Duration 10:04
Menopause
Liang A
Clinical Cases Applicability: menopausal symptoms (hot flashes, atrophy), osteopenia/osteoporosis, menopausal hormone, premature ovarian insufficiency
Learning Objectives:
1. Understand the physiologic changes in estrogen levels and the hypothalamic-pituitary-ovarian axis in menopause
2. Describe the pathophysiology of the various symptoms of peri-menopause/menopause
3. Discuss treatment options for the symptoms of menopause
What hormonal changes occur in perimenopause and menopause (defined as 1 year of cessation of menstruation)? How does this affect the HPO axis?
Perimenopause: Reduced ability of aging follicles to secrete inhibin (produced in granulosa cells of developing follicles) lack of negative feedback from ↓inhibin ↑FSH↑ovarian follicular response maintain overall estrogen levels
Menopause: Ovarian follicles undergo accelerated loss until depletion of follicles ↓ovarian steroid hormone (estrogen, progesterone) release lack of negative feedback ↑ GnRH release↑ circulating FSH and LH
What are common symptoms of menopause? What is the pathophysiology?
Abnormal uterine bleeding– increased anovulatory cycles; With ↑unopposed estrogen levels increasing risk for developing hyperplasia/carcinoma
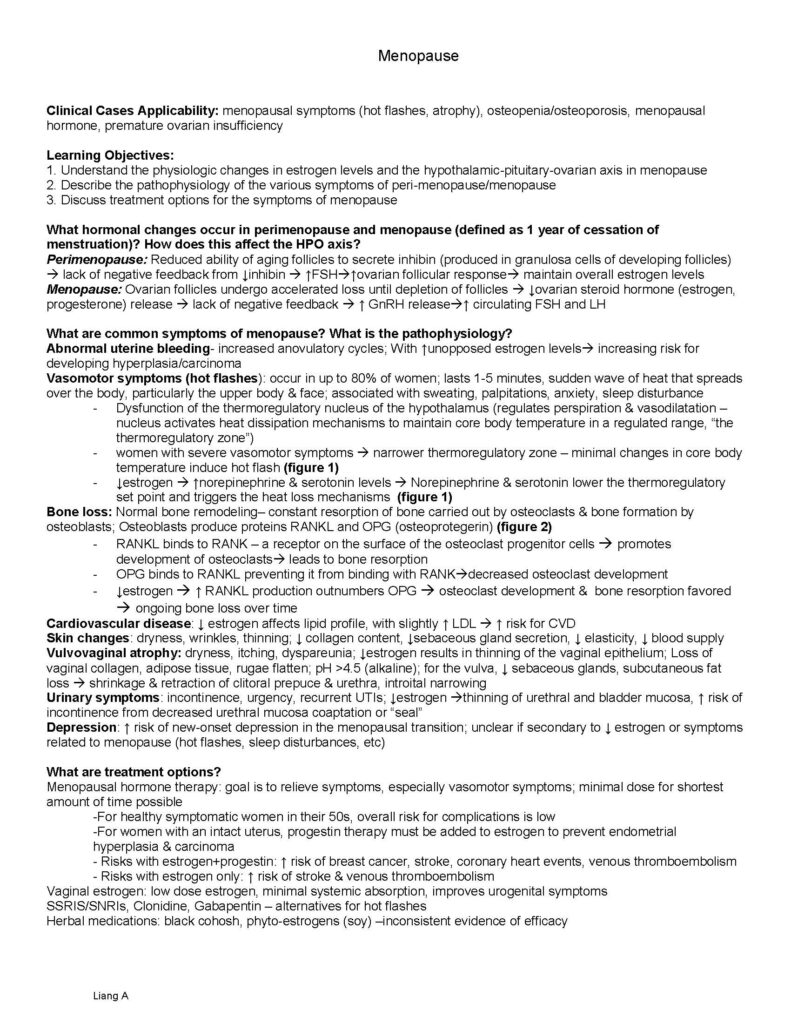
Vasomotor symptoms (hot flashes): occur in up to 80% of women; lasts 1-5 minutes, sudden wave of heat that spreads over the body, particularly the upper body & face; associated with sweating, palpitations, anxiety, sleep disturbance
– Dysfunction of the thermoregulatory nucleus of the hypothalamus (regulates perspiration & vasodilatation –nucleus activates heat dissipation mechanisms to maintain core body temperature in a regulated range, “the thermoregulatory zone”)
– women with severe vasomotor symptoms narrower thermoregulatory zone – minimal changes in core body temperature induce hot flash (figure 1)
– ↓estrogen ↑norepinephrine & serotonin levels Norepinephrine & serotonin lower the thermoregulatory set point and triggers the heat loss mechanisms (figure 1)
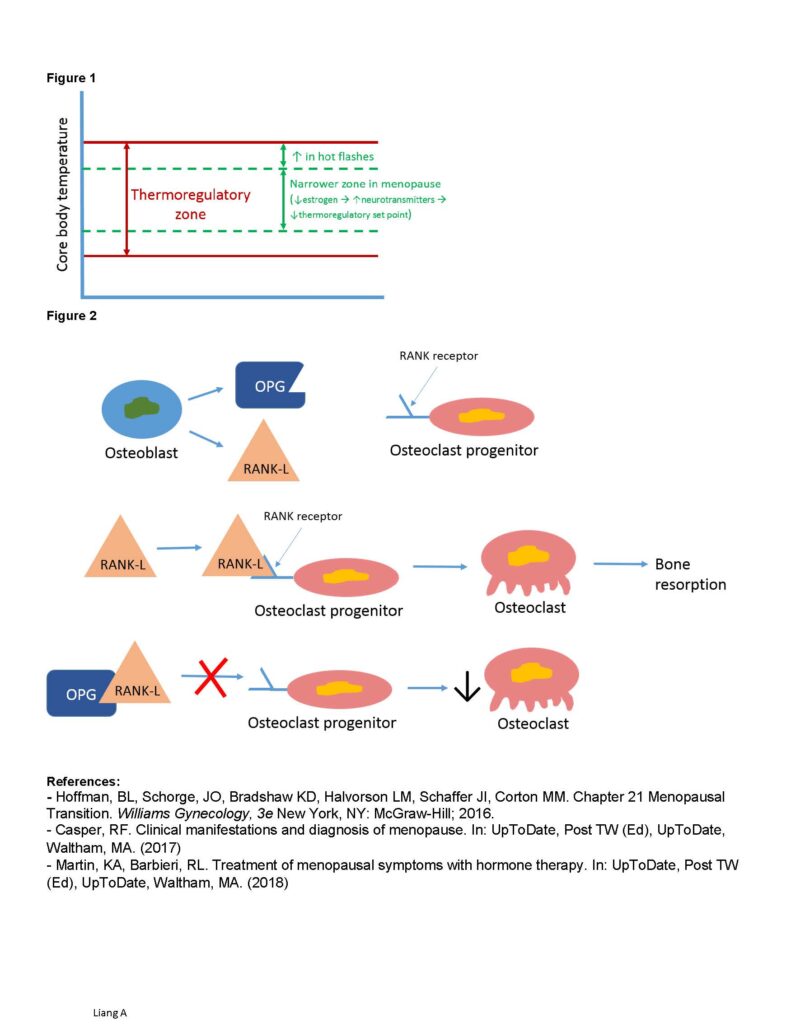
Bone loss: Normal bone remodeling– constant resorption of bone carried out by osteoclasts & bone formation by osteoblasts; Osteoblasts produce proteins RANKL and OPG (osteoprotegerin) (figure 2)
