a. Each type of operating room procedure requires different kinds and numbers of sponges, needles, and instruments.
Each of these items is a foreign object that could cause unnecessary harm or death should it be left inside the patient. To protect the patient, these items are counted before and after use. A counting procedure is a method of accounting for items put on the sterile table for use during a surgical procedure. The counting procedure may differ at various hospitals, but the count itself is mandatory. This subcourse will focus on sponge counts.
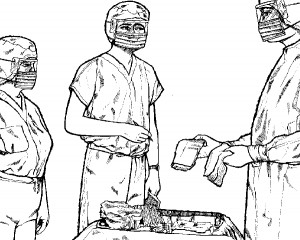
Figure 3-23. Circulator passing supplies to the scrub.b. The scrub will count the sponges with the circulating RN at the first opportunity. An RN must witness the count. A sponge count is necessary for surgical procedures when the depth or the location of the wound may allow a sponge to be left undetected in the wound. Such procedures include laparotomies (operations within the abdominal cavity), surgical procedures within the chest cavity, extra peritoneal operations such as kidney surgery, deep vaginal procedures, and operations on the hip and others. Points to be remembered and observed by both the scrub and the circulator during the sponge count are given below.
NOTE: Only radiopaque (X-ray detectable) sponges are to be used during surgery. Since the prep sponges are not radiopaque, they are to be used only for the prep. Prep sponges are not to be removed from the room. The circulator will put them in a place apart from the sponges that are counted.
(1) Counted sponges are grouped according to type and then counted. Neither sponges, nor linen, nor trash may be removed from the room once the sponges have been counted.
(2) There should be no interruptions during the count. If either the scrub or the circulator loses count, they are to recount.
(3) The scrub should slightly separate the sponges to make sure all sponges are counted (Figure 3-24).
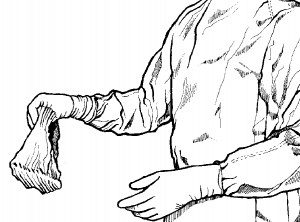
(4) Sponges are to be counted at the same time by the scrub and the registered nurse. Each sponge is to be separated from the others as it is counted (see Figure 3-25). Both the specialist and the RN must see every sponge and must see the radiopaque marking on each sponge. If all are not in agreement on the count, the count must be repeated.
(5) If the number of sponges in a new pack is incorrect, the entire pack must be removed from the room by the circulator and a new pack will be opened. The number of sponges in a pack will vary with the type of sponge. A standardized count routine is established in each hospital to help avoid a possibility of error. You must learn the local policy and follow it with meticulous attention to detail.
(6) When the scrub and RN are in agreement, the count is recorded immediately by the RN. Local policy will prescribe the manner in which the count is recorded. Most installations use a count “board.”
(7) If additional sponges are needed during the case, they are counted and recorded in the same manner and added to the initial sponge count.
(8) Sponges are kept away from articles that might drag a sponge into the wound unknowingly.
(9) Kitner sponges (small rolls of heavy cotton tape and used with a forceps) are kept in a medicine glass. Dirty ones are discarded into another medicine glass to facilitate counting them.
(10) Lap sponges (sponges with a loop of twilled taped sewed on one corner) are unfolded as they are counted and placed on the back table.
(11) Stick sponges (small gauze sponges used with a forceps) are placed in an empty emesis basin and placed on the back table.
(12) After the sponge count is completed, place a few of the appropriate sponges on the Mayo tray for the initial incision.

