Duration 10:17
Sexually Transmitted Infections
Plummer XD, Liang A
Clinical Case Applicability: pelvic inflammatory disease, infertility, chronic pelvic pain
Learning Objectives:
1. Understand the pathophysiology of common STIs
2. Describe the long-term sequelae of STIs
3. Understand the mechanism of action for treatment of common STIs
What is the pathophysiology of infectivity & treatment of these organisms? (HPV: see CIN script)
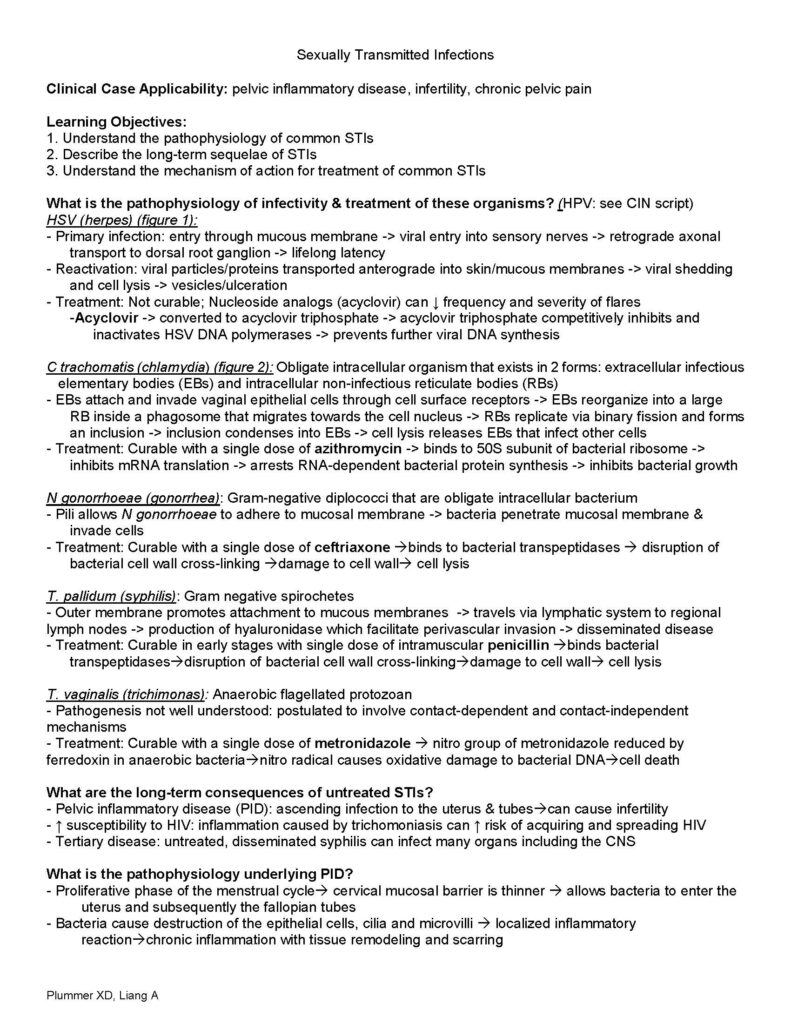
HSV (herpes) (figure 1):
– Primary infection: entry through mucous membrane -> viral entry into sensory nerves -> retrograde axonal transport to dorsal root ganglion -> lifelong latency
– Reactivation: viral particles/proteins transported anterograde into skin/mucous membranes -> viral shedding and cell lysis -> vesicles/ulceration
– Treatment: Not curable; Nucleoside analogs (acyclovir) can ↓ frequency and severity of flares
–Acyclovir -> converted to acyclovir triphosphate -> acyclovir triphosphate competitively inhibits and inactivates HSV DNA polymerases -> prevents further viral DNA synthesis
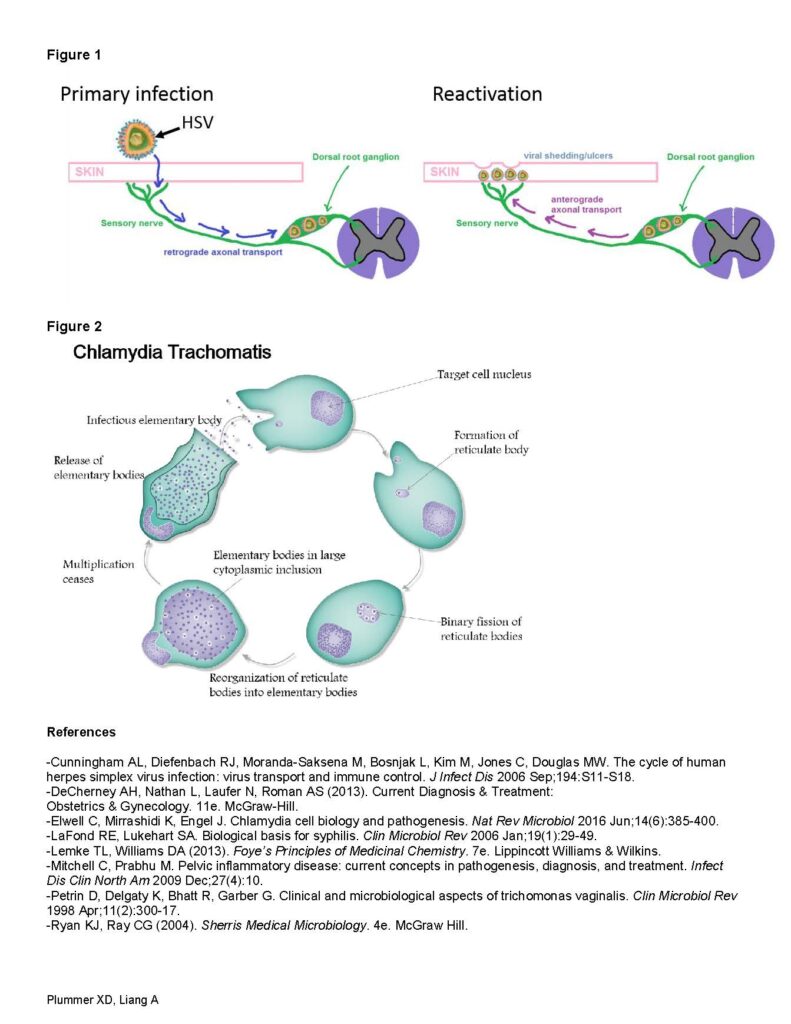
C trachomatis (chlamydia) (figure 2): Obligate intracellular organism that exists in 2 forms: extracellular infectious elementary bodies (EBs) and intracellular non-infectious reticulate bodies (RBs)
– EBs attach and invade vaginal epithelial cells through cell surface receptors -> EBs reorganize into a large RB inside a phagosome that migrates towards the cell nucleus -> RBs replicate via binary fission and forms an inclusion -> inclusion condenses into EBs -> cell lysis releases EBs that infect other cells
