is often indistinguishable clinically
from a pelvic abscess or appendicitis, although an ultrasound or CT Scan can be helpful in making this distinction.
The Treatment is surgery to remove the necrotic adnexa. If surgery is unavailable, then bedrest, IV fluids and pain medication may result in a satisfactory, though prolonged, recovery. In this suboptimal, non-surgical setting, metabolic acidosis resulting from the tissue necrosis may be the most serious threat. Mortality rates from this condition (without surgery) are in the range of 20%.
An Endometrioma is a form of an ovarian cyst that results from ectopic endometrial tissue being present in the ovary. During the normal cyclic hormonal changes, this ectopic endometrium responds with proliferative growth, decidualization, and then sloughing, accompanied by bleeding. As the blood is trapped within the ovarian capsule or stroma, it gradually accumulates, forming a chronic hematoma, known as an endometrioma. If large enough, these masses can be found during an examination or identified on ultrasound.
The most troublesome aspect of endometriomas from a diagnostic standpoint is that they can mimic any of the ovarian neoplasms. Classically, the endometriomas have a ground-glass, slightly speckled appearance on sonar, but may demonstrate both cystic and solid components.
Ovarian Neoplasms vary in seriousness from annoying, to slowly growing, to aggressively invasive. Their clinical significance may not be related to their microscopic appearance. For example, Dermoid tumors, rarely malignant, are very threatening because of their tendency to twist on their vascular stalk, causing ovarian necrosis.
Ovarian neoplasms may be primarily cystic, solid, or mixed. Some are benign, some are malignant. Some produce enough hormone to cause symptoms for the patient.
Dermoid Tumors are common neoplasms that contain a variety of elements of dermal origin, including teeth, hair, sebaceous glands, and hormone-producing thyroid cells.
They are also called ovarian teratomas, are usually benign and occasionally malignant. Bilaterality is common.
Dermoids have several annoying features:
-
- They can rupture and spill their epithelial contents into the abdominal cavity where they may implant and grow, making later removal difficult.
- They may produce enough thyroid hormone to produce frank hyperthyrodism.
- They may twist on their vascular pedicles, causing necrosis, an acute abdomen, and the need for emergent surgical intervention.
Uterine Fibroid Tumors (Leiomyomas)
Typically, uterine fibroid tumors are easily identified within the uterus, both by clinical exam, and by such imaging studies as diagnostic ultrasound. Sometimes, uterine fibroids are growing in an area that cannot be distinguished from the adnexa. In these cases, the fibroids may appear to be a solid adnexal mass.
Ultrasound is usually but not always helpful in tracking the base of the fibroid back to the uterus. Occasionally, it will only be through surgical intervention that the source of this adnexal mass will become clear.
Ovarian Cancer
The life-time risk for a woman to develop ovarian cancer is about 1%, but varies with race, socioeconomic status, and continent. However, there are other factors that may increase or decrease that risk.
-
- Taking oral contraceptive pills decreases the risk of developing ovarian cancer, particularly if the OCPs have been taken for a long The initial reduction of risk of about 40% increases with increasing use.
- Pregnancy decreases the risk of ovarian A single full-term pregnancy lowers the risk by about 40%, and each subsequent pregnancy decreases it somewhat more.
- Having a tubal ligation or hysterectomy (with preservation of the ovaries) decreases the risk of ovarian cancer by about 50%.
- Removal of one ovary does not change the risk of later development of ovarian
- Using fertility-enhancing medications to stimulate ovulation may increase the risk of ovarian This risk is relatively small and not all studies agree that the risk increases.
- A family history of breast or ovarian cancer increases the patient’s risk of ovarian
- The presence of the BRCA1 or BRCA2 gene increases the lifetime risk of developing epithelial cell ovarian cancer to about one in
- The incidence of ovarian cancer steadily increases with age, peaking in the mid-60s. Ovarian cancer among younger women is rare. Prior to age 30, the incidence is 5/100,000.
Detection
Ovarian cancer can be difficult to detect. Unlike uterine cancer (that tends to cause visible bleeding at a relatively early stage), ovarian cancer usually remains symptomless until fairly late in the disease process. Symptoms associated with ovarian cancer include pelvic discomfort and bloating. Unfortunately, these symptoms are so non-specific as to be nearly useless in evaluating a patient for possible ovarian cancer. Further, by the time a patient develops these symptoms, the ovarian cancer has frequently spread to distant sites.
