a. The circulator should check the operating room schedule the day before surgery for any changes that may have been made. The operating room specialist should be in the assigned room in plenty of time to prepare for the surgical procedure.
Centralized Materiel Service should be notified of any special equipment and/or instruments that may be needed for the case that are not readily available.
b. Personal cleanliness is extremely important for the operating room specialist.
Before performing the duties described in the following paragraphs for preparation of the operating room, the circulator should wash his hands thoroughly and don a surgical hat. The surgical cap must cover the hair completely to prevent possible contamination of the sterile area by falling hair or dandruff. He should then don a clean, cotton scrub suit before entering the semi-restricted areas of the surgical suite.
Before entering a restricted area, the OR specialist must don a surgical mask per local SOP. The mask protects the patient from bacteria exhaled by operating room personnel. The mask must fit snugly around the nose and mouth to filter the air through it rather than around the sides of the mask. The mask should be changed whenever it becomes damp and after each procedure.
The correct procedures for donning scrub suit, surgical hat, shoe covers, and surgical mask are provided in detail in Subcourse MD0933, Scrub, Gown, and Glove Procedures, which you should have studied prior to this subcourse. Now you are ready to prepare the operating room for surgery.
c. Damp dust the operating room unless this has already been done by personnel on the previous shift.
Concurrent with dusting, check equipment, arrange furniture, and restock supplies. After damp dusting with a cloth soaked in disinfectant solution prescribed by local policy, wet vacuum the floor using a disinfectant prescribed by local policy. Dry dusting and mopping is never done in the operating room because it raises dust that contains bacteria.
(1) Damp dusting should be done before the first scheduled incision time of the day.
(2) Establish and follow a definite order when damp dusting furniture. Start with the tallest equipment and work down since this method helps the settling of airborne microorganisms. Damp dust the operating room overhead light first, then the operating table. Work from the center of the room to the perimeter (outer limits) and from the tallest item to the lowest. If you are called from the room, leave the damp dusting cloth on the item being dusted; this will serve as the starting point when resuming dusting duties.
(3) As the damp dusting is accomplished, set up the equipment and check each item for proper functioning. This will save time and energy. This includes such things as:
(a) Switch on the overhead light to ensure proper functioning.
(b) Check the operating table for proper working order.
(c) Check the suction machine, the electrosurgical unit, and other pieces of equipment in the operating room whether or not they are to be used.
(d) Line the kick buckets with plastic bags.
(e) Check the supply cabinets for stock. Restock, if necessary.
(4) Consult with the scrub on the arrangement of the furniture for the surgical procedure. In general, the area chosen for the sterile setup should be away from doorways and traffic. It should be in the most closed-in area away from the cabinets that are to be opened during the setup. As damp dusting continues, arrange the furniture for the sterile setup so that the scrub can work within the sterile field and the circulator can work outside the field.
d. Check with the scrub for any special equipment he may need for the case.
e. If the instruments were not wrapped and sterilized on the preceding shift, ensure that instrument sets are placed in the autoclave.
f. Check that all equipment needed to position the patient is in the room. If not, get the necessary equipment.
g. Discuss with the scrub the sterile supplies needed for the case (be sure to discuss the kind and amount of sutures needed) and then bring the supplies into the room. The surgeon’s preference card will list the types and sizes of sutures needed for the procedure.
h. Place sterile goods on the tables or stands where they will be used to avoid having to move them from one place to another. You should place the various sterile items as indicated in (1) through (6) below.
(1) The linen or drape pack on the large instrument table (backtable).
(2) The gown pack on the prep table.
(3) The Mayo tray on the Mayo stand.
(4) The sterile basin set into the ring stand.
(5) The prep set placed on the prep table. Only after the scrub dons the gown and the wrapper is removed,
(6) The instrument set on a ring stand or table.
i. Put sterile packages that the scrub will not need immediately (such as suction tubing and culture tubes) on the utility table and open them after the scrub has prepared a space for them. You may also place on the utility tables supplies needed from the sterile supply cabinets such as knife blades, needles, etc.
j. Do not place sterile supplies on the operating table nor on the anesthetist’s equipment (the anesthesia apparatus and the anesthetist’s table) because these areas are for the use by the anesthetist only.
k. Open the sterile supplies. Before any sterile supplies are opened, however, the integrity of every package is checked for tears, punctures, watermarks, expiration date, and the sterilization indicator. Tears, punctures, and watermarks on a sterile pack indicate that the supplies are unsafe to use. The sterilization indicator shows whether the pack has been through the sterilization process. The date of expiration will tell you whether it is too old for safe use. If the package is in any way compromised, it must be discarded and a new pack secured.
l. Open the packs and sets in the order in which the scrub will need them. Open the sterile gown first; the scrub will need this immediately upon entering the room.