– Treatment: Curable with a single dose of azithromycin -> binds to 50S subunit of bacterial ribosome -> inhibits mRNA translation -> arrests RNA-dependent bacterial protein synthesis -> inhibits bacterial growth
N gonorrhoeae (gonorrhea): Gram-negative diplococci that are obligate intracellular bacterium
– Pili allows N gonorrhoeae to adhere to mucosal membrane -> bacteria penetrate mucosal membrane & invade cells
– Treatment: Curable with a single dose of ceftriaxone binds to bacterial transpeptidases disruption of bacterial cell wall cross-linking damage to cell wall cell lysis
T. pallidum (syphilis): Gram negative spirochetes
– Outer membrane promotes attachment to mucous membranes -> travels via lymphatic system to regional lymph nodes -> production of hyaluronidase which facilitate perivascular invasion -> disseminated disease
– Treatment: Curable in early stages with single dose of intramuscular penicillin binds bacterial transpeptidasesdisruption of bacterial cell wall cross-linkingdamage to cell wall cell lysis
T. vaginalis (trichimonas): Anaerobic flagellated protozoan
– Pathogenesis not well understood: postulated to involve contact-dependent and contact-independent mechanisms
– Treatment: Curable with a single dose of metronidazole nitro group of metronidazole reduced by ferredoxin in anaerobic bacterianitro radical causes oxidative damage to bacterial DNAcell death
What are the long-term consequences of untreated STIs?