Blood tests are of limited value. Serum CA-125 increases in the presence of most ovarian epithelial cancers.
Unfortunately, it also increases in the presence of anything that irritates the peritoneal surface, including infection, endometriosis, ovulation, and trauma. Further limiting its usefulness has been the observation that by the time the serum CA-125 levels increase in response to ovarian cancer, it is no longer in its early stages.
Transvaginal ultrasound scanning has been used, with some success, to identify ovarian cancer. Ultrasonic findings that can be suspicious for ovarian cancer include unusually large amounts of free fluid in the abdominal cavity, solid ovarian enlargement, mixed cystic and solid enlargement of the ovaries, and thick- walled or complex ovarian cysts. Like CA-125, diagnostic ultrasound has some limitations to its usefulness.
By the time the macroscopic changes of ovarian cancer are detectable by ultrasound, most ovarian cancers are well beyond the early stage of the disease. Also, most abnormalities seen by ultrasound are not, in fact, cancer, but are benign findings that require no treatment.
For these reasons, most ultrasound screening programs for early detection of ovarian cancer have been discontinued. The vast majority of the abnormalities found (and surgically removed) actually required no treatment, and the few cancers that were successfully identified and removed were far enough advanced that it remained doubtful that the ultrasonic detection of them made any difference.
That said, using CA-125 and ultrasound (and CT scanning or MR imaging) to evaluate an adnexal mass can be helpful. Simple ovarian cysts are virtually never malignant, and observing more complex masses over time can distinguish between the many that are benign (corpus luteum cysts, for example), and the few that are malignant and growing.
Ovarian Cancer Management
Specific management of ovarian cancer hinges on the cell type (and grade), the extent of spread (stage), and sometimes may be modified by particular patient characteristics (such as a desire to preserve childbearing capacity).
The histologic evaluation requires a tissue specimen from the cancer that can be evaluated by the pathologist. For some ovarian cancer cell types, the histologic grade had prognostic significance (the more well-differentiated, the better). For other cell types, histologic grade has not been shown to have much of an independent prognostic value.
Staging of the cancer is usually accomplished at the time of surgery and takes into account the spread of the disease. Guidelines for staging come from the International Federation of Gynecology and Obstetrics (FIGO). Stages include:
-
- Stage I (Growth limited to the ovaries, and subdivided into Stage IA, IB, and IC, depending on the number of ovaries involved, presence or absence of ascites, tumor cells on the external surface of the ovaries or in peritoneal washings)
- Stage II (Growth beyond the ovaries, but limited to the Stage II is further subdivided into IIA, IIB, and IIC, depending on the specific areas of extension, presence of ascites, and tumor cells in peritoneal washings)
- Stage III (Growth out of the pelvis, but still within the epithelial surfaces of the abdominal cavity. This is subdivided into IIIA, IIIB, and IIIC, depending on the location of the growth and its location)
- Stage IV (Distant metastases outside the confines of the abdominal cavity or within the liver parenchyma).
The prognosis for early stage cancer of the ovary is generally good, the earlier the better. Unfortunately, not many Stage IA ovarian cancers are detected and treated. Most are of a more advanced stage where the prognosis is more guarded, the higher, the worse.
Surgical treatment options include local excision, TAH/BSO, and such debulking procedures as omentectomy and bowel resection. Even if the entire tumor cannot safely be removed surgically, reducing its bulk by at least 90% will often result in improved survival.
Depending on the cell type, radiotherapy and/or chemotherapy can also be used with good results. Occasionally, sub-optimal surgical treatment will be accepted as a compromise to enable other worthy goals. For example, an early ovarian cancer might optimally be treated with TAH/BSO, but instead, a simple oophorectomy is performed to preserve the woman’s childbearing capacity. In such a case, the woman must be prepared to accept the increased risk of treatment failure as the appropriate trade-off in retaining her capacity to have children.
Fallopian Tube Masses
Tubal ectopic pregnancy can present with an adnexal mass as either a primary or incidental finding. These masses can arise in two ways. If the ectopic pregnancy is large enough (and it must be quite large), then it may be found on physical examination or ultrasound exam.
Another commonly-found adnexal mass is the corpus luteum frequently found on the opposite side of the ectopic pregnancy. Ectopic pregnancy treatment options are many.