– RANKL binds to RANK – a receptor on the surface of the osteoclast progenitor cells promotes development of osteoclasts leads to bone resorption
– OPG binds to RANKL preventing it from binding with RANKdecreased osteoclast development
– ↓estrogen ↑ RANKL production outnumbers OPG osteoclast development & bone resorption favored ongoing bone loss over time
Cardiovascular disease: ↓ estrogen affects lipid profile, with slightly ↑ LDL ↑ risk for CVD
Skin changes: dryness, wrinkles, thinning; ↓ collagen content, ↓sebaceous gland secretion, ↓ elasticity, ↓ blood supply
Vulvovaginal atrophy: dryness, itching, dyspareunia; ↓estrogen results in thinning of the vaginal epithelium; Loss of vaginal collagen, adipose tissue, rugae flatten; pH >4.5 (alkaline); for the vulva, ↓ sebaceous glands, subcutaneous fat loss shrinkage & retraction of clitoral prepuce & urethra, introital narrowing
Urinary symptoms: incontinence, urgency, recurrent UTIs; ↓estrogen thinning of urethral and bladder mucosa, ↑ risk of incontinence from decreased urethral mucosa coaptation or “seal”
Depression: ↑ risk of new-onset depression in the menopausal transition; unclear if secondary to ↓ estrogen or symptoms related to menopause (hot flashes, sleep disturbances, etc)
What are treatment options?
Menopausal hormone therapy: goal is to relieve symptoms, especially vasomotor symptoms; minimal dose for shortest amount of time possible
-For healthy symptomatic women in their 50s, overall risk for complications is low
-For women with an intact uterus, progestin therapy must be added to estrogen to prevent endometrial hyperplasia & carcinoma
– Risks with estrogen+progestin: ↑ risk of breast cancer, stroke, coronary heart events, venous thromboembolism
– Risks with estrogen only: ↑ risk of stroke & venous thromboembolism
Vaginal estrogen: low dose estrogen, minimal systemic absorption, improves urogenital symptoms
SSRIS/SNRIs, Clonidine, Gabapentin – alternatives for hot flashes
Herbal medications: black cohosh, phyto-estrogens (soy) –inconsistent evidence of efficacy Liang A
Figure 1
Figure 2
References:
– Hoffman, BL, Schorge, JO, Bradshaw KD, Halvorson LM, Schaffer JI, Corton MM. Chapter 21 Menopausal Transition. Williams Gynecology, 3e New York, NY: McGraw-Hill; 2016.