– Pelvic inflammatory disease (PID): ascending infection to the uterus & tubescan cause infertility
– ↑ susceptibility to HIV: inflammation caused by trichomoniasis can ↑ risk of acquiring and spreading HIV
– Tertiary disease: untreated, disseminated syphilis can infect many organs including the CNS
What is the pathophysiology underlying PID?
– Proliferative phase of the menstrual cycle cervical mucosal barrier is thinner allows bacteria to enter the uterus and subsequently the fallopian tubes
– Bacteria cause destruction of the epithelial cells, cilia and microvilli localized inflammatory reactionchronic inflammation with tissue remodeling and scarring Plummer XD, Liang A
Figure 1
Figure 2
References
-Cunningham AL, Diefenbach RJ, Moranda-Saksena M, Bosnjak L, Kim M, Jones C, Douglas MW. The cycle of human herpes simplex virus infection: virus transport and immune control. J Infect Dis 2006 Sep;194:S11-S18.
-DeCherney AH, Nathan L, Laufer N, Roman AS (2013). Current Diagnosis & Treatment:
Obstetrics & Gynecology. 11e. McGraw-Hill.
-Elwell C, Mirrashidi K, Engel J. Chlamydia cell biology and pathogenesis. Nat Rev Microbiol 2016 Jun;14(6):385-400.
-LaFond RE, Lukehart SA. Biological basis for syphilis. Clin Microbiol Rev 2006 Jan;19(1):29-49.
-Lemke TL, Williams DA (2013). Foye’s Principles of Medicinal Chemistry. 7e. Lippincott Williams & Wilkins.
-Mitchell C, Prabhu M. Pelvic inflammatory disease: current concepts in pathogenesis, diagnosis, and treatment. Infect Dis Clin North Am 2009 Dec;27(4):10.
-Petrin D, Delgaty K, Bhatt R, Garber G. Clinical and microbiological aspects of trichomonas vaginalis. Clin Microbiol Rev 1998 Apr;11(2):300-17.
-Ryan KJ, Ray CG (2004). Sherris Medical Microbiology. 4e. McGraw Hill.
Duration 11:33
00:00
This VAP is on vagina discharge.
00:03
00:07
By the end of this VAP,
00:08
[AUDIO OUT]
00:09
00:21
The normal vaginal environment
00:22
is acidic, with a pH of 3.8
00:25
to 4.4, thus discouraging
00:27
infections.
00:29
This environment is created
00:30
by normally occurring bacteria,
00:31
lactobacilli.
00:34
Any disruption to the pH balance
00:36
of the vaginal environment
00:37
can make it more
00:38
conducive to infection.
00:40
Physiological vaginal discharge
00:42
is normal and consists
00:44
of vaginal secretions.
00:46
Contribution
00:46
to vaginal secretions
00:47
include secretions
00:49
from sebaceous, sweat, Bartholin
00:52
and Skene glands,
00:53
transudate
00:54
from the vaginal wall,
00:55
exfoliated vaginal and cervical
00:58
cells, cervical mucus,
01:00
endometrial and oviductal fluid.
01:03
Physiological discharge is also
01:05
influenced by hormone levels.
01:07
The pH balance of the vagina
01:09
is the least acidic on the days
01:11
just prior
01:11
to and during menstruation.
