Lymphadenopathy
|
Lymph nodes are lymphoid organs responsible for the processing of antigens, and may become activated by a variety of processes. Antigenic stimulation may result in nodes enlarging to 10 -15 times the normal size within a matter of days. Lymphadenopathy is a manifestation of either stimulation of nodal B or T lymphocytes by antigens or infiltration of the node(s) by a neoplastic process. Lymphadenopathy may be a reflection of a wide variety of pathologic processes, ranging from mild, self-limited viral infections to life-threatening malignant processes. The key task in the evaluation of the patient with lymphadenopathy is to decide whether the underlying process is benign and can be observed over time, or whether adenopathy represents a more serious entity that requires prompt diagnosis and treatment. Often no single piece of the history or physical is sufficient to make this distinction. However, when combining a number of these clues, a suggested diagnosis may assist in the clinical work-up. 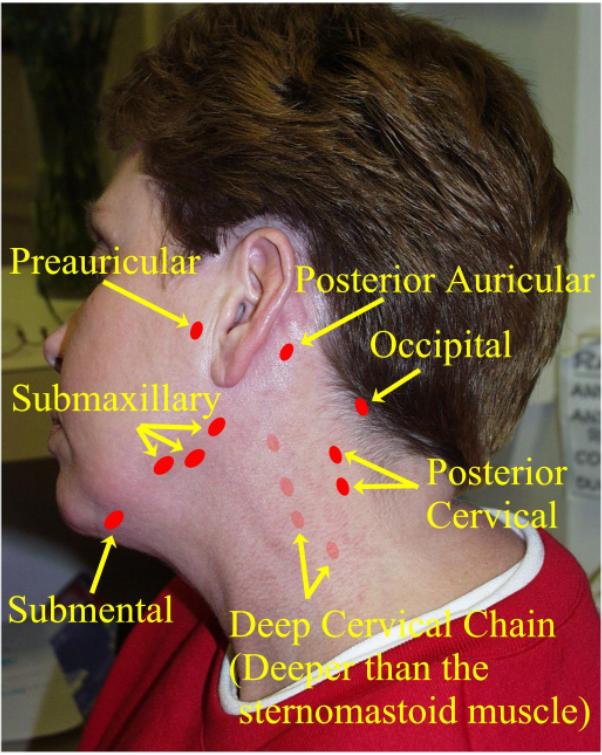
Some useful indicators that will help lead to diagnosis are as follows:
Viral: Epstein-Barr virus, cytomegalovirus, HIV, rubella, hepatitis B Bacterial: Toxoplasmosis, syphilis, tuberculosis, atypical mycobacterial infections, brucellosis, tularemia, leptospirosis
May include all of the above plus: streptococcal/staphylococcal infections, cat-scratch disease, lymphogranuloma venereum, herpes simplex virus, dermatopathic lymphadenitis, metastatic cancers, and sarcoid. Hilar Sarcoid, histoplasmosis, coccidiomycosis, lymphoma, tuberculosis, bronchogenic carcinoma The above list, while clearly not exhaustive, may still appear somewhat daunting when
one is faced with evaluation of the patient with lymphadenopathy. Fortunately, a
relatively small number of disease processes make up the bulk of patients seen with
adenopathy. By far the most common cause of generalized lymphadenopathy in the younger
active duty population is the infectious mononucleosis syndrome, or "mono."