Pelvic inflammatory disease can sometimes lead to a fallopian tube abscess or a fluid-filled tube (hydrosalpinx). If large enough, this mass can be palpated on examination or seen on ultrasound. If asymptomatic, these masses are usually ignored. If they are causing significant symptoms, they are removed surgically.
Evaluation of the patient with an adnexal mass The primary goal of this evaluation is to distinguish those patients with an innocent, self-resolving mass from those who will need intervention to achieve the best results.
There are several Evaluation techniques that may prove useful.
-
-
You can Re-examine the patient after the next menstrual flow to see if the mass has disappeared.
-
You can perform an Exam under anesthesia if the normal exam is equivocal or difficult.
-
Pregnancy tests identify the presence of a pregnancy, Beta HCGs tell you whether the pregnancy is normal or not, and ultrasound scanning, combined with serial HCGs can determine the location of the pregnancy.
-
You can Have the patient use an enema to cleanse the lower bowel of stool and then re-examine the patient to see if the mass has disappeared.
-
A Pelvic ultrasound scan can identify the sonographic characteristics of the mass.
-
Serum CA-125 level will indicate if the peritoneal surface is being irritated
-
A CT scan (with contrast) of the abdomen and pelvis can be very helpful in identifying a non-gynecologic source for the mass, such as a pelvic kidney, diverticular abscess, or colon carcinoma.
-
Culdocentesis or paracentesis of ascitic fluid can be microscopically evaluated
-
You may elect to perform Laparoscopy to look directly at the pelvic mass, with possible laparoscopic removal
-
Or, a Laparotomy can be performed to explore the mass and remove it.
-
Duration 3:17
I was running one day again and I had
00:05
been getting slower and slower all year
00:06
long I knew something didn’t feel right
00:08
and I just felt a sort of this pain in
00:10
my abdomen but I just didn’t feel well
00:12
and then two weeks later my birthday in
00:16
June I was running with two friends and
00:19
I had to stop I just did not feel well
00:21
and I could feel it in my stomach and
00:23
then maybe a week later that that was a
00:26
we could just kind of was very
00:27
persistent and I just felt terrible and
00:30
then I figured I had to go make another
00:32
doctor appointment and I was diagnosed
00:34
with a hernia and so then I went to
00:38
another doctor who’s the hernia
00:40
specialist and he checked me out and
00:42
said you don’t have a hernia and I said
00:45
what do you think I have and he said I
00:47
don’t know and so my gut just said okay
00:49
I have to go back to my doctor and go
00:51
for an OB GYN exam and so I went back to
00:54
my doctor and she did an exam and after
00:57
that she called me back and said are you
01:01
driving which I was she said do you want
01:04
to pull over and I said no just tell me
01:05
what you have to tell me we have a list
01:08
of math there but they didn’t know what
01:10
it was she said I want you to go to
01:12
Roswell and she got me in right away and
01:14
I saw dr. Akers it was amazing and dr.
01:17
Akers
01:18
said okay yes there’s a mass it could be
01:21
something it could be nothing I won’t
01:25
know until I actually go in and biopsy
01:26
it and when I got here and had my
01:28
surgery it was something but very
01:31
luckily for me I was at stage 2 so she
01:34
did a complete hysterectomy took out
01:36
both ovaries and and the next week I
01:38
came in and saw dr. Akers and she said
01:40
well here are your options you can go
01:41
with no chemo I wouldn’t necessarily
01:43
recommend that you can go with
01:46
traditional chemo which would be just a
01:48
chest port or you can go with the IP
01:51
treatment and the chest port and it’s
01:54
most aggressive and she said it’s very
01:56
tough it’s brutal on your body and it is
01:59
but the day after I came home I saw my
02:02
friends walking by and I got off the
02:04
couch and they all helped me down the
02:07
steps and we took about four steps down
02:09
the driveway and then back off
02:11
and each day I’d walked a little further
02:13
so–but truly I mean quite literally got
02:16
me walking and I would see them every
02:18
day and it was you know what I would
02:20
look forward to and then that Monday
02:21
would feel good and Tuesday and have
02:22
chemo again and start all over anytime
02:25
there was a problem anytime I had the
02:26
allergic reactions they went okay we’re
02:29
gonna try this instead and I never felt
02:31
like I was not going to get through some
02:34
days I wasn’t thrilled about getting for
02:36