01:14
Infections are thus most common
01:15
at this time.
01:17
There is also a normal increase
01:19
of discharge around mid-cycle.
01:22
Pregnancy also increases
01:23
physiological discharge.
01:24
01:28
Vaginal discharge can be
01:29
either physiological or
01:31
pathological.
01:32
Pathological causes can be
01:34
further divided
01:35
into infective or non-infective
01:37
causes.
01:38
The commonest cause
01:39
is physiological,
01:41
but infective causes should be
01:42
excluded.
01:44
We will be focusing
01:44
on the major common causes
01:46
of infective vaginal discharge–
01:48
namely bacterial vaginosis,
01:51
vulvovaginal candidiasis,
01:53
and trichomonas vaginalis.
01:54
01:58
The following diagnostic
01:59
approach is recommended.
02:01
First, a thorough history must
02:03
be obtained.
02:04
Details
02:05
about the vaginal discharge
02:06
include the onset, duration,
02:09
color, and odor.
02:11
Associated symptoms
02:12
such as vaginal itch, rash,
02:14
and dysuria
02:15
are
02:16
suggestive of infective vaginal
02:18
discharge.
02:19
A sexual history is used
02:21
to assess the risk of STIs.
02:24
Risk factors include age less
02:26
than 25 years,
02:27
change of new sexual partner
02:29
in the last year,
02:30
and more than one sexual partner
02:32
in the last year.
02:33
Similar symptoms in partners
02:35
should be covered.
02:37
Medical history is important
02:38
as immunocompromised states
02:40
like diabetes and HIV
02:42
can predispose to infection.
02:44
Current and previous medication,
02:46
menstrual history,
02:47
and obstetric history
02:49
should be obtained, too.
02:51
Next, perform
02:53
a physical examination,
02:54
inspection
02:55
of the external genitalia
02:57
and perianal areas
02:59
are done to look
02:59
for inflammation and other
03:01
lesions.
03:02
A speculum examination allows
03:04
one to inspect
03:05
the vaginal and cervical region.
03:08
Attention to the appearance
03:09
and character of discharge
03:10
is important, including
03:12
the consistency and odor.
03:16
Not all women
03:17
with vaginal discharge
03:18
require investigations.
03:20
Empirical treatment can be given
03:22
if the patient is at low risk
03:23
of STI and has no symptoms
03:26
to suggest upper genital tract
03:27
infection.
03:29
The description
03:30
in the top right blue box
03:32
gives a clue
03:33
as to the potential infection.
03:36
Investigations are indicated
03:37
if a woman is at high risk
03:39
of STIs, has symptoms suggestive
03:42
of upper genital tract
03:44
infection– for example,
03:46
abdominal pain, dyspareunia,
03:49
or fever, has previous treatment
03:51
which has failed, is post-natal,
03:54
post-miscarriage,
03:55
or post-abortion,
03:57
but is within three weeks
03:58
of insertion
03:59
of an intrauterine contraceptive
04:01
device.
04:03
Investigations include
04:04
high vaginal swabs, which are
04:06
used to diagnose a common cause
04:08
such as candida,
04:09
bacterial vaginosis,
04:11
and trichomonas.
04:13
Endocervical swabs are used
04:15
to diagnose certain sexually
04:16
transmitted diseases
04:18
like chlamydia and gonorrhea.
04:20
04:23
Bacterial vaginosis is the most
04:25
common cause
04:26
of vaginal discharge in women
04:27
of reproductive age.
04:29
However, up to 50%
04:31
of women
04:31
with a clinical diagnosis of BV
04:33
are asymptomatic.
04:36
BV is due to an overgrowth
04:37
of organisms.
04:38
This occurs when there is
04:39
an alteration
04:40
of normal vaginal flora,
04:42
causing a loss of lactobacilli,
04:44
thus disrupting the pH balance
04:46
of the vaginal environment
04:47
and increasing the pH.