(1) Remove the tape from the packages, unwrap the item, and check the indicator tape to ensure item has been through the sterilization process. If the indicator tape shows no or incomplete sterilization process, discard the package and secure a new one.
(2) After opening the pack containing the scrub’s gown, open the basin set, the linen pack, the prep set ,and the instrument set.
m. All sterile wrappers are to be removed in the same general manner. Open the wrapper so that your hand and arm do not pass over any part of the inside of the wrapper that has been exposed.
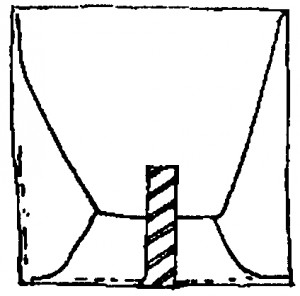
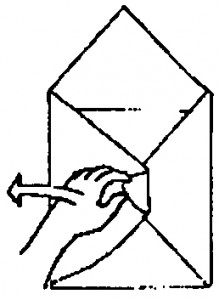
(1) Position the package so that the flaps are on top (Figure 3-1).
(2) Using one hand lift the distal flap up and away from the package (Figure 3-2).
(3) Open the left flap (Figure 3-3).
(4) Open the right flap (Figure 3-4).
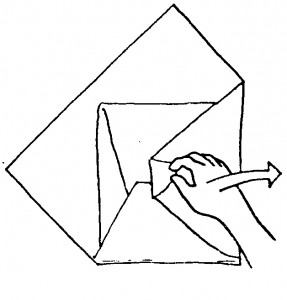
(5) Open the near flap (Figure 3-5).
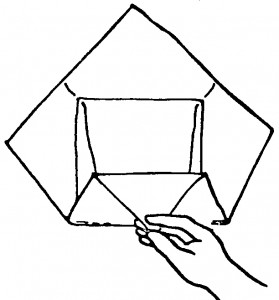
n. Larger sterile supplies can be opened using the wrappers to form a sterile field and are to be opened in the following manner.
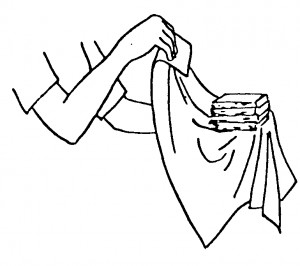
(1) With hands on the outside of each wrapper in a folded cuff, always lift the wrapper toward you to avoid contaminating the contents of the pack (see Figure 3-6). The area touched by you under the cuff falls below table level and the inside of the wrapper remains sterile.
(2) Walk around the table as you remove each portion of the wrapper. Do not reach over the inside of the sterile table cover or the contents of the pack.
(3) Stand at arms length from the sterile pack as you lift the wrappers (see Figure 3-7). If a sterile pack falls to the floor, discard it, as it has now become contaminated.

(4) Check the sterilization indicator. If the sterilization indicator in the pack is acceptable, the circulator continues. If the indicator is not acceptable, the pack is discarded and a new pack is opened.
(5) The inside of the wrapper can now be used as a sterile field. The object that was wrapped (such as the scrub’s gown, double basin set or back table surgical pack) is now located within a sterile field.
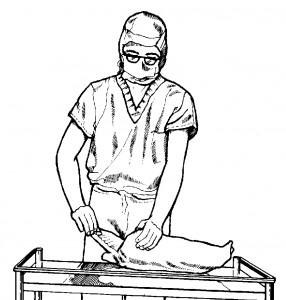
o. Smaller sterile supplies are to be opened and added to the sterile field in the following manner:
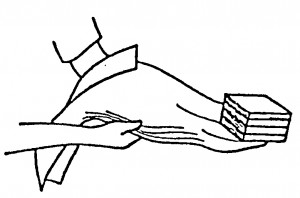
(1) Hold the sterile package in one hand with the flaps up. This is done away from the sterile field.
(2) Grasp the outside edges of the sterile wrapper with your free hand. This protects the sterility of package contents.
(3) Unwrap the sterile package (Figure 3-8). Be careful not to contaminate the inside of the wrapper or the sterile object.
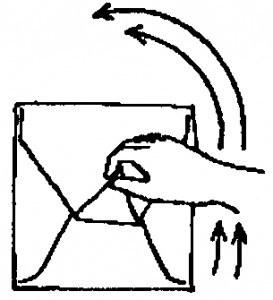
(4) Hold edges of sterile wrapper back around your wrist (Figure 3-9) so they will not accidentally drag across sterile field and so the hand supporting the sterile object is enclosed by the wrapper.
(5) Drop small sterile items directly into the sterile field.