the chemo but I never thought I wasn’t
02:37
gonna get past it 18 weeks and then be
02:40
done and again I’ll never for a day take
02:42
for granted that I was lucky enough to
02:45
feel it because a lot of people don’t
02:46
feel it till it’s too late but usually
02:49
it comes back within one to two years
02:50
but dr. Akers told me because nurse was
02:53
caught early it didn’t spread you had
02:54
pretty aggressive chemo and you’re at
02:57
three years you’re already further along
02:58
in survivorship than most people on
03:01
earth I really I’m glad I came to rise
03:02
alive because I really from the person
03:06
who cleaned my room and after surgery
03:08
and to dr. Akers to everybody in between
03:11
everyone’s been amazing
03:14
[Music]
03:16
you
Duration 13:15
00:30
video is going to be last week I went to
00:33
the emergency room for ruptured ovarian
00:36
cysts
00:37
I actually had two ruptured cyst so I
00:40
think the most watched video on my
00:42
channel is my er story time from the
00:46
last time I had a ruptured cyst so why
00:49
not talk about it again this experience
00:51
was similar in some ways different in
00:54
other ways and I think it’s really
00:56
important to talk about this stuff I’ve
00:58
gotten so much good feedback on that
01:01
last video and if it would interest you
01:04
to watch that video as well I will put a
01:06
card that was my first experience having
01:08
anything so so severe this one I would
01:12
say was not precisely worse but just a
01:16
little bit different so let’s get right
01:19
into it just starting off I have been
01:22
under quite a lot of stress the last
01:25
couple months I’ve been traveling a bit
01:27
more than usual
01:28
that is definitely taken its toll on my
01:31
body my last two periods were very off
01:34
schedule my normal cycle is about 34 or
01:38
35 days my second to last period was
01:41
like 44 days or something I was like
01:43
where is it the following one was like
01:46
21 days last period was just terrible so
01:50
painful I had so much pain in my legs in
01:53
my rib cage I just had pain all over my
01:56
abdomen my last period what started on
01:59
March 9th and then by the time I think I
02:03
had the system the 21st I went to the
02:06
emergency room for I think it was the
02:07
21st between that time when I first got
02:10
my period all the way up until
02:12
I wound up in the emergency room I was
02:14
just in a lot of pain and it never
02:15
really went away like there were some
02:17
days where it was better and I was able
02:18
to like go for a walk and there were
02:21
other days where it was just so bad I
02:23
basically really wasn’t doing very much
02:25
cut to about four or five days before I
02:28
went to the emergency room I had a lot
02:30
of pain on one side on my left side
02:34
I wasn’t sure maybe this is just
02:36
digestive pain what’s frustrating about
02:39
having ovarian cysts and digestive
02:42
issues is you kind of never know what it
02:44
is because everything’s really in the
02:46
same area like it’s very hard to tell
02:48
what’s going on and it wasn’t clearly
02:51
like sometimes you have that real clear
02:53
ovulation middle shmurda pain it really
02:57
wasn’t that sort of fuzzy it was like a
02:59
dull achy pain and that kind of passed
03:02
and I was able to be a little bit active
03:05
the day before I went to the emergency
03:07
room was Sunday I actually went to the
03:10
gym I did some light weight lifting
03:12
walked in the treadmill I went to yoga
03:14
class and I felt pretty good I was
03:17
fatigued and I was sort of pushing
03:19
through I was pushing myself a little
03:21
bit but nothing too strenuous really at
03:24
all Sunday night the pain started to get
03:27
worse and it was sort of all over my
03:30
abdomen it was on both sides which was
03:32
really strange it had been really
03:34
concentrated on the left side for a few
03:36
days and then it was sort of on the
03:38
right side as well
03:39
that really confused me because
03:41
generally cystic pain or ovulation pain
03:44
is gonna be one side only and it might
03:47
rady but generally it’s gonna be in the
03:49
one side the other thing was that I had
03:51
pain on one side of my back a very dull
03:54
achy pain and I was like is this my
03:56
kidney I had a little bit of urinary
03:59
symptoms but nothing to write home about
04:02
there so then I woke up Monday morning
04:05
and I was still in a lot of pain the
04:07
pain had actually shifted over to the
04:09
right side it had been in the left side
04:11
for a few days and just feeling mmm not
04:16
good so I knew I needed to see the
04:19
