f. The scrub is considered a “sterile” person.
(1) The “sterile” personnel gowns and gloves without touching the outside of the gown or gloves with his bare hands.
(a) If a “sterile” team member’s glove is punctured during an operation, the glove is to be changed at once.
(b) If the glove is pricked by a needle or an instrument, the needle or instrument is discarded from the sterile field. Notify the circulator of the needle’s whereabouts.
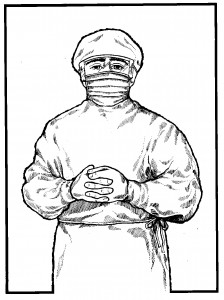
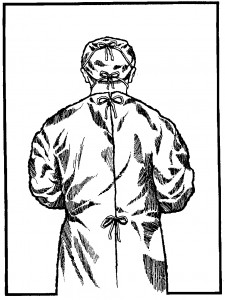
(2) The parts of a surgical gown (see Figures 1-2 and 1-3) considered sterile are the sleeves (except for the axillary area) and the front of the gown from table level to a few inches below the neck opening.
(3) The scrub sets basins or glasses to be filled at the edge of the sterile table opposite where he stands. The circulator stands near the edge of the table to fill them.

(4) A “sterile” team member turns away from the sterile field to have perspiration mopped from his brow.
(5) The scrub drapes the part of an unsterile table nearest himself first.
(6) A “sterile” person should keep his hands in sight and at waist level or above.
(7) A “sterile” person should keep his hands away from his face and his elbows close to his sides. He should never fold his arms because his gown may be moist with perspiration in the axillary (under arms) region; thus, his gloves would become contaminated. When a “sterile” person stands on a footstool, the lower part of his gown should not brush the sterile table. (Common sense determines sterile parts of a gown worn by tall and short members in relation to their waists and the tops of sterile tables.)
(8) “Sterile” team members should keep their contact with sterile areas to a minimum.
(a) “Sterile” team members should not lean on the sterile tables or on the draped patient.
(b) The scrub should keep the large instrument table (back table) and the Mayo stand far enough away that the gowns of other “sterile” team members do not brush them.
(9) “Sterile” team members keep well within the sterile area. The scrub should allow a wide margin of safety when passing unsterile areas. He and all other “sterile” team members should observe the following practices.
(a) “Sterile” team members should stand back at a safe distance from the operating table while draping the patient.
(b) “Sterile” team members should pass each other back to back.
(c) A “sterile” team member should turn his back to an “unsterile” person or area when passing.
(d) A “sterile” team member should face a sterile area when passing.
(e) “Sterile” team members should stay near the sterile table. They should not wander about the room nor go out into the corridor.
(f) When used items or soiled sponges are placed into a basin and maintained on the sterile field, the inside of the basin is contaminated. Handle such a basin by the outside only.
g. The circulator is considered the “unsterile” member of the surgical team.
(1) An “unsterile” team member should never crowd past a “sterile” team member or field. Allow sufficient space between you and the sterile field or between you and gowned individuals when passing them.
(a) “Unsterile” team members should keep away from sterile areas. “Unsterile” persons should allow a wide margin of safety when passing sterile areas.
(b) “Unsterile” persons should face a sterile area when passing it to be sure you have not touched it.
(c) In addition, “unsterile” persons should not go within the sterile “circle” or between two sterile fields.
(d) When passing behind a gowned team member, always notify him to avoid possible contamination of his sterile attire if he should turn or move back and brush you.
(2) The circulator stands at a safe distance from the sterile field when adjusting the light over it.
(a) Never reach across a sterile field. Stand outside the sterile field and hold the extra supplies needed; allow the scrub to reach for them. Do not enter the sterile field to perform any duties.
(b) When moving a sterile table, grasp the table legs well below the tabletop and underneath the sterile drapes.
(c) The circulator “flips” the sterile suture material onto back table (see Figure 1-4).
h. The edge of a cover that encloses sterile contents is not considered sterile.
Such covers include the edges of wrappers on sterile packages, the caps on solution bottles, and test tube covers. No definite line separates the sterile from the unsterile area at the edge of the cover; therefore, the edge is considered unsterile.
(1) The scrub should lift contents from packages by reaching for them with the arm straight out and lifting the items straight up — with the elbow held high throughout the procedure.
(2) The circulator lifts the cap from a solution bottle so that the edge of the cap never touches the lip. Caps are not replaced. The entire contents are dispensed and any excess solution is discarded.

i. Sterile areas should be protected from moisture because a moist item may become contaminated.
When moisture soaks through a sterile area to an unsterile one, or vice versa, a means of transporting infectious organisms to the sterile area is provided. Therefore, the OR specialist should observe the following rules of practice.
(1) Sterile packages should be laid on dry areas.
(2) If any portion of a sterile package becomes damp or wet, the entire package should be discarded.
(3) If a sterile package falls on the floor, it is considered unsterile.
(4) Linen packages from the sterilizer should be permitted to cool before being stored on shelves. This procedure prevents their becoming damp from steam condensation when placed on a cool shelf.
(5) Sterile drapes should be placed on a dry surface. (Thus, time should be allowed for the prep solution used to paint the patient’s skin to dry before draping is begun.)
(6) During surgery, if a solution soaks through a sterile area from an unsterile one or through an unsterile area from a sterile one, the wet area should be covered with another sterile drape.
