The scrub should anticipate the needs of the surgeons and have instruments, sponges, sutures, and other equipment ready for use.
The usual procedures are as follows.
a. Hand the scalpel used to incise the skin (skin scalpel) to the surgeon. An alternate method of handing a scalpel is to place it on a hand towel or in an emesis basin. This is referred to as the “no touch” technique. Some local policies mandate this method because it reduces the likelihood of puncturing a glove with the scalpel blade.
b. After the skin incision is made, put the skin scalpel into a basin and remove it from the operative field onto the back table or cover the blade with a suture package.
The blade of this scalpel is considered contaminated because the skin cannot be made sterile. The scalpel is to remain where you have placed it unless it is needed for enlarging the incision or for making stab wounds for drainage later during the case.
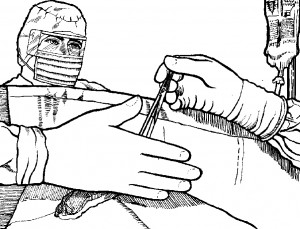
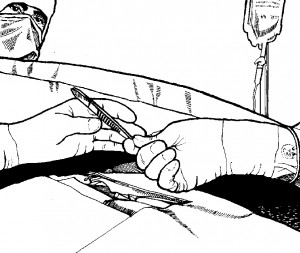
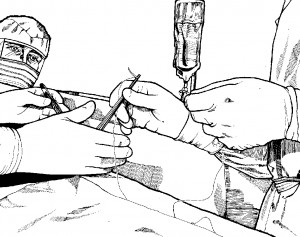
c. Pass instruments and supplies to the surgeon as he needs them; handing each instrument in the position that the surgeon will use it and in such a way that he can grasp it easily. There is to be NO hand contact when handing instruments (see Figures 4-3, 4-4, and 4-5).
d. Remove used supplies from the operative field. Keep the Mayo tray and the back table neat and orderly at all times. Keep the sterile field clean and dry.
e. Keep instruments free of blood with a moist sponge.
f. Clear the operative field of all loose sponges when the surgeon is ready to open the peritoneum. Once the peritoneum is open, use only laparotomy tapes and sponges on forceps.
g. Hand a threaded suture in a needle holder with the needle positioned so that the surgeon can use it without having to shift the instrument.
When you pass the needle holder, hold the end of the longer strand of suture in your other hand to keep it out of the surgeon’s way and to prevent it from dragging over the operative area.
h. Keep a mental count of the suture needles.
Do not allow needles to lie loose on either the operative area or the Mayo table; they should be clamped in a holder. Make sure that you receive a needle holder and a whole needle from the surgeon in exchange for another. If part of a needle has been broken off, report this to the surgeon immediately so that he may take appropriate measures.
i. Pass the peritoneal suture to the surgeon when he is ready to start closure of the wound.
At this point in the procedure, a sponge and sharps count is required. Again, both the scrub and an R.N. must see each sponge. The sponges in the various areas are counted separately (those discarded, those on the sterile tables, and those in the operative field) and then added to obtain the total count. The sequence used in the sponge count is: start with sponges around the incision; then sponges on the Mayo tray; then sponges on the back table; and, finally, the discarded sponges. The procedure is as follows.
(1) The circulator uses forceps to point to each discarded sponge.
(2) You are to handle the sponges remaining on the back table, separating each as it is counted so that both you and the circulator see every sponge.
(3) The surgeon may assist in counting the sponges remaining in the operative field.
(4) The counts are added and should total the number recorded for the initial count plus any that were opened during the case.
(5) You are to report the result of the sponge count to the surgeon. If the count is correct, he will proceed with closure of the wound. If the count is incorrect, all sponges are to be recounted at once. The circulator is to check the kick bucket and the floor. He will often need to don rubber gloves to see that all sponges are separated. The surgeon may assist in recounting sponges in the operative area. You are to check the instrument tables.
(6) If the count remains incorrect after the recount, the operating room supervisor is notified and normally assists with another recount. An X-ray of the operative area may be ordered. If so, it will be taken with portable X-ray equipment while the patient is still on the operating table.
(7) A sharps count is done at the same time and in the same manner as the sponge count. An instrument count is done with the first closing sponge count.
j. After the sponge, sharps, and instrument counts are completed, remove the instruments that are not needed from the Mayo tray and place the material needed for closing the wound on the tray.
k. Pass the necessary sutures to the surgeon, making sure that you receive intact each needle used by the surgeon (see paragraph h above). An X-ray may be necessary to locate a lost needle. While the surgeon is suturing the wound, you are to begin unclamping the instruments and placing them into solution in one of the basins in the basin stand.
l. Prepare the wound dressing during the closure.
m. When the surgeon finishes closing the skin, wet a sponge and wipe around the incision to remove the blood.
n. Hand the wound dressing to the surgeon.