04:50
The organisms responsible
04:51
are predominantly anaerobic,
04:53
and include Gardnerella
04:55
vaginalis, Mycoplasma hominis,
04:57
and Mobiluncus.
04:59
An isolation of Gardnerella
05:01
vaginalis alone should not
05:03
be used as a diagnostic test
05:04
for BV, as between 35% to 55%
05:07
of women
05:08
are carriers of this organism.
05:11
Predisposing factors include
05:13
repeated alkalinization
05:14
of the vagina– for example,
05:16
douching
05:17
and frequent sexual intercourse.
05:20
BV increases the risk
05:21
of post-abortion endometritis
05:23
and pelvic inflammatory disease.
05:26
In pregnancy, it is associated
05:28
with late miscarriage, preterm
05:30
delivery
05:31
in high-risk pregnancies,
05:33
preterm premature rupture
05:34
of membranes,
05:35
and postpartum endometritis.
05:36
05:40
BV is usually diagnosed using
05:42
Amsel’s criteria,
05:43
where at least three
05:44
of the following four conditions
05:46
must be met.
05:48
Number one, a raised vaginal pH
05:50
of more than 4.5; number two,
05:53
thin, homogenous grey or white
05:55
vaginal discharge; number three,
05:58
the presence of clue cells
06:00
on wet preparation microscopy;
06:02
and number four, a positive
06:04
amine test demonstrated
06:05
by the release of the fishy odor
06:07
on mixing vaginal discharge with
06:09
10% potassium hydroxide.
06:11
Organisms are cultured
06:13
from a high vaginal swab
06:14
for diagnosis.
06:14
06:18
All symptomatic women
06:19
with bacterial vaginosis
06:21
or asymptomatic women with BV
06:23
before surgical procedures
06:25
should be treated.
06:27
BV can be treated
06:28
with either oral Metronidazole
06:30
or Clindamycin for seven days.
06:33
Treatment in pregnancy
06:34
is the same as
06:35
in non-pregnant women.
06:37
Overall cure rates range
06:38
from 75% to 85% and followup is
06:41
not necessary if symptoms
06:43
resolve.
06:44
Recurring BV occurs within three
06:46
months of treatment in about 15%
06:49
of women.
06:50
Suppressive regimens may be
06:52
considered, but evidence
06:53
to support their effectiveness
06:55
is limited.
06:56
Maintenance
06:57
with acetic acid vaginal gel
06:59
at the time of menstruation
07:01
and following unprotected
07:02
sexual intercourse maintains
07:04
acidic vaginal pH.
07:05
07:08
Candidiasis is
07:09
a fungal infection mostly caused
07:11
by the species Candida albicans.
07:15
Candida albicans
07:16
is responsible for 80% to 92%
07:18
of cases.
07:20
Other species of Candida
07:21
such as Candida glabrata
07:23
and Candida tropicalis
07:24
tend to be resistant to therapy.
07:27
Predisposing factors
07:28
to infection
07:29
include immunosuppression,
07:32
antibiotic use, high estrogen
07:34
levels that occur
07:35
with oral contraceptive pills
07:37
and hormone replacement therapy
07:39
usage, pregnancy, diabetes
07:42
mellitus, and prolonged
07:43
corticosteriod therapy.
07:45
07:48
Typical Candida infection
07:50
presents
07:50
with thick, white, curdy cottage
07:52
cheese-like discharge
07:54
associated with vaginal itch
07:56
and soreness.
07:57
Occasionally, it can be
07:59
associated
07:59
with superficial dyspareunia
08:02
or external dysuria.
08:04
Clinically,
08:05
vulvovaginal erythema
08:07
and excoriation is common.
08:09
The high vaginal swab is used
08:11
for diagnosis.
08:12
Yeast cells are seen on gram
08:14
stain microscopy.