Typically caused by the Epstein-Barr virus, adenopathy is most prominent in the cervical
distribution, and usually accompanied by pharyngitis (usually exudative), fever, fatigue,
and frequently splenomegaly and elevated liver-associated enzymes. Disease is suggested by
atypical lymphocytosis on peripheral smear, and essentially ruled-in by a positive
Monospot test, with the caveat that the Monospot may be negative initially but positive on
repeat testing. It is important to realize that cytomegalovirus and toxoplasmosis can
present in identical fashion (although pharyngitis tends to be a less prominent
complaint), and serologies for these diseases should be sent in heterophile-negative
infectious mono syndromes. HIV infection should always be kept in mind when faced with a sexually active patient
with lymphadenopathy, in particular the acute seroconverting illness as previously
mentioned. This syndrome occurs on average 6 weeks after exposure in about half of all
individuals infected with HIV. Symptoms often consist of pharyngitis, fever, diarrhea,
maculopapular, truncal rash, and mucocutaneous ulcers in addition to lymphadenopathy. Of
critical importance, these individuals will typically test negative for HIV at the time of
illness, and so it is essential to send a p24 antigen if possible, and to retest for HIV
44 weeks later. As alluded to earlier, syphilis as well as hepatitis B need to be kept in mind as
possibilities in the active duty population. Localized adenopathy in most cases will be
caused by a local strep or staph infection, but cat scratch disease should be kept in
mind, particularly if there is a history of recent exposure to cats. Finally, although
malignancies are fortunately not common in the active duty population, they do occur
regularly, and should always be kept in mind in the differential of both localized and
general lymphadenopathy. Bilateral hilar adenopathy in an asymptomatic individual, especially if
African-American, strongly points to sarcoid as the diagnosis. Bilateral hilar adenopathy
in a symptomatic patient, or the presence of enlarged unilateral hilar nodes, raises the
possibility of lymphoma, bronchogenic lung cancer, or tuberculosis. Laboratory studies may be very useful in the investigation of
lymphadenopathy. A CBC with differential should always be performed if any doubt exists as
to the etiology. A left shift suggests a bacterial process, atypical lymphocytes point
toward infectious mononucleosis, or other viral diseases, and eosinophils raise the
possibility of a drug reaction. Other studies that may be useful include syphilis
serologies, Monospot, hepatitis
serologies, toxoplasmosis
titer, LDH (nonspecific,
but substantial elevation suggests lymphoma), ANA, rheumatoid factor, and PPD. A chest
x-ray may be useful also. With peripheral lymphadenopathy and an abnormal chest film there
is a likelihood of a serious systemic illness. If a diagnosis is not apparent after appropriate initial work-up, consideration should
be given to referral of the patient to a higher level of care for further evaluation
and/or a biopsy. While it is difficult to give definite guidelines regarding whom and when
to refer to, certain factors should prompt early referral. These include a history of
fever or night sweats, node(s) greater than 2 centimeters in size, an abnormal CXR,
anemia, and any enlarged supraclavicular node. Unfortunately, even when biopsy is
performed, not infrequently the pathology is non-diagnostic. It is essential to remember
that anywhere from 15 to 25 percent of these patients, when followed over time, will prove
to have a definable cause for their lymphadenopathy. Most often this proves to be
lymphoma, pointing out the importance of continued re-evaluation after a non-diagnostic
biopsy. Written and reviewed by CDR James C. Pile, MC, USN, Department of Infectious
Disease, National Naval |
Preface · Administrative Section · Clinical Section
The
General Medical Officer Manual , NAVMEDPUB 5134, January 1, 2000
Bureau
of Medicine and Surgery, Department of the Navy, 2300 E Street NW, Washington, D.C.,
20372-5300
This web version of The General Medical Officer Manual, NAVMEDPUB 5134 is provided by The Brookside Associates Medical Education Division. It contains original contents from the official US Navy version, but has been reformatted for web access and includes advertising and links that were not present in the original version. This web version has not been approved by the Department of the Navy or the Department of Defense. The presence of any advertising on these pages does not constitute an endorsement of that product or service by either the Department of Defense or the Brookside Associates. The Brookside Associates is a private organization, not affiliated with the United States Department of Defense. All material in this version is unclassified. This formatting © 2006 Medical Education Division, Brookside Associates, Ltd. All rights reserved.
Home · Textbooks and Manuals · Videos · Lectures · Distance Learning · Training · Operational Safety · Search
This website is dedicated to the development and dissemination of medical information that may be useful to those who practice Operational Medicine. This website is privately-held and not connected to any governmental agency. The views expressed here are those of the authors, and unless otherwise noted, do not necessarily reflect the views of
the Brookside Associates, Ltd., any governmental or private organizations. All writings, discussions, and publications on this website are unclassified.
© 2006 Medical Education Division, Brookside Associates, Ltd. All rights reserved
Other Brookside Products