– Casper, RF. Clinical manifestations and diagnosis of menopause. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA. (2017)
– Martin, KA, Barbieri, RL. Treatment of menopausal symptoms with hormone therapy. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA. (2018)
Duration 5:16
00:09
I’m Maureen Leupold. I’m a retired biology professor. I’ve been retired
00:14
about three years and Steve and I will have been married for forty five years
00:19
this year. We have one daughter and a granddaughter. My daughter was adopted
00:24
from Paraguay, so it is approximately 11 years ago I was still teaching and I
00:30
started to have an irregular period but then I missed the period for long enough
00:37
to think could I be pregnant? And I mean I’m in my 50s this is crazy but you know
00:43
I mentioned my daughter was adopted so I’m in I’m a parent but I never was
00:46
pregnant so how would I know. So I had the test and no I wasn’t. I was beginning
00:51
menopause and I laugh now but it wasn’t funny at the time. Then I started
00:57
with the hot flashes and you know I think they probably started at night. My
01:01
husband was getting kind of annoyed because I didn’t go easy into the hot
01:06
flashes at night I’d throw the covers off you know and the heat would be up
01:11
and then of course you’d get chilly and you’d put him back on but that was when
01:15
I started to try some of the herbal supplements so I think I tried three
01:19
different things like black cohosh and you know a couple of the blends that
01:23
you’ll find on the internet and I gave him I gave everybody about a month trial
01:28
to see is it going to work and nothing really worked and the worst of it was
01:32
standing in front of students and at the time I was you know I was teaching a
01:38
high school class on the college campus along with you know the young adults but
01:42
you know standing in front of a group of teenagers and just have your face turn
01:47
beet beet red and start to sweat and you know try to carry on it did just it was
01:53
difficult so I finally went to my physician and requested to go on the
01:59
hormone replacement therapy and I stayed on that for quite a while.
02:03
It was always standard protocol to warn a woman that there could be some risks
02:08
associated with going on hormone replacement therapy so I know that I got
02:13
the standard story about what to be concerned about
02:18
on going on that. I went on the hormone replacement therapy in the summertime and
02:24
I was more-or-less getting ready to go back to school in the fall and not have these
02:28
symptoms and you know by the time school started I was good and it seemed like
02:33
you know the miracle drug being able to just eliminate hot flashes. It was
02:38
amazing. I did try to go off it. I was probably on it maybe five six years and
02:45
I just decided I’m just going to stop this and I went cold turkey and that was
02:49
a very large mistake so I went back on it again.
02:54
In total, I was on it for eight years. I finally went off of it last summer so it
02:59
was around July and probably immediately gained about ten pounds you know over
03:05
the course of a month or two which is very frustrating because I didn’t really
03:08
change anything. I’ve gotten it somewhat under control since but the hot flashes
03:15
started up again the hot flashes in the lack of sleep
03:18
that’s probably the very worst thing that happens. I really walked into a
03:23
completely unprepared you know and in how silly that I thought I could have
03:27
been pregnant when it was really the start of menopause you know when you
03:30
think about it. But it’s very frustrating that I didn’t feel like I knew what was
03:37
about to hit. Even today I want to know is why hasn’t there been more research
03:42
into this? I just wonder are there large studies on other ways to help ease the
03:49
symptoms of menopause especially hot flashes so given that I still have
03:55
symptoms I’m still trying various things in order to ease especially the hot
04:00
flashes. I have this little fan blowing on me all night long. Very helpful with
04:05
the hot flashes. I have a little mister in order to get a little coolness on my
04:13
face. I bought these sports towels and you
04:17
wet this and wring it out and it stays cooler than a normal wash cloth.
04:21
I’m still trying things over-the-counter to see if there’s any help to be had.
04:27
Magnesium supplements were one thing. I am currently trying this paradin
04:35
C compound it’s a vitamin C compound and jury’s still out on that because I’ve
04:40
only started that a couple weeks ago and then some of the other things that I’ve
04:43
tried over time. In the end I’m back to where I started in so many ways because
04:49
I still have hot flashes and I’m very affected by the lack of sleep that they
04:54
cause.
04:59
(Music)
05:02
BlueCross BlueShield is a proud sponsor of Second Opinion
05:06
live fearless. Second Opinion is produced in conjunction with UR medicine
05:11
part of University of Rochester Medical Center Rochester New York