08:15
08:18
There are various preparations
08:20
of drugs that can be used
08:21
for treatment.
08:22
All topical and oral azole
08:24
therapies give a cure rate
08:26
of 80% to 90%.
08:28
In pregnancy,
08:29
asymptomatic colonization
08:31
with Candida is common at 30%
08:33
to 40%.
08:35
No treatment is necessary,
08:37
unless patients are symptomatic.
08:39
Oral azole is contraindicated
08:42
and should not be used
08:42
in pregnancy.
08:44
Longer courses of topical azole
08:46
for 7 days is recommended
08:48
instead.
08:49
Nystatin preparations have a 70%
08:51
to 90% cure rate.
08:53
They are the first line
08:54
treatment
08:55
for non-albicans infection.
08:58
Patients should avoid
08:59
local irritants
09:00
such as tight clothing
09:02
or perfumed vaginal douche.
09:04
Topical creams or antihistamines
09:06
can be used to relieve itch.
09:08
09:11
Recurrent infection is defined
09:13
as four or more episodes
09:15
of symptomatic infection
09:16
annually,
09:17
with positive microscopy
09:18
of Candida on at least two
09:20
episodes.
09:21
For acute treatment
09:23
of the infection, an induction
09:24
regimen of oral azole
09:26
is repeated every three days
09:27
for three doses.
09:29
Following that, [INAUDIBLE]
09:30
maintenance regimen is used
09:32
for six months.
09:33
09:35
Trichomonal vaginitis is caused
09:38
by the parasite Trichomonas
09:40
vaginalis.
09:41
It is
09:41
the only sexually transmitted
09:43
vaginal infection of the three
09:45
infections discussed.
09:47
However, unlike chlamydia
09:49
and gonorrhea, it does not
09:51
affect extragenital sites,
09:53
but can infect the vagina,
09:54
urethra, and periurethral
09:56
[INAUDIBLE].
09:58
Partners in the last two months
09:59
should be screened and treated.
10:01
Testing for other sections
10:03
including BV and other STIs
10:05
should be considered,
10:06
as 60% of patients
10:08
have BV and 30%
10:09
have chlamydia or gonorrhea.
10:12
The graph shows
10:13
the concurrent STIs found
10:14
in a survey of women
10:15
with a Trichomonas infection.
10:17
10:20
Clinical diagnosis is typically
10:22
identified
10:23
by a yellow green foul-smelling
10:24
discharge associated
10:26
with vulvovaginal erythema
10:28
and excoriation
10:29
with a “strawberry cervix”
10:31
presenting in 2% of patients.
10:33
Investigations will review
10:35
a raised pH
10:36
with motile trichomonads seen
10:38
on microscopy.
10:39
10:42
First line treatment requires
10:44
systemic rather than
10:45
topical treatment,
10:46
because the infection is not
10:47
always confined to the vagina
10:49
but may involve other parts
10:50
of urogenital tract.
10:53
Oral Metronidazole for one week
10:55
gives a cure rate of 90% to 95%,
10:57
compared to 50%
10:59
with topical treatment.
11:01
Patients
11:02
with persistent symptoms
11:03
should be retreated
11:04
with oral Metronidazole 400 mg
11:06
b.i.d.
11:07
for another seven days.
11:09
Repeated failure of treatment
11:10
may require high dose
11:12
oral Metronidazole of two grams
11:13
daily for three days.
11:15
Sexual partners should also
11:17
be treated as this will improve
11:18
cure rates.
11:19
11:22
This is the end of the VAP.
11:24
Further reading references are
11:25
as stated.
Duration 6:55
Welcome.
00:02
Today, we will review
00:03
pelvic inflammatory disease.
00:05
00:08
Our objective today will be
00:09
to briefly review
00:10
the definition, epidemiology,
00:12
and pathogenesis
00:13
of pelvic inflammatory disease,
00:16
which I will refer to as PID
00:18
in this presentation.