doctor I still at that point didn’t even
04:21
know if maybe the
04:22
was a digestive problem I wasn’t really
04:24
having any digestive symptoms actually
04:26
my digestion was much better than it
04:29
normally is yeah I was like should I go
04:31
to my family doctor or should I go to my
04:34
gynecologist and I really didn’t know I
04:37
was like let me just go to my
04:39
gynecologist so my normal doctor wasn’t
04:42
available I think he was off delivering
04:44
babies or something I saw a family nurse
04:46
practitioner in the same practice she
04:48
did an internal examination and with
04:51
pressing on my belly and the only part
04:55
that was really tender and painful when
04:57
she did that was actually my bladder
04:59
when she pressed on my ovaries didn’t
05:01
really hurt at all and that was very
05:04
surprising so I had to pee in a cup and
05:06
that was fine no infection so she said
05:10
well it’s probably a cyst
05:12
I’ll schedule an ultrasound for Thursday
05:14
and then I’ll see you next week
05:16
just take Advil you’ll be fine that was
05:19
first thing in the morning about 9
05:21
o’clock or so and I went home I did a
05:23
little work sat in my office and I just
05:26
the pain became on bearable I just
05:30
couldn’t I had no position I could get
05:32
comfortable and Advil really didn’t do
05:34
anything at all the one thing that I
05:37
would say was really consistent with the
05:39
last time I had a cyst was peeing was so
05:44
painful so so so painful to the point
05:48
where I really felt like I was gonna
05:50
pass out from the pain and so I just
05:52
didn’t drink a lot of water because I
05:54
just couldn’t even bear the thought of
05:56
peeing that’s how painful it was so I
05:58
was just feeling worse and worse and I
06:00
am a person who has a lot of like
06:01
medical anxiety so I was just saying to
06:05
myself I don’t want to miss something I
06:06
don’t want to wait till tomorrow to go
06:08
back to the doctor it was about five
06:10
o’clock I made the decision to go over
06:14
to the emergency room I was fine enough
06:16
to drive but I was feeling pretty
06:17
anxious I you know again I was like if
06:20
it’s my appendix or something a B it’s
06:23
my kidney maybe I have a kidney stone or
06:26
kidney infection you know if it is my
06:28
ovary generally over ovarian cysts just
06:31
heal on their own they don’t require any
06:34
intervention at all but there are two
06:37
cases where they would one is a dermoid
06:40
cyst you might want to cover your ears
06:42
if you’re a sensitive person but
06:44
basically it’s one assist grows hair and
06:47
teeth an egg contains stem cells so it
06:51
can actually form any kind of tissue
06:53
those do need to be removed surgically
06:55
and I think it’s like 10% of cysts or
06:58
something the other thing would be a
07:00
cyst that’s so large that it can cause
07:03
the ovary to twist on its stem and
07:05
that’s a medical emergency because the
07:07
ovary will die and the tissue will
07:10
become necrotic you know I’m a person
07:12
who really likes to stay out of the
07:14
emergency room first of all it’s
07:16
crawling with germs but there are some
07:18
things that I think do require emergency
07:21
attention and I felt like this qualified
07:24
for that so I went over to the emergency
07:26
room got triage like pretty quickly all
07:29
my vitals were normal heart rate blood
07:31
pressure all that stuff so that’s
07:32
reassuring and then I waited in the
07:34
waiting room for about two hours
07:36
I got seen by a doctor probably within
07:39
five minutes of getting a bed which was
07:40
great he ordered an ultrasound I was
07:43
getting an ultrasound probably within
07:45
about 2 and 1/2 hours of walking into
07:47
the emergency room which was not bad at
07:49
all an ultrasound confirmed that I had
07:52
not one but two ruptured cysts I had one
07:56
ruptured on the left that had ruptured
07:58
probably about four or five days before
08:00
and they could tell it had like deflated
08:03
and there was fluid had leaked out of it
08:07
a cyst that had ruptured on the right
08:09
probably that earlier that day and there
08:13
was like fresh fluid leaking out of
08:15
there as well and then I had one other
08:17
large cyst on my left as well so I had
08:21
three cysts I think the largest one was
08:24
four centimeters once I had the
08:26
diagnosis I felt so much better I felt
08:30
no matter how much pain it is I know
08:32
it’s not dangerous I know my body will
08:34
take care of it it was just such a
08:36
weight off my shoulders so I felt so
08:41
relieved and so glad part two of the
08:44
tale is that while I was in the
08:47