00:19
We’ll review
00:20
the important long term sequelae
00:22
associated with PID
00:24
that makes it
00:24
such a public health concern.
00:26
We will also discuss diagnosis
00:28
and first line treatment
00:29
for PID.
00:30
00:33
Here is an outline
00:34
of the presentation today.
00:36
00:42
Pelvic inflammatory disease
00:44
is a spectrum
00:45
of inflammatory disorders
00:46
of the upper female genital
00:48
tract, which includes
00:49
the uterus, fallopian tubes,
00:51
and ovaries.
00:52
It is believed to be caused
00:54
by ascending spread
00:55
of microorganisms
00:56
from the vagina
00:57
to the cervix, endometrium,
00:59
fallopian tubes,
01:00
and/or adjacent structures.
01:02
01:05
The rate of PID in the United
01:07
States population has gone down
01:09
over the last 10 to 20 years.
01:11
Most likely, this
01:12
is due to the use
01:13
of prophylactic antibiotics
01:15
prior to surgical procedures,
01:17
routine screening of high risk
01:18
populations for sexually
01:20
transmitted infection,
01:21
and to the use of antibiotics
01:23
early in patients in which lower
01:25
genital infections,
01:26
such as cervicitis,
01:27
is suspected.
01:28
01:31
PID it’s
01:32
a polymicrobial infection.
01:35
The most common bacteria
01:36
isolated in cases of PID
01:38
are anaerobic bacteria,
01:40
chlamydia trarchomatis,
01:42
and neisseria gonorrhea.
01:43
01:46
Certain high risk populations
01:48
should be watched closely
01:49
for evidence of PID.
01:51
In particular, sexually active
01:53
young women, patients attending
01:54
sexually transmitted disease
01:56
clinics, and patients who live
01:57
in other settings
01:58
where there are high rates
01:59
of gonorrhea or chlamydia
02:01
are at risk.
02:02
02:05
A clinical diagnosis
02:06
of symptomatic PID
02:08
has a positive predictive value
02:10
at 65% and 90%,
02:12
compared with laparoscopy, which
02:14
is thought to be
02:14
the gold standard for diagnosis
02:17
based on early studies.
02:19
Today, the diagnosis of PID
02:21
is primarily made using
02:22
this clinical criteria.
02:24
Of note, the diagnosis of PID
02:27
requires ruling out other causes
02:29
of abdominal pain,
02:30
such as appendicitis,
02:32
ectopic pregnancy,
02:33
or other surgical emergencies.
02:36
Treatment should be initiated
02:37
if patients have at least one
02:38
of the minimum criteria listed
02:40
here,
02:41
which are cervical motion
02:42
tenderness, uterine,
02:43
or adnexal tenderness.
02:45
Further work
02:46
up for alternative etiology
02:47
of pain should not delay
02:48
treatment.
02:50
According to the Center
02:51
for Disease Control
02:52
and Prevention, other criteria
02:54
that may increase
02:55
your specificity
02:56
for the diagnosis of PID
02:58
include fever,
02:59
mucopurulent vaginal discharge,
03:02
numerous white blood cells
03:04
on a wet mount, and/or detection
03:06
of gonorrhea or chlamydia.
03:08
The most specific tests
03:10
for diagnosis
03:11
include endometrial biopsy,
03:13
ultrasound evidence
03:14
of tubo-ovarian abscess,
03:16
and/or diagnostic laparoscopy.
03:19
However, due to the increased
03:21
risk of long term morbidity
03:23
associated with failing to treat
03:24
a patient with PID,
03:26
it is recommended
03:27
that a high level
03:27
of clinical suspicion
03:29
be maintained
03:29
and that patients
03:30
with minimum criteria
03:31
be empirically treated early.
03:33
03:36
In the short term, treatment
03:38
is aimed
03:39
at clinical and microbiologic
03:41
cure.
03:42
This can be reliably achieved
03:43
with antibiotic regimens,
03:45
as described
03:46
on the next few slides.
03:48
Less is known about the effect
03:49
of current regimens
03:50
on long term outcomes.
03:52
However, it is thought
03:53
that by early detection
03:55
and treatment of PID,
03:56
it is possible to decrease
03:58
the rates of infertility,
03:59
ectopic pregnancy,
04:01
recurrent infection,
04:02
and chronic pelvic pain
04:03
that can be the long term
04:04
sequelae.
04:05
04:08
Certain patients are candidates
04:10
for outpatient treatment
04:11
in the setting of PID,
04:13
and there does not appear to be
04:14
any benefit of inpatient
04:15
over outpatient therapy
04:17
if they meet criteria
04:18
for outpatient management.
04:20
Appropriate regimens should
04:21
empirically cover gonorrhea
04:23
and chlamydia.
04:24
If the clinical picture is
04:25
concerning
04:26
for anaerobic infection–
04:27
for instance,
04:28
if bacterial vaginosis is
04:29
detected– then consideration
04:31
may be given to adding
04:33
an antibiotic with broader
04:34
anaeorbic coverage,
04:35
such as Metronidazole.
04:36
04:39
Certain populations will require
04:41
closer monitoring
04:42
and in patient parenteral
04:43
therapy.
04:44
These include patients who are
04:46
pregnant, those in whom
04:48
a surgical emergency may
04:49
be suspected,
04:50
such as appendicitis, patients
04:52
who have not responded
04:53
to oral medications
04:55
or are unable to tolerate
04:56
outpatient oral regimen, those
04:58
who demonstrate
04:59
other signs of severe illness,
05:00
or have radiologic findings
05:02
concerning
05:03
for a tubo-ovarian abscess.
05:04
05:07
Per the Center for Disease
05:09
Control, the recommended
05:10
first line treatment
05:11
includes a cephalosporin
05:12
with broader anaerobic coverage,
05:14
such Cefotetan or Cefotxitin,
05:16
with Doxycycline for a total
05:18
of 14 days.
05:19
After clinical symptoms improve,
05:21
patients may continue
05:22
Doxycycline
05:23
with or without Metronidazole
05:25
for a total of 14 days.
05:27
There are many alternatives
05:28
to this regimen, and there’s
05:29
limited evidence
05:30
that any regimen is better
05:31
than the other.
05:32
05:35
Whether patients are treated
05:36
as inpatients or outpatients,
05:38
the patient should be followed
05:40
closely and clinical improvement
05:42
should be seen within three days
05:43
of initiation of therapy.
05:45
Repeat testing and completion
05:47
of screening for any sexually
05:48
transmitted diseases
05:49
within three to six months
05:50
should be performed.
05:52
Patients
05:52
with pelvic inflammatory disease
05:54
are at high risk of recurrence.
05:56
All patients diagnosed
05:57
with gonorrhea and/or chlamydia
05:59
should also have testing
06:00
in treatment
06:00
of their sexual partners.
06:01
06:05
In summary, pelvic inflammatory
06:07
disease
06:08
is a polymicrobial disease
06:09
with significant public health
06:10
implications,
06:11
including increased risk
06:13
of ectopic pregnancy,
06:14
infertility,
06:15
and chronic pelvic pain.
06:17
Early detection
06:18
and effective treatment
06:19
is required to decrease
06:21
long terms sequelae.
06:22
Evidence suggests
06:23
that outpatient oral therapy is
06:25
equally effective for treatment
06:27
of mild
06:27
to moderate PID
06:29
as inpatient parenteral therapy
06:31
in certain clinical situations.
06:33
It is very important to remember
06:34
to screen for other sexually
06:36
transmitted diseases in patients
06:38
diagnosed with PID,
06:39
and their partners.
06:40
06:43
Here are my key references.
06:44
06:47
Here are acknowledgements.
06:48
06:52
Thank you.