emergency
08:48
I told them I rated my pain between a
08:50
seven and an eight and they asked me if
08:53
I wanted medication for the pain I had
08:55
remembered from the last experience of
08:58
having dilaudid which is a very strong
09:02
narcotic how amazing that was and just
09:06
how great I felt they offered me
09:08
dilaudid again this time it was awful it
09:13
was a complete nightmare experience if I
09:17
could take it back I fully would have it
09:19
was so so so bad I had it along with
09:23
some zofran I hadn’t eaten in about six
09:26
hours before then I’d had no IV fluids
09:29
just straight on an empty stomach this
09:32
very strong narcotic talking twice as
09:35
strong as morphine my main symptom was
09:38
just extremely Ness and that lasted for
09:42
I would say a solid two hours so it was
09:45
an absolute nightmare
09:46
it did relieve my pain I guess but I was
09:49
just so focused on how bad I felt
09:52
otherwise that it didn’t even really
09:55
matter so if I could do that part of it
09:56
over again I would have probably just
09:58
asked for an Advil or something not
10:01
quite so strong the other time I had it
10:04
it was like the greatest thing on earth
10:06
this time it was the worst possible
10:09
nightmare so I had to actually stay in
10:11
the emergency room for a little while
10:12
longer and have them monitor me on that
10:15
the other thing that I had that was an
10:18
issue with it was like my whole neck and
10:21
back it’s just completely seized up
10:24
almost like just it was such it was such
10:26
a terrible terrible feeling so start to
10:29
finish I was in the emergency room for
10:31
about six hours I got home and paced
10:34
around for probably about half an hour I
10:36
actually called the emergency room and
10:38
called the doctor and was like is this
10:40
normal I really feel so so so bad and he
10:43
was a little impatient he was like yeah
10:45
you’re fine go to bed but I did feel
10:47
when I went to sleep that I was just
10:49
gonna stop breathing
10:50
like I was probably taking three breaths
10:52
a minute or something like I was just
10:55
ridiculous I woke up a few hours later
10:57
my pain was back in full force it was
11:00
even worse but
11:01
least the effects of the dilaudid had
11:03
worn off that’s pretty much the story I
11:06
have a few little clips I did make some
11:09
Instagram stories I put all my deepest
11:12
darkest secrets on Instagram keep that
11:14
stuff off YouTube where things live
11:15
forever
11:16
I like the ephemeral Ness of Instagram
11:18
but I did save a few stories so I’m
11:20
going to post those at the end of this
11:22
video I just want to invite you to stick
11:24
around because I will be posting some
11:26
vlogs from the few days after and my
11:30
recovery with the ovarian cysts and then
11:32
whatever is happening going forward with
11:34
it and that’s pretty much it so if you
11:38
enjoyed this video if you found this
11:40
helpful please give it a thumbs up that
11:41
really helps me out so much feel free to
11:43
leave a comment below I think it’s so
11:46
valuable that we have this medium to
11:49
connect with each other I actually know
11:51
a few people in real life that this has
11:53
happened too but I get to meet so many
11:55
people through the internet who we can
11:58
relate and share these crazy stories so
12:01
I definitely would love to hear from you
12:03
in the comments below feel free to stick
12:05
around subscribe and stay tuned for more
12:08
vlogs of my life and health and this
12:12
whole journey thank you so much for
12:15
watching and I will catch up with you
12:17
guys next time
12:17
hey friends so I’m still in the ER
12:20
getting ready to leave pretty soon I’m
12:24
just waiting up my blood work and three
12:28
cyst on my ovary is part two of the
12:32
story is that they gave me dilaudid for
12:35
the pain for the last hour I’ve just
12:38
been so dizzy kind of took one problem
12:43
and made it into a completely other
12:45
bigger profit
12:47
ratings from my bathroom I think I might
12:52
sleep down here tonight my face feels
12:55
like it’s two sizes too small for my
12:58
face I feel so bad I obviously don’t
13:02
feel like myself I feel so weird and
13:06
dizzy and I feel like if I go to sleep
13:08
we’re gonna stop breathing so it’s like
13:10
3:00 a.m. my
13:13
Davo no pain is back and it seems to be
13:16
a lot worse that was only seven hours
13:20
ago that I had the medication so I don’t
13:23
think that roller coaster was worth the
13:25
price of image so I will just reiterate
13:27
I said earlier don’t do drugs seriously
13:32
if you can there’s an alternative